Introduction
The purpose of this study was to compare the isolated effects of bonded and conventional spurs on the craniofacial and dentoalveolar complexes of patients in the mixed dentition with anterior open bite.
Methods
The sample included 68 subjects with anterior open bite and Class I malocclusion. Group 1 comprised 20 patients treated with bonded lingual spurs with a mean initial age of 9.31 years (SD, 1.17). Group 2 consisted of 21 patients treated with conventional lingual spurs with a mean initial age of 9.22 years (SD, 1.62). The control group (group 3) consisted of 27 untreated subjects. One-way analysis of variance tests followed by Tukey tests were used for intergroup cephalometric comparisons. After 1 month of treatment, patient acceptance of the spurs was evaluated with a questionnaire.
Results
There were significantly greater overbite increases in the experimental groups than in the control group. The group with bonded lingual spurs showed significantly better acceptance than did the group with conventional lingual spurs during chewing and eating.
Conclusions
The 2 appliances resulted in similar overbite increases during early open-bite treatment. After a week or less of treatment, 92.5% of the children had adjusted to the spurs.
Highlights
- •
Treatment effects and patient acceptance of 2 types of lingual spurs were compared.
- •
Both appliances resulted in similar overbite increases.
- •
After 1 week or less of treatment, 92.5% of the children adjusted to the spurs.
Anterior open bite is a common malocclusion in growing patients. The incidence of anterior open bite varies with age and has a high prevalence (17.7%) in the mixed dentition. The etiology is multifactorial, including oral habits, abnormal size or function of the tongue, oral breathing, vertical growth pattern, and congenital or acquired diseases. Among the most frequent habits are finger sucking, pacifiers, altered labial postures, and tongue habits.
Treatment of an anterior open bite is a great challenge in orthodontics. After treatment, patients can benefit from an improved ability to incise and chew food, and improved esthetics and speech. Several early approaches to treat anterior open bite have been developed. Frequently, early anterior open-bite treatment is performed with fixed and removable palatal cribs and lingual spurs that may be associated with a chincup or high-pull headgear in patients with a vertical facial pattern. Although many treatment modalities are available, the effectiveness and the stability after treatment are still critical issues because evidence on the long-term stability of these options is lacking.
Investigators have cited tongue position or activity as reasons for difficulty in achieving long-term stability of anterior open-bite treatment. It was concluded that banded-spur appliances correct anterior tongue posture and maintain long-term stability of open-bite correction. Lingual-spur therapy results in closure of the anterior open bite by successfully keeping tongue pressure away from the anterior teeth and serving as a reminder to the patient to discontinue oral habits. Spur appliance effects include palatal tipping of the maxillary incisors, increases in overbite, and increases in dentoalveolar development of the maxillary and mandibular incisors. Also, when associated with a chincup, they can lead to a significant decrease of the gonial angle. However, some clinicians are wary of using banded spur appliances because of expected negative patient or parent reactions. The use of this appliance has faced resistance from patients, parents, speech pathologists, and psychologists, as well as from some orthodontists. This aversion is linked to the idea that this orthodontic device is a source of irritation, generates discomfort, violates the patients’ space, and is not well tolerated by patients and parents. However, recent studies have shown that treatment with banded or bonded spurs was well accepted by patients and parents and that their reactions to treatment seemed to be similar to or even better than other functional and fixed orthodontic appliances.
Bonded lingual spurs (BLS) were envisioned and designed based on the principles of conventional orthodontic spurs. This appliance has some apparent advantages, such as small size, low cost, esthetics, no laboratory preparation, easy installation, and reduced clinical time for bonding. However, we are aware of only 2 studies that analyzed the effects of the bonded spur appliance in growing patients with anterior open bite. Despite favorable arguments about effectiveness of BLS in early correction of anterior open bite, their effects have not yet been compared with conventional spurs. Therefore, the purpose of this study was to compare the isolated effects of bonded and conventional spurs on the craniofacial and dentoalveolar complexes of patients in the mixed dentition with anterior open bite.
Material and methods
Ethical approval for this multicenter randomized trial was obtained from the research ethics committee of the Federal University of Pernambuco. Written and verbal explanations about the study were provided to the patients’ guardians. Those agreeing to participate completed a written consent form.
The sample size of each group was calculated based on an alpha significance level of 0.05 and a beta of 0.2 to achieve power of 80% to detect a mean difference of 2.0 mm in overbite change between the groups, with an estimated standard deviation of 1.69 mm, according to Cassis et al. The sample size calculation showed that 21 patients in each group were needed. The sample sizes of this study comprised at least 20 patients in each group.
