Chapter 42 A minimally invasive technique for tongue base stabilization
1 INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) results from a complex scenario initiated with airway collapse and obstruction, loss of compensatory wake and sleep reflexes, increased ventilatory effort, arousal, hypoventilation, and asphyxia during sleep. In adults, a structurally small upper airway may be a primary contributing factor. Enlarging this airway may prevent the cascade into sleep apnea and snoring.
2 RATIONALE
Obstruction during sleep is the result of a complex cascade. During inspiration, upper (pharynx) and lower (chest wall and diaphragm) airway muscles are activated. The lower airway muscles create a negative intraluminal force balanced by upper airway muscles that stiffen and dilate the airway. Increases in negative airway pressure or loss of muscle dilation will obstruct the airway. In sleep-disordered breathing both occur. Increased upper airway resistance leads to more negative intraluminal pressure and activation of upper airway dilator muscles is delayed or decreased. During expiration, positive pressure forces dilate the airway, and upper airway muscle tone is reduced. If the balance is unfavorable and the effects of tissue mass are not compensated, collapse and obstruction occur.
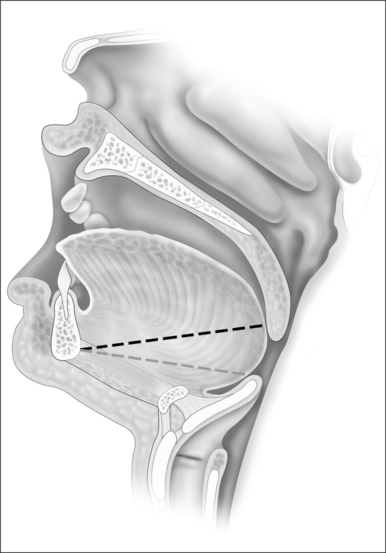
Since during expiration the largest decreases in airway size occur in the hypopharynx, treatment of this segment may be critical for most if not all individuals with sleep-disordered breathing. The tongue suspension procedure was conceived as a means of providing an extraluminal dilating force to the lower pharyngeal airway in contrast to nasal Continuous Positive Airway Pressure (CPAP) which is an intraluminal dilating force. This is accomplished by passing a submucosal suture into the posterior midline tongue. The suture prevents passive collapse while not interfering with anterior and superior tongue movements which are involved with swallowing and speech. Placement is directed towards the level of the foramen cecum (Fig. 42.1).
3 TONGUE SUTURE SUSPENSION TECHNIQUE
3.1 STEP ONE (BONE ANCHOR)
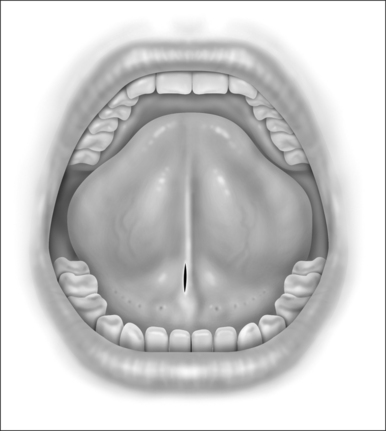
When performing the intraoral approach, an intraoral incision is made posterior to the salivary papillae (Fig. 42.2). The incision should be generous. An excessively long linear incision is easily closed with excellent healing. An incision too small for the device may result in mucosal tearing that may damage the papillae and create an intraoral scar. If an external incision is used an incision is made 1cm posterior to the gnathion in a convenient skin crease or shadow.
< div class='tao-gold-member'>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses