Temporomandibular Disorders
Effects of Occlusion, Orthodontic Treatment, and Orthognathic Surgery
• Incidence of Temporomandibular Disorders in the General Population and the Basic Treatment Approach
• Review of Occlusal Factors and Association with Temporomandibular Disorders
• Occlusal Conditions More Frequently Associated with Temporomandibular Disorders
• Orthodontic Treatment and Its Effects on Temporomandibular Disorders
• Association of Jaw Deformities, Orthognathic Surgery, and Temporomandibular Disorders
• Brief Overview of Okeson’s Thinking About Temporomandibular Disorders and the Effects of Occlusion
• Personal Thoughts About the Role of Open Joint Procedures for Temporomandibular Disorders
Incidence of Temporomandibular Disorders in the General Population and the Basic Treatment Approach
The prevalence of temporomandibular disorders (TMDs) in the general population as reported in the literature varies widely. It is estimated that an average of 32% of the population reports at least one symptom of TMD, whereas an average of 55% demonstrates at least one clinical sign.* Schiffman and colleagues completed a cross-sectional epidemiologic study that indicated that, at any given time, between 40% and 75% of individuals who were not currently seeking treatment had at least one sign of TMD, and about one third of individuals reported at least one symptom of TMD.296 Mongini and colleagues documented a prevalence of TMD symptoms in children and teenagers of 12% and 20%, respectively.210 Wanman and colleagues showed an incidence of joint noise in young adults in their late teens to be as high as 17.5% over a 2-year period.345 TMDs remain a frequent cause of visits to primary care physicians, otolaryngologists, internists, and pediatricians. Despite the high incidence of TMDs, their natural history suggests that, in up to 40% of patients, symptoms resolve spontaneously.296
TMD includes various signs and symptoms of the temporomandibular joint (TMJ), the masticatory muscles, and related structures (Figs. 9-1 through 9-8). These may include a spectrum of referred head and neck pain; joint noise (e.g., popping, clicking, crepitus); reduced or altered mandibular range of movement as a result of muscle spasm or disc displacement; condylar head erosion; and direct pain on palpation of either the TMJ or the masticatory muscles. The signs and symptoms associated with TMDs can also lead to misdiagnosis.16,112,171,216,342




Figure 9-1 A, Intraoral frontal view of dentition juxtaposed with the underlying alveolar bone. B, Intraoral lateral view of dentition juxtaposed with the underlying alveolar bone. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 3, Figures 1-1, A and B, 1-3, and 1-4.
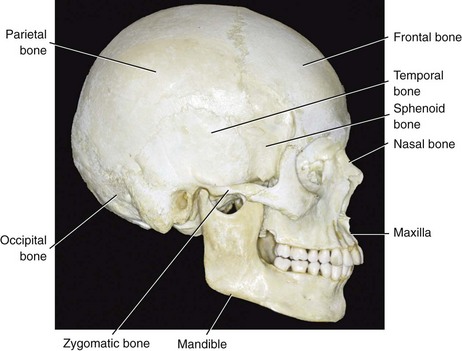
Figure 9-2 Lateral view of the craniofacial skeleton. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 4, Figure 1-5.
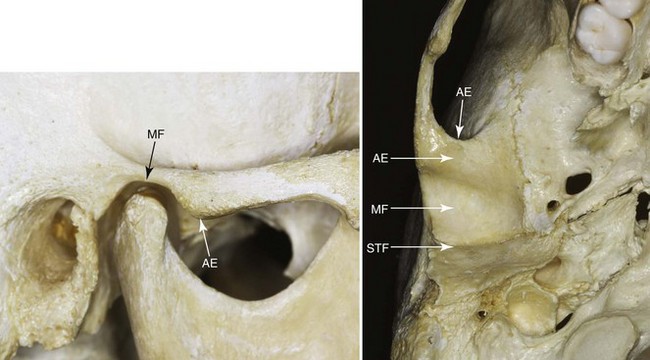
Figure 9-3 Bony structures (components) of the temporomandibular joint. MF, Mandibular fossa; AE, articular eminence; STF, squamotympanic fissure. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 4, Figure 1-12.
