To obtain optimal and predictable aesthetics, deficiencies caused by soft and particularly hard tissue loss can be managed by various methods, such as orthodontic tooth eruption, socket preservation, and guided bone regeneration. However, in complex cases, these methods are often insufficient. Here, the authors introduce advanced concepts in aesthetic implant dentistry, such as “Aesthetic Site Foundation”, “Aesthetic Guided Bone Regeneration” and “Implant Rectangle” that will guide the clinician in the quest to optimal aesthetic outcomes.
The establishment of optimal and predictable aesthetics is one of the most important and challenging aspects of rehabilitation with dental implants. Aesthetic rehabilitation is important, not only because achieving the “perfect smile” is demanded by our beauty-oriented society, but also because individual impairment and disability may result from aesthetic deficiencies.
The goal of aesthetic rehabilitation is to alleviate or eliminate deficiencies and to obtain optimal aesthetics. Optimal aesthetics should be defined as the patient’s perception of “visually pleasing or satisfying,” and the clinician’s assessment of acceptable anatomic architecture coupled with proper function of the masticatory system (mastication, speech, swallowing).
Aesthetic rehabilitation has to be predictable, implying reproducibility and stability of the outcome in the short and long term. Achieving these characteristics depends on the interaction between multiple variables, namely, biologic (anatomic factors, host response), surgical (procedure, technical skills), implant (dimensions, surface characteristics, design), and prosthetic factors . It is obvious that analyzing, selecting, and integrating each of these factors is challenging. Because most often aesthetic rehabilitation encompasses “the aesthetic zone” of the anterior maxilla, this article focuses on this area. This article discusses several anatomic, surgical, and implant criteria that have to be considered to achieve optimal and predictable aesthetics. Specifically, it introduces the concepts of “Aesthetic Site Foundation”, “Aesthetic Guided Bone Regeneration”, and “Implant Rectangle”. It helps guide the clinician in assessing anatomic factors by using morphologic and radiographic (CT scan) landmarks. Finally, the integration of the criteria described and the underlying rational are presented through illustrations and clinical scenarios.
Background knowledge
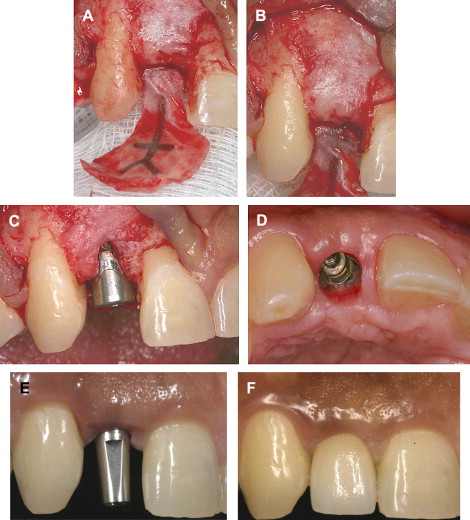
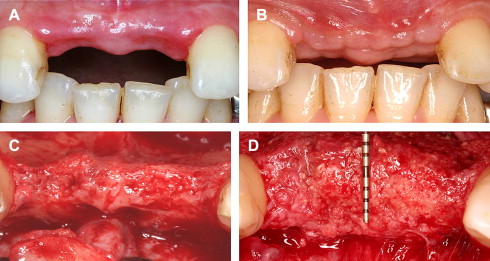
Aesthetic deficiencies may result from numerous pathologic conditions . Even after a simple atraumatic tooth extraction, the alveolar ridge may lose approximately 4 mm in the buccal dimension . Moreover, with tissue borne denture usage, the alveolar ridge resorption occurs at even higher rates resulting in significant ridge deformities . In the maxilla, this resorption can be vertical and horizontal with buccal and palatal components significantly compromising the potential for aesthetic rehabilitation ( Fig. 1 ) .
Several methods have been used to preserve and enhance the alveolar bone in the anterior maxilla before implant placement. Some frequently used ones are orthodontic tooth eruption, socket preservation, and guided bone regeneration (GBR) . Although these techniques are effective in many clinical situations, they may not be sufficient in complex cases, especially where bone loss is more severe and comprises more than one aspect of the alveolar ridge (ie, vertical, buccal, and palatal). Horizontal augmentations by GBR are predictable; however vertical ones are less assured . Most horizontal bone augmentations are performed on the buccal aspect of the alveolar ridge. Often the augmentation is performed purely to provide what seems to the practitioner as enough bone to cover any potential implant thread dehiscence. However, to ensure long-term stability of the soft tissue, at least 2 mm of facial bone thickness is required buccal to the implant . Therefore, when a ridge deformity is complex and/or aesthetic requirements are high, it is necessary for the practitioner to have a clear vision and understanding of the three-dimensional envelop of bone surrounding an implant. Once this is achieved, the proper augmentation approach can be selected.
Another variable to be considered in aesthetic reconstruction is the bone and soft tissue remodeling following surgical intervention. The remodeling of augmented bone and the formation of the biologic width are concerns that need to be addressed. To compensate for bone resorption, the authors advocate over building of the defective ridge; this is discussed in further details in the article. Additionally, the implications that arise from the formation of the biologic width have to be considered buccally, lingually, and interproximally. For a comprehensive review of the remodeling that occurs following the formation of the biologic width, the following articles are appropriate: .
Creating the Aesthetic Site Foundation
Careful planning, superior execution, and objective evaluation of the aesthetic outcome are critical phases in the establishment of the Aesthetic Site Foundation. Important principles of each of these phases are described. The authors of this article are strong proponents of the staged approach (ie, building one step at a time based on previously successful outcomes before placing an implant into a deficient ridge), particularly in complex cases such as the ones described.
