Introduction
Our objectives were to evaluate the amount of decompensation of the mandibular incisors and the change of periodontal support around them after corticotomy with bone augmentation before orthognathic surgery.
Methods
Before orthognathic surgery for 15 skeletal Class III patients, orthodontic treatment was combined with corticotomy and bone augmentation labially to the anterior mandibular roots. Lateral cephalograms were taken before orthodontic treatment and before surgery (completion of preoperative orthodontic treatment). The amounts of mandibular incisor proclination, alveolar bone thickness, and periodontal support (gingival margin levels and augmentation pattern) were evaluated.
Results
Significant proclination of the mandibular incisors was shown after decompensation ( P <0.001; incisor mandibular plane angle, 10.45°; incisor symphyseal plane angle, 10.74°). The incisor edge moved labially by 3.47 mm. The alveolar bone thickness increased by 1.56 mm at the root apex and 1.98 mm at the level of B-point ( P <0.001). There was no gingival recession irrespective of the degree of proclination of the mandibular incisiors. Two types of bone augmentation pattern were evident. One was characterized by alveolar bone proclination proportional to the labial tipping of the mandibular incisors. Buccal alveolar bone at the cervical area was well maintained (60%, 9 subjects). The other showed greater increases in alveolar thickness at B-point than at the cervical area (40%, 6 subjects).
Conclusions
The augmented corticotomy provided effective decompensation of the mandibular incisors in skeletal Class III patients while maintaining labial bone thickness and with no periodontal side effects. This technique reduces or eliminates the risk of moving the roots through the labial plate during decompensation with the associated risk of gingival recession.
Orthognathic surgery combined with orthodontic treatment has become commonly accepted for skeletal Class III malocclusions. This has been facilitated by wider patient awareness and improved surgical and orthodontic techniques. Dentoalveolar compensation is common in patients with Class III malocclusions. To achieve the best surgical result, compensated (retroclined) mandibular incisors should be uprighted to their normal inclinations. It has been reported that clinicians typically introduce decompensation of the mandibular incisors, but often the correction is short of the norm.
Various methods to induce incisor decompensation have been reported: temporary skeletal anchorage devices, intermaxillary elastics, or pushing coils to open spaces for the third premolars. These methods can correct incisor inclinations, but the clinician must also attend to the health of the periodontum around the mandibular incisor roots. It appears that, in patients with mandibular prognathism, alveolar bone loss or fenestration is more common in the anterior mandibular teeth. A previous study showed that the mean amount of vertical bone loss at the mandibular central incisor in surgical skeletal Class III patients was 6.87 mm; this means that 62.88% of the root length was not covered by alveolar bone. Tipping the mandibular incisors will improve the surgical result but has the risks of bony dehiscence, fenestration, and gingival recession. The clinician facing this conundrum might choose not to fully upright the mandibular incisors to prevent periodontal risk.
Augmented corticotomy combined with orthodontic treatment can be used to overcome these limitations. It is a combination of selective alveolar decortication, alveolar augmentation by using particulate bone grafting material, and orthodontic treatment. The biologic basis of augmented corticotomy has been suggested to be mediated by a regional acceleratory phenomenon. It has been hypothesized that a corticotomy or an osteotomy induces an intensified osteoclastic activity resulting in osteopenia, increased bone remodeling, and rapid tooth movement. Therefore, it enhances the range of possible tooth movements with increased alveolar bone volume and a more structurally complete periodontium. There has been only 1 other case report about dental decompensation of anterior teeth in Class III treatment combined with augmented corticotomy.
The goal of this study was to evaluate the amount of decompensation of the mandibular incisors and the change in periodontal support with an augmented corticotomy combined with orthodontic treatment before orthognathic treatment.