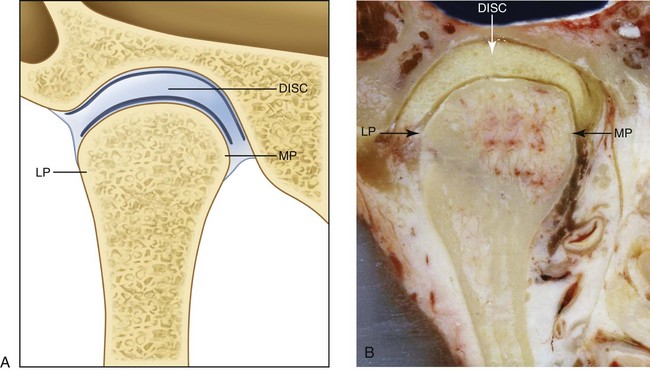
Figure 9-4 Anterior cross-sectional view of the articular disc, the fossa, and the condyle. A, Illustration. B, Cadaver specimen. The disc adapts to the morphology of the fossa and the condyle. LP, Lateral pole; MP, medial pole. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 8, Figure 1-14.
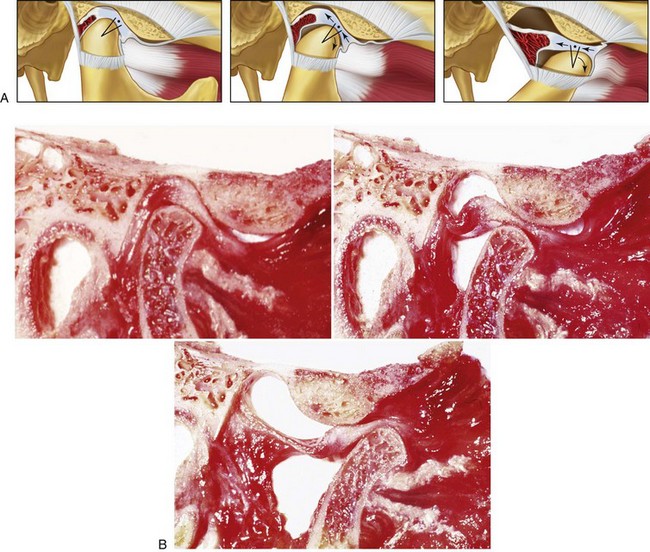
Figure 9-5 A, Lateral view illustrations and B, cadaver specimen views of normal movement of the condyle and disc during vertical mouth opening. As the disc moves out of the fossa, it rotates posteriorly on the condyle. First, rotational movement occurs (predominantly in the lower joint space). After that, translation takes place (predominantly in the superior joint space) as mouth opening continues. A from Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 17, Figure 1-30. B courtesy Terry Tanaka, MD, San Diego, Calif.
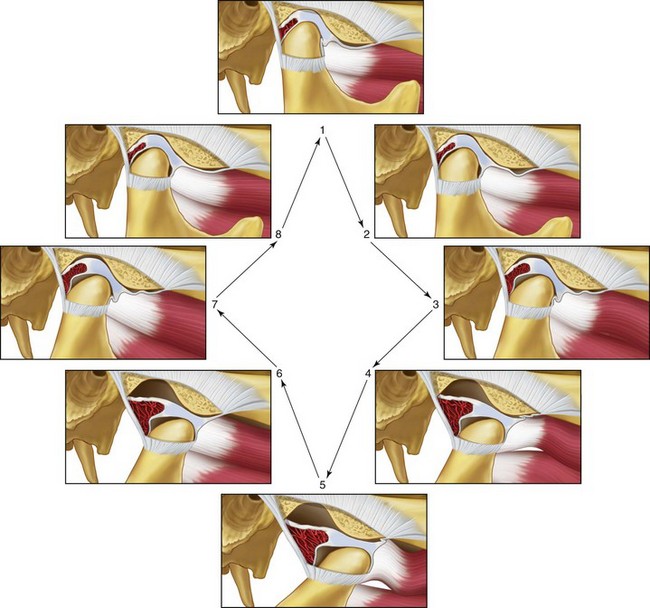
Figure 9-6 Illustrations of the normal functional movement of the condyle and disc during the full range of opening and closing. The disc is rotated posteriorly on the condyle as the condyle is translated anteriorly out of the fossa. The closing movement is the exact opposite of the opening movement. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 19, Figure 1-31.
