The incisive canal is located on the median plane of the maxilla, posterior to the roots of the central incisor. Although the incisive canal is not considered an anatomic structure that may limit tooth movement, it has recently gained attention regarding the possibilities of surgical invasion and associated complications because of its proximity to the maxillary central incisors. In the 2 illustrated cases, lip protrusion was improved by en-masse bodily retraction of the anterior teeth (>8 mm) using temporary anchorage devices. Three-dimensional cone-beam computed tomography showed that the maxillary incisor roots were approximated to the incisive canal after maximum retraction. One central incisor root was in direct contact with the incisive canal with severe root resorption, but tooth vitality and the overall occlusion were stable in the long term without any sensory dysfunction. The apparent root resorption may be mainly related to the large amounts of anterior retraction and root movement in the 2 patients. However, the anatomic location of the incisive canal and the possibilities of its invasion after tooth movement should be closely monitored when maximum retraction is planned, to prevent potential complications.
Highlights
- •
Maxillary central incisor roots approximated to the incisive canal following maximum retraction.
- •
Apparent root resorption was noted at the incisor root in direct contact with the incisive canal.
- •
Incisive canal-incisor root relationship should be monitored when maximum retraction is planned.
The determination of the position of the maxillary incisors is a key issue in orthodontic diagnosis and treatment planning. In patients with bimaxillary or bialveolar protrusion, premolar extraction followed by maximum retraction of the anterior teeth is required for esthetic improvement. In general, the ideal position of the maxillary incisor is determined based on various soft and hard tissue criteria, and orthodontic tooth movement within the biologic limitations is desirable for a successful treatment outcome with long-term stability.
According to the well-known concept of the “envelope of discrepancy,” the clinical guidelines recommend that the maximum amounts of maxillary incisor retraction and intrusion by orthodontics alone are 7 and 2 mm, respectively. The hard tissue limit for retraction in the maxilla is reportedly the lingual cortical plate; however, it is also commonly accepted that the range of maxillary incisor retraction is greater because of fewer anatomic and physiological constraints than in the mandible.
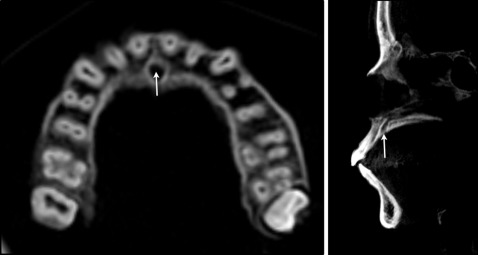
The incisive canal is an anatomic structure located on the median plane of the palatine process of the maxilla, posterior to the roots of the central incisor, surrounded by thick cortical bone ( Fig 1 ). It transmits nasopalatine vessels and nerves, branches of the maxillary division of the trigeminal nerve, and the maxillary artery. Although the incisive canal has not been proposed as an anatomic structure that may limit tooth movement, it has gained attention because of the possibilities of surgical invasion and associated complications such as nonosseointegration or sensory dysfunction owing to its proximity to the maxillary incisor region. Approximation and contact of the mandibular molars to the mandibular canal and the inferior alveolar neurovascular bundle during orthodontic tooth movement have also been reported and in rare incidences were associated with temporary paresthesia of the lower lip.
The following 2 case reports illustrate the contact and approximation of the maxillary central incisor roots to the incisive canal after maximum retraction with temporary anchorage devices.
Case reports
Patient 1
Patient 1 was a 19-year-old woman with chief complaints of lip prominence and protrusion. The intraoral photographs and cephalograms indicated a skeletal Class II malocclusion with a protrusive profile. A panoramic radiograph showed no gross abnormalities. She had no notable medical history ( Fig 2 ).
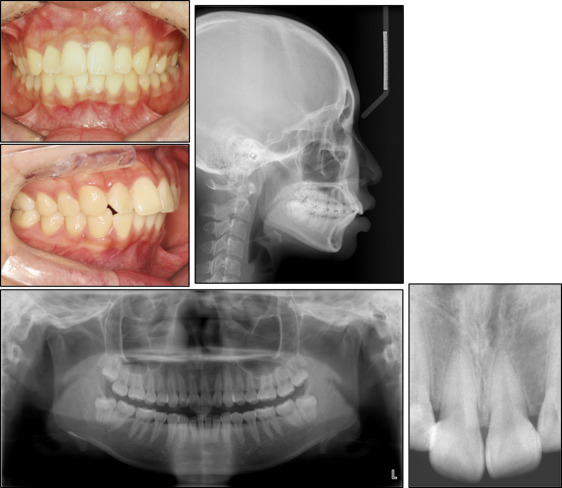
The overall goals of treatment were to improve the protrusive profile and to obtain a Class I occlusion with ideal overjet and overbite. Four first premolars were extracted, and orthodontic treatment was initiated using 0.022-in slot Roth prescription self-ligating brackets (Clippy-C; Tomy International, Tokyo, Japan). In addition, 4 miniscrews (Ortholution, Gyeonggi-do, Korea), one per quadrant, were inserted between the second premolars and the first molars to reinforce anchorage during space closure. We used 150-g nickel-titanium coil springs (Tomy International) and elastomeric modules for anterior retraction via en-masse sliding mechanics. Since the patient lived abroad, she was able to visit the clinic only once every 4 months on average during her vacations.
The duration of the treatment was 24 months. After treatment, her profile was improved with a Class I occlusion and ideal overjet and overbite, and the dental midline was in accordance to the facial midline. Fixed retainers were bonded, and removable retainers were provided for use at night. The patient was fully satisfied with the overall outcome. The cephalometric superimposition indicated absolute retraction of the maxillary incisors through bodily movement and controlled tipping of the mandibular incisors along with intrusion ( Table I ). However, the posttreatment radiographs indicated moderate to severe apical root resorption, especially in the maxillary right central incisor, compared with the neighboring teeth. Interestingly, according to the periapical radiograph, the incisive canal, which was identified as a radiolucent tube-like structure surrounded by a thin radiopaque margin between the central incisor roots, was curved to the right and not to the left, making contact with the right central incisor root and not the left central incisor ( Figs 3-5 ).
| Measurement | Norm | Pretreatment | Posttreatment | Postretention |
|---|---|---|---|---|
| Skeletal (°) | ||||
| SNA | 81.6 ± 3.1 | 76.2 | 74.9 | 74.8 |
| SNB | 79.1 ± 3.0 | 71.1 | 70.8 | 70.9 |
| ANB | 2.4 ± 1.8 | 5.1 | 4.1 | 3.9 |
| FMA | 24.0 ± 5.0 | 26.3 | 23.7 | 25.9 |
| Dental (°) | ||||
| IMPA | 94.0 ± 5.0 | 113.5 | 93.8 | 97.4 |
| U1 to SN | 106.0 ± 5.0 | 104.7 | 92.1 | 97.4 |
| Interincisal angle | 126.0 ± 7.0 | 103.6 | 136.6 | 128.5 |
| Soft tissue (mm) | ||||
| Upper lip E-plane | −1.0 ± 2.0 | 2.7 | −1.4 | −2.4 |
| Lower lip E-plane | 1.0 ± 2.0 | 5.2 | 0.1 | 1.4 |
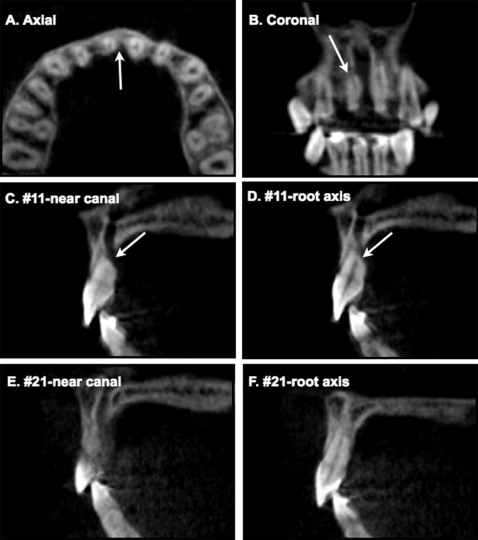