Material and methods
Fifteen patients (7 men, 8 women; mean age, 25.15 years) with skeletal Class III malocclusion treated at the Department of Orthodontics at Kyung Hee University Dental Hospital in Seoul, Korea, were recruited for this study ( Table I ). All patients were planned for 2-jaw surgery (bisagittal split ramus osteotomy setback with LeFort I osteotomy). The study was performed with the approval of the institutional review board of Kyung Hee University Dental Hospital (KHU-IRB-110604). The inclusion criteria were bilateral skeletal and dental Class III relationships, lack of severe facial asymmetry (less than 3 mm of chin point deviation from the facial midline), less than 3 mm of crowding in the mandibular arch, no missing or malformed teeth, and the use of the 0.022-in Roth prescription appliance, fully bonded to the second molars.
| Measurement | Men (n = 7) | Women (n = 8) | Total (n = 15) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| SNA (°) | 82.81 | 2.11 | 81.92 | 3.47 | 82.33 | 2.85 |
| SNB (°) | 86.21 | 2.86 | 84.11 | 3.80 | 85.09 | 3.45 |
| ANB (°) | −3.41 | 3.01 | −2.20 | 1.45 | −2.76 | 2.31 |
| SN-MP (°) | 32.28 | 4.59 | 40.72 | 5.94 | 36.78 | 6.76 |
| FMA (°) | 25.81 | 5.23 | 33.16 | 5.74 | 29.73 | 6.53 |
| Age (y) | 24.73 | 3.56 | 25.52 | 4.21 | 25.15 | 4.13 |
| Duration (mo) | 8.64 | 3.44 | 6.38 | 2.56 | 7.43 | 3.12 |
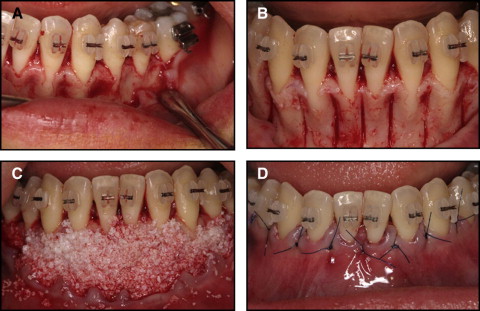
Immediately after bracket bonding, full-thickness flaps were reflected labially by using a sulcular incision. In some patients, the interdental papillae were reflected with the flaps; in others, they were left in place. A vertical releasing incision was made at the premolar area as needed ( Fig 1 , A ). Decortication was performed with a number 2 round bur in a high-speed hand piece or piezoelectric surgical device ( Fig 1 , B ). Vertical grooves were placed in the interradicular space, midway between the root prominences extending from a point 2 to 3 mm below the crest of the bone to a point 2 mm beyond the apices of the roots. These vertical corticotomies were then connected with horizontal corticotomies apically to the root end. Sufficient bleeding in the decorticated area was confirmed, and then the bone graft materials were placed. Mineralized and deproteinized bovine bone mineral (Bio-Oss; Geistlich Pharma, Wolhusen, Switzerland) was used for the alveolar augmentation ( Fig 1 , C ). Interdental papillae were repositioned and sutured with 5-0 or 6-0 nylon with vertical everting mattress sutures ( Fig 1 , D ). It is critical to achieve primary closure to protect the bone graft material. After the flap was repositioned, an immediate heavy orthodontic force was applied to the teeth. Further details of the procedure have been described in a previous article.