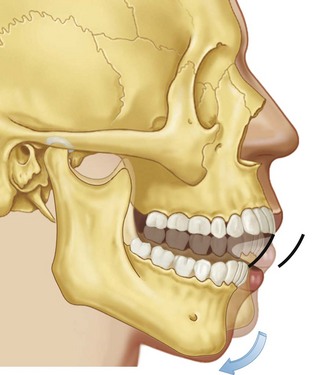
Figure 9-7 Illustration of rotational movement of the mandible. This movement occurs with the condyles in the terminal hinge position. This pretranslation opening will occur until the anterior teeth are approximately 20 to 25 mm apart. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 64, Figure 4-7.
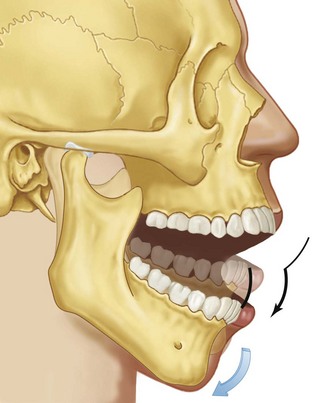
Figure 9-8 The second stage of movement during mouth opening is illustrated. Note that the condyle is translated down the articular eminence as the mouth rotates open to its maximum limit. From Okeson JP: Management of temporomandibular disorders and occlusion, St. Louis, 2012, Elsevier, p 64, Figure 4-8.
A wide variety of often contradictory “conservative” treatment modalities (i.e., non-invasive or potentially reversible) have been recommended to alleviate the symptoms of TMD and to prevent recurrence.* Enthusiasm by clinicians for the direct surgical alteration of the structures that comprise the TMJ to treat TMD have waxed and waned over the past half century.60,71,141,143,200,222,241,344 Occlusal factors (i.e., degrees of malocclusion) are often claimed to be associated with TMD. Although it is sometimes stated that orthodontic treatment increases the prevalence of TMD, it is also claimed that orthodontic maneuvers (for at least some types of malocclusion) may reduce the signs and symptoms of TMD. Studies document that the correction of a baseline jaw deformity with malocclusion through orthodontics and orthognathic surgery improves the presenting TMD in the majority of the treated patients, whereas a minority get worse.6,29,31,67,102,131,152,232,236,347,349,356,359 This is described in greater detail later in this chapter.
Mandibular Range of Motion
The expected normal mandibular range of motion and inter-incisor mouth opening is discussed periodically in the literature.9,70,93,115,146,179,197,234,235,249,308,309,311–313,315,316,318 Even a 6-year-old child can often open the mouth to a maximum 40 mm or more. Measurements of maximum vertical mouth opening with and without discomfort are considered useful parameters of TMJ health. A restricted mouth opening is considered by many to be a distance of less than 40 mm. Only 1.2% of young adults open their mouths less than 40 mm. However, 15% of the healthy elderly population open their mouths less than 40 mm. Any lateral or protrusive movement of less than 8 mm is considered restricted, although the significance of this measurement is unclear.
Review of Occlusal Factors and Association with Temporomandibular Disorders
Clinicians from a spectrum of medical and dental specialties often consider malocclusion to be the major etiologic factor of TMD.† An assumed strong association between TMD and the malpositioning of the teeth serves as one reason why the diagnosis and treatment of TMD is generally considered within the purview of dentistry. Many of the therapeutic options for the treatment of TMD are based on the idea of “normalizing” or “neutralizing” the occlusion.135,355 Common treatment approaches to do so include the reversible use of an occlusal appliance or definitive techniques such as occlusal adjustment (equilibration), restorative dentistry, orthodontics, and orthognathic surgery. Concurrently, it is also true that either the onset of TMD or the worsening of current symptoms is frequently blamed on any one of the previously mentioned treatment regimens.