To obtain patients for the 2 experimental groups, 1 operator (L.F.G.C.) examined 1124 schoolchildren in Recife, Brazil, with written authorizations from their parents and school supervisors. The subjects were consecutively selected according to the following criteria: between 6 and 11 years of age with Angle Class I malocclusions, anterior open bite equal to or greater than 1 mm, and maxillary and mandibular permanent central incisors fully erupted. Patients with an anterior open bite of at least 1 mm, without other occlusal changes, were invited to participate. None of the selected patients, according to all sample selection criteria, refused to participate after a detailed treatment explanation.
Full eruption in young children is difficult to determine. Therefore, children in the first transitional period were considered to be eligible for treatment when the maxillary lateral incisors were beginning to erupt and the maxillary central incisors still showed an open bite. Additionally, all patients had at least 1 oral habit, such as tongue thrust or thumb or digital sucking, at treatment onset. Children with tooth agenesis, loss of permanent teeth, crowding, maxillary constriction, or posterior crossbites were excluded from this study.
The selected patients were randomly allocated to 2 groups with different treatment protocols: BLS and conventional lingual spurs (CLS). The 2 experimental groups of the study were prospectively treated by 1 investigator (L.F.G.C.) at the orthodontic department of the Federal University of Pernambuco. The control group data were obtained from the files of the orthodontic department of the Bauru Dental School, University of São Paulo.
Group 1 consisted of the initial and final lateral headfilms of 20 patients (10 girls, 10 boys) treated with BLS. Each subject had an Angle Class I malocclusion, and the initial mean anterior open bite was 4.01 mm (SD, 2.52). The initial mean age was 9.31 years (SD, 1.17).
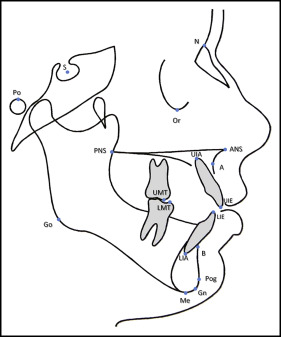
The protocol used in this group consisted of therapy with BLS (Tongue Tamers; Ortho Technology, Tampa, Fla) for 12 months. These appliances were bonded on the palatal and lingual surfaces of the maxillary and mandibular incisors with Concise Orthodontic Chemical Curing Adhesive (3M Unitek, Monrovia, Calif). The bonded spurs were sharpened with a carborundum disk before installation, according to the methods of Haryett et al and Justus. The bonded spurs were positioned in the cervical and incisal portions of the maxillary and mandibular incisors, respectively, to prevent possible future occlusal interferences ( Fig 1 , A ).

Group 2 consisted of the initial and final lateral headfilms of 21 patients (12 female; 9 male) treated with CLS. Each subject had an Angle Class I malocclusion, and the initial mean anterior open bite was 3.03 mm (SD, 1.37). The initial mean age was 9.22 years (SD, 1.62).
The protocol used in this group consisted of therapy with CLS for 12 months. The spur appliance was constructed from 0.045-in stainless steel wire to which 8 short, sharpened 0.026-in spurs, 3 mm in length, were soldered to the anterior part. The spurs were positioned 3 mm from the cingula of the maxillary incisors and were directed at an angle (downward and backward) to encourage correct tongue posture, with the tip of the tongue behind the maxillary central incisor papilla. The spur appliance was soldered to maxillary molar bands and cemented with Multi-Cure Glass Ionomer Band Cement (3M Unitek). The spurs were also sharpened with a carborundum disk before installation ( Fig 1 , B ).
Radiographs of the 2 experimental groups were taken after the 12-month treatment period, within 30 days after appliance removal.
The control group (group 3) consisted of 27 untreated subjects with an Angle Class I malocclusion and an initial mean anterior open bite of 3.30 mm, obtained from the files of the orthodontic department at Bauru Dental School, University of São Paulo. This sample had no treatment and was previously selected according to the same criteria as above. The cephalometric data were obtained from lateral headfilms at a comparable time period as the experimental groups, for the control group, as seen in Table I . The control group had been selected for previous studies regarding early open-bite treatment and was used here as well.