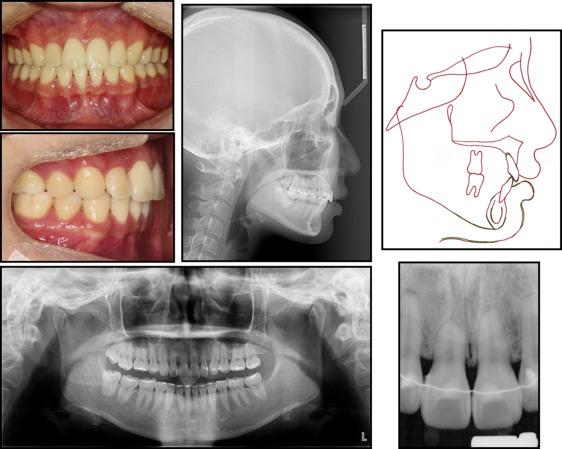
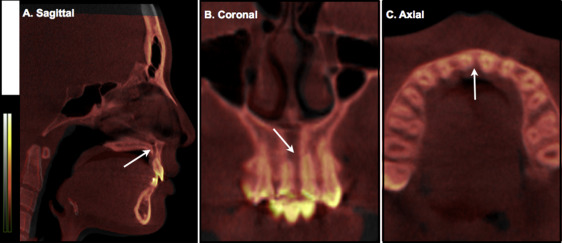
Considering the large amounts of anterior retraction and root movement, and the severity of root resorption at the right central incisor, we performed a cone-beam computed tomography (CBCT) scan (Pax-Zenith3D; Vatech, Seoul, Korea) to further evaluate the 3-dimensional (3D) structural changes, including the amount of alveolar bone surrounding the maxillary incisors. In general, the palatal surface of the maxillary teeth was covered with a thin layer of cortical bone. However, to our surprise, the mesiopalatal surface of the maxillary right central incisor root apex was in contact with the incisive canal ( Fig 4 , A and B ), which was associated with severe root resorption ( Fig 4 , C and D ), whereas the left central incisor was in proximity rather than in contact, showing mild apical root blunting ( Fig 4 , E and F ). Specific symptoms, such as numbness or pain of the teeth or periodontium, were not noted, and the incisors were vital.
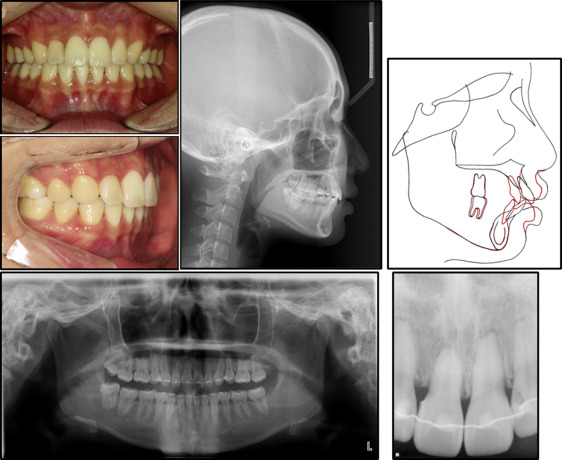
After 30 months, the patient revisited the clinic. Although the maxillary fixed retainer had been detached for approximately a year after debonding and she had stopped using the removable retainers, her occlusion was stable. No detrimental changes in the maxillary incisor’s root were noted. Rather, a periapical radiograph showed that the apical surface had become smoother with even periodontal ligament space. Considering the crown-root ratio of the incisors, new fixed retainers were bonded on the maxillary incisors ( Fig 5 ). To determine whether any changes had taken place with regard to the occlusion and the incisive canal, another CBCT scan was performed at 36 months of retention with the patient’s consent. The 3D CBCT findings obtained immediately after the treatment and those obtained 36 months after treatment were superimposed by automatic voxel-by-voxel registration at the cranial base (OnDemand3D; Cybermed, Seoul, Korea). The 3D superimposition did not indicate any specific changes in the surrounding alveolar bone, the position of the central incisors in contact or approximation with the incisive canal, or the incisive canal itself ( Fig 6 ). No specific symptoms or pain was reported; in general, the probing depth was less than 2 mm, except for the mesiopalatal interproximal gingiva, where the depth was approximately 3 to 4 mm, but it was not associated with bleeding.

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