The dental literature contains clinical studies and reports that claim there are causal relationships between occlusal factors and the symptoms and signs associated with TMD. Egermark-Eriksson and colleagues examined 402 children and reported an association between signs and symptoms of TMD, specific malocclusions (i.e., Class II, Class III, anterior crossbite, and anterior open bite), and occlusal supra-contacts.87 Brandt studied 1342 children and found a correlation between TMD and degrees of overbite (deep and open) and overjet.33 Nilner examined 749 teenagers and young adults and reported an association with centric relation (CR)–centric occlusion (CO) discrepancies (i.e., slides), balancing-side contact slides, and symptoms and signs of TMD.220 Confusion in the literature arises as independent research studies have drawn contrary conclusions. DeBoever and colleagues examined 135 individuals with signs and symptoms of TMD and found no specific associations with malocclusion.59 Gunn and colleagues similarly found no association between TMD and occlusion in 151 migrant children that they studied.121 Dworkin and colleagues examined 592 individuals within a specific health maintenance organization and found no association between TMD signs and symptoms and specific occlusions.80
In their review article, Seligman and Pullinger pointed out that the majority of existing clinical research (up to that point in time) did not support a clear relationship between occlusion and TMD symptoms.302 They further clarified that the majority of published research relied on symptom-based data rather than discrete disease classifications. Seligman pointed out that symptoms like joint sounds (e.g., popping, clicking, crepitus) and pain (e.g., in the TMJ region and the masticatory system) lack specificity.303 In addition, most published studies did not differentiate between TMD diagnostic categories (e.g., disc displacement, myalgia, TMJ osteoarthritis). Most published studies also suffered from a lack of or an inadequate control group. Seligman and colleagues attempted to avoid these shortcomings by completing a multifactorial analysis of the risks and relative odds of an individual having a TMD as a function of 1 of 11 common occlusal features.259,304 They looked for correlations between each of these 11 specific occlusal factors (Box 9-1) and 1 of 6 TMJ diagnostic categories (Box 9-2), including asymptomatic normal controls without TMD.259
• Overjets ranging from –1 to +6 mm
• Overbites ranging from –2 to +10 mm
• Midline discrepancies of up to 5 mm
• Anteroposterior molar relationships from –6 to +6 mm
Pullinger and colleagues concluded that occlusion cannot be considered the most important factor in the definition of TMD but that specific occlusal factors do make biologic contributions to TMD and thus cannot be ignored.254–261 In most individuals, they observed that the human biologic system will adapt to a variety of malocclusions in an attempt to achieve TMJ stability. The authors surmised that some occlusal features will place greater adaptive demands on the individual’s biologic system than others. Although most individuals are able to compensate for their occlusal disharmony without problems, adaptation for others may lead to a greater risk for TMD. On the basis of this data, the authors stressed the importance of five occlusal conditions, which in isolation or combination are more likely to reach the threshold that exceeds adaptation for an individual and therefore results in TMJ dysfunction. The high-risk malocclusions are discussed later in this chapter.
Occlusal Conditions More Frequently Associated with Temporomandibular Disorders
Anterior Open Bite
Research by Pullinger and colleagues showed a strong relationship between osteoarthritis of the condylar head with a loss of condylar height and an anterior open-bite malocclusion.254–261 Interestingly, anterior open bite was not commonly associated with disc displacement disorders with or without reduction. Myalgia (i.e., masticatory muscle discomfort) was also a frequent symptom among patients with an anterior open bite. It is not stated in what percentage of individuals the anterior open-bite malocclusion occurred only secondarily as a result of osteoarthritis followed by a loss of condylar height with clockwise rotation of the mandible. Therefore, it is unclear what percentage of the examined individuals with anterior open bites had these finding as part of a developmental jaw deformity.
Centric Relation–Centric Occlusion Slides
Limited occlusal slides (i.e., 1 mm) were common in all patient groups, including the normal controls. CR–CO slides of more than 2 mm were only found in the patients with TMDs. Pullinger found that larger slides were frequently associated with osteoarthritis of the condylar head. He questioned the advisability of the clinicians’ automatic attempt to “relieve” the occlusal slides in all individuals—whether by irreversible (e.g., occlusal equilibration, orthodontics, surgery, restorative dentistry) or reversible (e.g., occlusal splints) means—because the observed slide may be either adaptive or inconsequential.260
Unilateral Maxillary (Lingual) Crossbite
The occlusal feature of unilateral maxillary crossbite occurs in about 10% of the adult population, and it is frequently found in association with TMJ disc displacement with or without disc reduction. Approximately 25% of the patients with non-reducing disc displacements were found to have unilateral maxillary lingual crossbites. This indicated to Pullinger and colleagues that disc displacement may be a biologic adaptive response of the individual to a unilateral maxillary lingual crossbite.260 The investigators theorized that these individuals may later be prone to osteoarthritis. They suggested that the orthodontic treatment of a unilateral crossbite discovered during childhood should be considered as a preventative measure to reduce the adaptive demands on the masticatory system. They did not come to the same conclusion for the correction of a longstanding unilateral posterior crossbite in an adult, because skeletal adaptation would have already occurred. Unfortunately, the investigators did not clarify if the crossbites in their study patients were the result of developmental jaw deformities (e.g., asymmetrical mandibular excess) or simply due to the malpositioning of the teeth. They did not specifically comment on whether orthognathic surgery should be carried out in conjunction with orthodontics (if needed) in young adults to correct the presenting malocclusion as a way to prevent the progression of TMD.
Missing Posterior Teeth (≥5)
The investigators found that, when five or more posterior teeth were missing, the incidence of TMD increased. This includes TMD categories of both osteoarthritis and disc displacement with or without osteoarthritis. Pullinger and colleagues further claimed that, when two or four of the “posterior teeth” (bicuspids) were removed as part of an orthodontic treatment protocol, there was a negligible effect on TMD.260 Other studies carried out by Kayser156 and Witter354 have also documented acceptable masticatory function after bicuspid extractions and orthodontic treatment without increased signs and symptoms of TMD.
In the Pullinger and Seligman study, it must be assumed that many of the significant overjets observed in the adult subjects were secondary deformities after condylar resorption (i.e., condylysis).260 The authors did not present evidence to suggest that the presence of significant overbite or overjet plays a role in the pathophysiology of non-arthritic disorders of the TMJ, and they did not show that it was a causative factor in the observed osteoarthritis. They do believe that a combination of unilateral retruded centric position in the presence of a clinically apparent retruded centric position–inter-contact position slide may encourage TMJ disc displacement but that unilateral retruded centric position per se is not associated with TMD. They found that lost molar support (i.e., 4 or 5 posterior teeth) may be associated with osteoarthrosis. They concluded that a dental midline discrepancy is not a predictor of TMD development during adulthood. Anterior open bite is frequent in the presence of condylysis or osteoarthritic changes in the TMJ, but it is probably the result of (rather than the cause of) the osteoarthritic changes. Interestingly, when open bites are observed in children, they are rarely associated with TMJ symptoms. In the pediatric population, the majority of observed open bites represent a developmental jaw deformity rather than a result of osteoarthritis. Nevertheless, it is recommended that, when either a child or an adult is found to have an anterior open bite, radiographic analysis of the condylar head should be undertaken to check for osteoarthritic changes.
Orthodontic Treatment and Its Effects on Temporomandibular Disorders
Review of the Literature
The relationships among malocclusion, orthodontic treatment to improve the occlusion, and the effects on TMD is discussed frequently in the literature.* A spectrum of orthodontic treatment philosophies has been championed by individual practitioners on the basis of presumed effects on TMD. The longitudinal nature of orthodontic treatment, which is often carried out over several years, means that a changing TMD history would also be expected in a control group that is not simultaneously undergoing orthodontic treatment. Therefore, the occurrence of joint noise (e.g., popping, clicking) or myalgia (i.e., masticatory muscle discomfort) during orthodontic treatment may either be the result of the treatment or consistent with the natural history of the untreated individual.
Sadowsky and colleagues reported on 75 adult study patients who had undergone orthodontic treatment with full appliances during adolescence at least 10 years earlier.290 The treated group was compared with a group of 75 similar adults with untreated malocclusions. The authors also went on to increase both their control and subject groups and to report these additional findings several years later.291 In the two sequenced studies, respectively, 15% to 21% of the treated subjects presented with one or more signs of TMD (e.g., joint noise), and 29% to 42% had at least one or more symptoms of TMD. There were no statistically significant differences between the treated and untreated (control) groups.