Aesthetic planning
In treatment planning an aesthetic area, the clinician must consider a manifold of important elements. Most of these have been discussed in detail in the literature. They range from evaluating broad characteristics such as facial dimensions and smile line, to detailed considerations of the delicate papilla. However, when dental implants are used in the aesthetic site, the clinician must consider another critical element: the Aesthetic Site Foundation. The edentulous ridge’s osseous dimensions and contour, as well as its spatial relation to the overall aesthetic zone and tooth position are what create the Aesthetic Site Foundation. To plan for the aesthetic implant site, the clinician must determine the criteria composing the Aesthetic Site Foundation.
Criteria for the Aesthetic Site Foundation
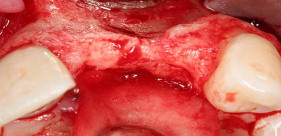
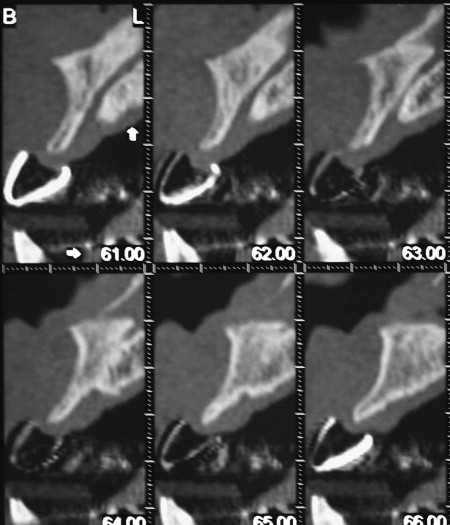
Determination of site requirements is initially similar to all types of aesthetic evaluations. It starts with the diagnostic wax-up, necessary radiographs, mounted study models, and clinical photographs. Incisal and buccal clinical photographic views should be taken. In addition, it is important to create a radiographic template. This template should delineate radiographically the contours of the wax-up, especially the buccal and lingual location of the ideal cemento–enamel junction ( Fig. 2 ). This template is worn by the patient during the administration of the CT scan. Evaluation of the CT scan with the radiographic template allows the analysis of the condition of the Aesthetic Site Foundation. One of the significant findings during this phase of investigation is the determination of the ridge defect spatially. It has become common to see discussion of ridge augmentations as they pertain to buccal or crestal defects. However, it is the authors’ contention that therapy of the insufficient ridge cannot be approached based on buccal and crestal defects alone. In developing the Aesthetic Site Foundation, it is paramount that one also examines the following questions: does a palatal defect exist; how does the existing ridge deficiency relate to other existing structures and proposed implant position(s)? This information in connection with the other diagnostic parameters provides the elements required for treatment planning.
Ridge defect
The standard ridge defect classification introduced by Seibert is helpful during the clinical evaluation in assessing the type of deformity. Further evaluation of the ridge defect is necessary after a CT scan is taken. Addressing the combination of soft and hard tissue deformity in the vertical, buccal, and lingual dimension is of paramount importance in determining the surgical approach for the augmentation procedure ( Figs. 2–4 ).
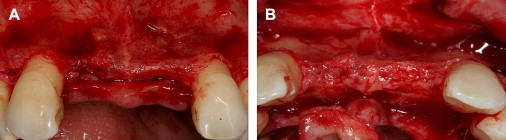
The goal of the augmentation procedure is to create enough bone around the implant to ensure maximum longevity of the implant and stability of the hard and soft tissue. To that end it is necessary to have 2 mm of bone thickness around the implant, especially at the crestal level ( Fig. 5 ). This thickness is required to maintain the height of bone following remodeling of the biologic width . Therefore, the authors submit the concept of the “Implant Rectangle,” which is visualized in radiographic cross-sectional analysis. The Implant Rectangle is defined by superimposing vertical lines placed 2 mm buccal and 2 mm lingual to the proposed implant site, and by placing horizontal lines at the platform and at the apex level of the proposed implant. The horizontal line at the platform level is positioned parallel to the proposed buccal and lingua cemento–enamel junction and approximately 3 mm apical to it. The horizontal line at the apical level is positioned relative to the length of the implant desired and/or limitations of anatomic structures. These dimensions of the Implant Rectangle represent the minimum volume of bone required to obtain an aesthetic result ( Fig. 6 ). Prosthetically, the buccal and lingual aspects of the tooth fall within the coronal extension of the vertical walls of the Implant Rectangle. This makes the location of the Implant Rectangle prosthetically driven. When a cement-retained restoration is planned, the implant is well within the Implant Rectangle, and the surgeon has a wide range of implants that can be used ( Fig. 7 ). However, when a screw-retained restoration is selected, either additional volume of bone is needed at the apical aspect of the implant (in comparison to a cement-retained restoration), or a tapered or short implant is needed to keep the implant within the Implant Rectangle ( Fig. 8 ). In summary, the location of the Implant Rectangle is prosthetically driven, and its dimensions are biologically driven. In essence, to achieve aesthetic results around implants placed in the anterior maxilla, the patient’s soft and hard tissue should be transformed into a thick squared biotype. Understanding the three-dimensional criteria and the concept of the Implant Rectangle, introduced in Figs. 6–8 , provides guidelines in developing the necessary augmentation for the Aesthetic Site Foundation ( Figs. 9–11 ).