| Variable | BLS group (n = 20) | CLS group (n = 21) | Control group (n = 27) | P | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Initial age (y) | 9.31 | 1.17 | 9.22 | 1.62 | 8.5 | 1.12 | 0.0648 |
| Initial overbite (mm) | −4.01 | 2.52 | −3.04 | 1.37 | −3.35 | 1.92 | 0.2717 |
| Treatment/observation time (y) | 1.06 | 0.06 | 1.08 | 0.07 | 1.06 | 0.1 | 0.5133 |
| SN.GoGn (°) | 36.25 | 3.63 | 35.38 | 3.36 | 33.42 | 5.63 | 0.0895 |
| FMA (°) | 29.05 | 5.08 | 29.75 | 3.63 | 29.57 | 5.59 | 0.8925 |
| SN.PP (°) | −0.63 | 2.5 | −0.47 | 2.8 | −1.68 | 3.14 | 0.3216 |
| Y-axis (°) | 69.55 | 2.58 | 68.94 | 2.48 | 67.46 | 3.98 | 0.0751 |
The 3 groups were at stage 1 of cervical vertebrae maturation, which is the period before the peak in skeletal maturity, according to Baccetti et al.
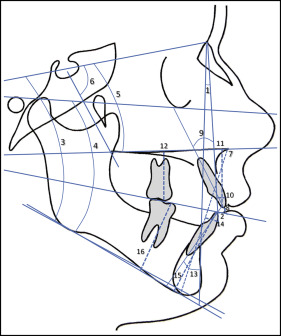
All landmarks were identified and digitized by 1 investigator (L.F.G.C.) using Dolphin Imaging Software (version 10.5; Dolphin Imaging and Management Solutions, Chatsworth, Calif). These data were stored in a computer, and the software corrected the image magnification factor of the control group, which was 9.5%. The experimental groups had digital lateral radiographs taken; therefore, no magnification factor correction was necessary. The radiographs were traced in random order by 1 operator (L.F.G.C.) to reduce bias ( Figs 2 and 3 ).
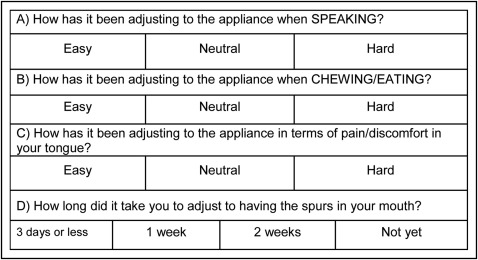
After 1 month of treatment, patient acceptance of the spurs was evaluated with a questionnaire, similar to that proposed by McRae. The questionnaire consisted of questions on patient reactions during speaking, chewing, and eating, discomfort to the tongue, and how long it took to adjust to the spur therapy ( Fig 4 ).
Within a month from the first measurement, 20 digitized lateral radiographs were randomly selected and remeasured by the same examiner (L.F.G.C.). The random errors were calculated according to Dahlberg’s formula (Se 2 = Σd 2 /2n), where Se 2 is the error variance, and d is the difference between the 2 determinations of the same variable. The systematic errors were calculated with dependent t tests, at P <0.05.
Statistical analyses
Data distribution was analyzed with Kolmogorov-Smirnov tests. The pretreatment cephalometric characteristics, and the treatment and normal growth changes were normally distributed in the groups and therefore were compared using 1-way analysis of variance (ANOVA), followed by Tukey tests.
Intergroup comparability regarding initial ages, anterior open-bite severity, observation period, and craniofacial growth pattern were evaluated with ANOVA. The chi-square test was used to compare sex distributions in the groups.
Treatment and normal growth changes were calculated by subtracting the initial from the final values. Means and standard deviations were calculated for the treatment and normal growth changes in all variables. Intergroup treatment and normal growth changes were compared using ANOVA, followed by Tukey tests.
Chi-square tests were used to compare the acceptability of conventional vs bonded lingual spur treatments.
All statistical analyses were performed with Statistica software (version 7.0; StatSoft, Tulsa, Okla). Results were considered significant at P <0.05.
Results
Linear random errors ranged from 0.08 (Mx1-PP) to 0.27 mm (overjet), and angular random errors ranged from 0.15° (Md1.NB) to 2.0° (SN.GoGn). There were no statistically significant systematic errors.
At the pretreatment stage, the groups were comparable regarding age, anterior open-bite severity, observation period, craniofacial growth pattern, and sex distribution ( Tables I and II ).
| Group | Sex | Total | |
|---|---|---|---|
| Female | Male | ||
| BLS | 10 | 10 | 20 |
| CLS | 12 | 9 | 21 |
| Control | 22 | 5 | 27 |
| Total | 44 | 24 | 68 |
During treatment, there was a significantly greater decrease in overjet in the BLS group compared with the control group. There were significantly greater increases in overbite in the BLS and CLS groups compared with the control group ( Table III ).