Larsson and colleagues evaluated 23 individuals who had undergone orthodontic treatment during adolescence at least 10 years earlier.172 Mild TMD was recorded in 8 out of 23 (35%) of the patients, whereas only 1 (4%) had severe TMD. The authors compared this with published epidemiologic controls and stated that there was no difference in the incidence of TMD in the treated group versus the control group.
Dahl and colleagues examined 51 subjects 5 years after the completion of orthodontic treatment and compared them with an untreated control group.54 The authors found no statistical differences in TMD between the two groups. The number of subjects in both groups who had at least one mild TMD symptom was relatively high (70% in the treated group versus 90% in the untreated group). Mild symptoms (e.g., joint noise), masticatory muscle fatigue, and stiffness in the lower jaw were frequently observed in both groups.
A study by Smith and Freer examined 87 individuals who were treated with full orthodontic bracketing during adolescence.320 The treatment group (N = 87) was compared with an untreated control group (N = 28). Four years after treatment ended, TMD symptoms were found in 21% of the treated group and 14% of the control group; this was not found to be statistically significant. The one symptom that was statistically more common in the treatment group was a “soft click” (64% of the treated group versus 36% of the untreated group).
Rendell and colleagues examined 462 individuals (90% adolescents and 10% adults) who were undergoing orthodontic treatment in a graduate orthodontic dental school clinic.267 With the use of a modified Helkimo Index, only 11 of the patients presented with TMD signs or symptoms before treatment. Of the other 451 patients, during the 18-month study, none developed TMD signs or symptoms. For those with preexisting TMD signs or symptoms (N = 11), there was no consistent change in the level of pain or dysfunction reported during treatment.
Kremenak and colleagues reported pretreatment and posttreatment TMD examination data from 109 patients who were treated with full orthodontics.166,167 The Helkimo Index scores were also compared. No statistically significant differences were noted between the subjects’ pretreatment and posttreatment scores. Ninety percent of the patients had Helkimo Index scores that either remained the same or improved, and 10% of the treated patients had scores that worsened. The authors concluded that the orthodontic treatment provided to their patients was not an important etiologic factor for the development of TMD.
Hirata and colleagues examined 102 individuals before and after orthodontic treatment for signs and symptoms of TMD.128 They compared their treatment group with 41 untreated controls who were matched for age. The incidence of TMD for the treatment and control groups was not statistically significantly different.
Orthodontic Treatment Undertaken Specifically to Relieve Temporomandibular Disorders
In everyday dental practice, the establishment of a preferred intra-arch morphologic relationship of the teeth and then the achievement of a satisfactory inter-arch relationship of the teeth in one jaw to those in the other jaw (i.e., occlusion) serves as the basis of treatment objectives. According to a review of the literature, the establishment of a “normal” occlusion through orthodontic mechanics or via other dental means carried out for the purpose of eliminating or preventing the worsening of TMD does not seem warranted. Pullinger and Seligman have stated five potential exceptions to this, which were described previously in this chapter.255–261 McNamara and colleagues also stated that prudent basic dental treatment objectives will generally include the establishment of the six keys to ideal occlusion as advocated by Andrews, when feasible; the establishment of a limited CR–CO slide (i.e., <2 mm); the limiting of an anterior open bite; the alleviation of significant overjet (i.e., >6 to 7 mm); the limiting of unilateral maxillary lingual crossbites in children; and the establishment of a stable posterior occlusion.
Orthodontic Treatment Undertaken Specifically to Prevent Temporomandibular Disorders
The literature also contains studies that suggest that specific orthodontic maneuvers are effective for the prevention of TMD. The studies by Magnusson and colleagues187–192 and the study by Egermark and colleagues89 suggest preventative TMD advantages related to orthodontic occlusal corrections. At 5 and 10 years, these investigators reevaluated a group of 402 children and adolescents who had originally undergone a full course of orthodontic treatment. The Helkimo Index was used to measure clinical signs of TMD in the now older age group (i.e., ≥25 years old). Interestingly, the Helkimo Index outcome was lower in those who had undergone orthodontic treatment as compared with the control group. The studies by Dahl and colleagues and Sadowsky and colleagues also demonstrated a trend (although not a statistically significant one) toward the decreased prevalence of TMD signs and symptoms in orthodontically treated patients.53,290,291 These studies would require further confirmation before accepting them as credible indications of a cause-and-effect relationship.