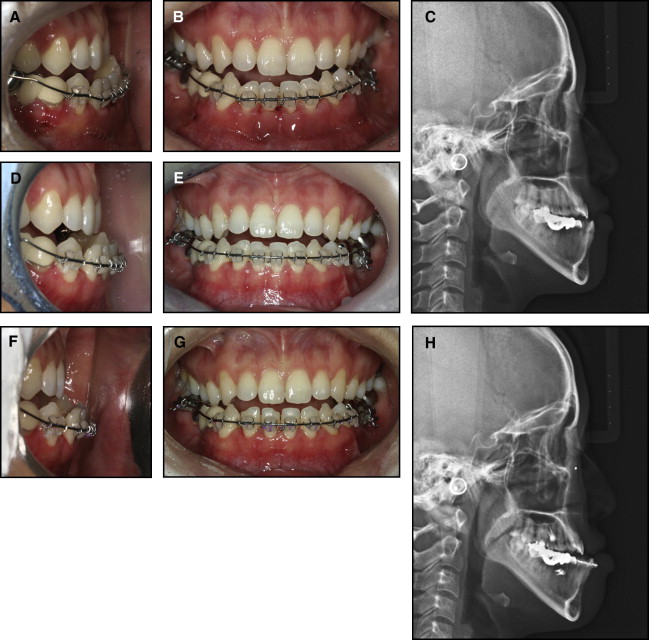
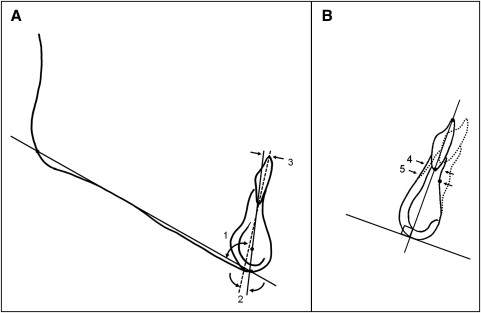
Lateral cephalograms were taken before orthodontic treatment and before surgery (completion of preoperative orthodontic treatment) ( Fig 2 ). Definitions of the landmarks, reference planes, and dental and alveolar variables are given in Figure 3 . The amount of mandibular incisor proclination was evaluated in relation to the mandibular plane or the symphyseal plane. The symphyseal plane was suggested as the line between Steiner’s D-point and the root apex of the mandibular incisor before treatment. The root apex at the initial stage is assumed to be the physiologic center of the alveolar portion, as is D-point in the basal portion. Alveolar bone thickness (labiolingual dimension) was measured along a perpendicular to the long axis of the tooth before treatment at both B-point and the root apex of the mandibular incisor. Cephalometric measurements were made by 1 operator using the V-Ceph program (version 5.5; Osstem Co, Seoul, Korea).
Statistical analysis
The raw data of the 15 patients are shown in Table II .
| Patient | Variables | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IMPA (°) | ISPA (°) | ISPD (mm) | LAW (mm) | BTH (mm) | ||||||
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| 1 | 77.50 | 86.00 | 10.20 | 16.78 | 4.20 | 7.20 | 6.05 | 10.15 | 7.50 | 11.67 |
| 2 | 88.00 | 93.00 | 12.80 | 19.50 | 4.50 | 7.00 | 6.02 | 8.95 | 5.00 | 9.17 |
| 3 | 75.00 | 93.00 | −4.10 | 15.00 | −1.50 | 5.30 | 9.91 | 10.02 | 8.75 | 9.58 |
| 4 | 77.00 | 84.00 | 0.10 | 9.20 | 0.20 | 3.95 | 6.80 | 9.70 | 5.83 | 9.17 |
| 5 | 66.00 | 77.00 | −3.00 | 9.00 | −1.00 | 3.60 | 4.00 | 5.60 | 4.17 | 5.42 |
| 6 | 67.50 | 78.00 | −6.35 | 5.05 | −2.00 | 2.20 | 3.50 | 3.60 | 3.30 | 5.20 |
| 7 | 84.00 | 90.00 | 16.60 | 24.10 | 6.50 | 9.40 | 5.00 | 5.10 | 5.83 | 6.67 |
| 8 | 73.00 | 87.00 | −6.00 | 9.20 | −1.90 | 3.00 | 6.00 | 7.20 | 6.67 | 7.92 |
| 9 | 78.24 | 86.08 | 10.10 | 16.50 | 4.00 | 4.50 | 7.10 | 8.60 | 6.90 | 8.60 |
| 10 | 85.33 | 94.24 | 17.00 | 25.20 | 6.50 | 8.60 | 6.10 | 9.50 | 6.89 | 11.05 |
| 11 | 79.10 | 96.05 | 14.10 | 31.00 | 5.15 | 8.23 | 5.11 | 5.70 | 5.00 | 5.10 |
| 12 | 86.20 | 101.87 | 12.50 | 27.00 | 4.90 | 9.20 | 7.71 | 7.90 | 8.00 | 9.20 |
| 13 | 76.10 | 80.50 | 5.14 | 9.20 | 1.80 | 4.60 | 2.00 | 4.50 | 6.60 | 8.90 |
| 14 | 76.10 | 86.61 | 0.20 | 11.30 | 0.10 | 2.70 | 2.10 | 2.12 | 5.30 | 5.60 |
| 15 | 80.80 | 93.21 | 10.80 | 23.20 | 3.50 | 7.50 | 5.18 | 7.31 | 6.90 | 9.10 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