Summary of Effects of Orthodontic Treatment on Temporomandibular Disorders
McNamara, Seligman, and Okeson summarize their understanding of the relationship between orthodontic treatment and TMDs as follows203:
1. Signs and symptoms of TMD do occur in healthy individuals.
2. Signs and symptoms of TMD increase with age, particularly during adolescence.
3. Orthodontic treatment performed during adolescence generally does not increase or decrease the odds of developing TMD later in life.
4. The extraction of teeth as part of an orthodontic treatment plan does not increase the risk of TMD.
5. There is no elevated risk for TMD associated with any particular type of conventional orthodontic mechanics.
6. Although a stable occlusion is a reasonable orthodontic treatment goal, the inability to achieve a specific gnathologic ideal occlusion does not result in TMD signs or symptoms.
7. No specific method of TMD prevention has been demonstrated to be effective.
8. When more severe TMD signs and symptoms are present, simple forms of treatment can alleviate them in most patients.
A summary of evidence-based systematic reviews of TMDs was carried out by Rinchuse and McMinn.283 Their systematic review resulted in the following conclusions:
1. Occlusion, which was once considered the primary and sole cause of TMD, now at best is recognized as having a secondary role in causing it.
2. Conventional orthodontic treatment that improves the occlusion does not cause TMD.
3. The use of occlusal adjustments in orthodontic patients has no evidence-based support for the treatment of TMD.
4. There is evidence-based support for the use of occlusal splints and biofeedback for the treatment of TMD.
Association of Jaw Deformities, Orthognathic Surgery, and Temporomandibular Disorders
Review of the Literature
The association of a jaw deformity with malocclusion and the effects of orthodontic and surgical correction on TMD signs and symptoms have been examined in clinical studies for the past several decades.* The quality of the research and therefore the value of the conclusions vary. There are just three longitudinal prospective controlled clinical trial studies that have been carried out to assess the effects of orthognathic surgery on TMD: the studies by Onizawa and colleagues,232 Panula and colleagues,236 and Dervis and colleagues.67
The study by Onizawa and colleagues sought to evaluate changes in the symptoms of TMD after orthognathic surgery.232 TMJ symptoms in preoperative orthognathic patients (N = 30) were compared with those of healthy control volunteers (N = 30). Changes in TMD symptoms were evaluated in both groups at 3- and 6-month postoperative intervals. The authors found no significant differences in the incidence of TMJ sounds, deviation of mouth opening, or tenderness on direct palpation of the TMJ and masticatory muscles between patients who were scheduled to undergo orthognathic surgery and control volunteers. The treatment group did not report TMJ symptoms significantly more often than the control subjects. At both the 3- and 6-month postoperative intervals, half or more of the treatment group showed no change in TMJ sounds, deviation of mouth opening, or tenderness on palpation of the TMJ or masticatory muscles. At each evaluation time frame, some individuals in both the control group and the study group exhibited improvement in TMJ symptoms, whereas others showed a change for the worse. Findings of postoperative TMJ sounds were observed to be associated with a reduction of mandibular mobility (i.e., mouth opening). The authors concluded that TMD symptoms did not always show improvement after surgical correction and that, for some patients, the symptoms changed for the worse.
Panula and colleagues carried out research to study the effects of orthognathic surgery on TMJ dysfunction.236 They completed a prospective follow-up study to examine the influence of orthognathic procedures for the correction of dentofacial deformities on signs and symptoms of TMJ dysfunction. Sixty consecutive patients with dentofacial deformities were examined preoperatively and then twice after orthognathic surgery. The Helkimo Anamnestic and Dysfunction Indices were also given as a questionnaire, and the results were used as part of the determination. The prevalence of headache was also assessed. The average follow-up was 4 years after the initial preoperative examination. A group (N = 20) with a similar type and grade of dentofacial deformity who elected not to undergo surgical correction or any other occlusal therapy served as the control group. The majority of the treatment group (73%) was found to have signs and symptoms of TMJ dysfunction or TMD during the preoperative examination. At the final postsurgery examination (i.e., 4 years after surgery), the prevalence of TMD had been reduced to 60%. There was also a dramatic improvement in the prevalence of headache, which was initially experienced by 63% of patients and reduced to 25% of patients at the final visit. The authors concluded that signs and symptoms of TMD, including pain (headache) levels, could be reduced with orthognathic treatment. The risk of an orthognathic patient experiencing new TMD was extremely low. No association could be shown between TMD and any specific type or magnitude of dentofacial deformity.
A study was conducted by Dervis and colleagues with the objective of looking at the long-term prevalence of TMD in individuals with a dentofacial deformity who then underwent orthognathic surgery as compared with a control group.67 Signs and symptoms of TMD in both the dentofacial deformity patients and the control group were evaluated before surgery, 1 week after release of intermaxillary fixation, and 1 and 2 years after surgery with the use of the Helkimo Anamnestic and Dysfunction Indices. At both the initial preoperative examination and the final examination (i.e., 2 years after surgery), signs and symptoms of TMD in the patients who were undergoing orthognathic surgery were compared with those of healthy control subjects. The lengths of condylar pathways during opening and with lateral and protrusive movements were also evaluated with the use of axiography. A statistically significant reduction of TMD symptoms and signs 2 years after surgery as compared with before surgery was found. Interestingly, at the initial examination, the patients with dentofacial deformities who were scheduled to undergo orthognathic surgery did not report TMD signs and symptoms with a greater frequency than other healthy control subjects. At the final examination (i.e., 2 years after surgery), greater improvements in TMD symptoms in the patients who had undergone orthognathic surgery were found as compared with healthy control subjects. The authors also found a statistically significant decrease in masticatory muscle tenderness after surgery. The authors concluded that the “functional status” of the TMJ can be improved with orthognathic surgery. There was no clear association between TMD symptoms and a specific type or pattern of dentofacial deformity.
When comparing and contrasting the three published longitudinal prospective controlled studies that were conducted to determine the effects of orthognathic procedures on TMD symptoms and signs (i.e., Onizawa and colleagues,232 Panula and colleagues,236 and Dervis and colleagues67), several observations can be made:
1. Patients with dentofacial deformities who were scheduled to undergo orthognathic surgery were not found to have significant differences in their TMD signs and symptoms as compared with patients in the control groups.
2. After orthognathic surgery and orthodontics, signs and symptoms related to TMD were frequently improved.
3. Despite the trend for diminished signs and symptoms of TMD after orthognathic surgery and orthodontics, individuals did not always show improvement; for some, the symptoms changed for the worse.
4. After orthognathic surgery and orthodontic treatment, a decrease in masticatory muscle tenderness was frequent. A decrease in joint tenderness on palpation was also a common occurrence.
5. In one of the three studies reviewed, a decrease in maximum mouth opening was observed, but this was not found to be of clinical importance.
Karabouta and colleagues reviewed 280 individuals with different patterns of mandibular deformities (e.g., prognathism, retrognathia, open bite, asymmetry) who underwent orthognathic surgery that included sagittal split ramus osteotomies of the mandible. Before surgery, the patients were found to present subjective or objective TMJ dysfunction symptoms with an incidence of 41%.154 After surgery, the incidence of such symptoms in the same patients was reduced to 11%. Individuals with no preoperative TMJ dysfunction symptoms developed such symptoms with an incidence of 4% after surgery.
White and colleagues set out to review the prevalence of TMD in patients with dentofacial deformities who were undergoing orthognathic surgery.349 Preoperatively, 49% of their study group presented with TMD. After orthognathic surgery, in the symptomatic patients, 89% had improved temporomandibular function, 3% were unchanged, and 8% developed increased symptoms. Of the preoperative asymptomatic patients, 8% developed TMD after surgery. In the study group, TMD was significantly greater in patients with Class II skeletal deformities as compared with those with Class III tendencies. Overall, temporomandibular function generally improved in both treatment groups (i.e., Class II and Class III) after successful surgery.
Hori and colleagues reported three individual (non-consecutive) cases in which there was a worsening of preexisting TMJ dysfunction after sagittal s/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


