Restoration of the Single Implant
Implant Survival and Complications Data
Retaining the Soft Tissue and Interdental Papillae
At the conclusion of this chapter, the reader will be able to:
 . Understand the rationale for selecting an implant-supported single crown as a treatment option with awareness of the complications that can occur.
. Understand the rationale for selecting an implant-supported single crown as a treatment option with awareness of the complications that can occur.
 . Explain the design principles involved in the fabrication of an implant-supported single crown with consideration of the biomechanical factors involved.
. Explain the design principles involved in the fabrication of an implant-supported single crown with consideration of the biomechanical factors involved.
 . Describe challenges in retaining the soft tissue and interdental papillae and the guidelines suggested to minimize complications associated with the soft tissue around the dental implant.
. Describe challenges in retaining the soft tissue and interdental papillae and the guidelines suggested to minimize complications associated with the soft tissue around the dental implant.
 . Explain the concept of immediate implant placement and loading, different impression techniques, clinical considerations, and laboratory procedures involved in the fabrication of an implant-supported crown.
. Explain the concept of immediate implant placement and loading, different impression techniques, clinical considerations, and laboratory procedures involved in the fabrication of an implant-supported crown.
Implant Survival and Complications Data
In 2008 a systematic review determined the 5-year survival of single implants to be 96.8% and that of single crowns to be 94.5%.1 Despite these high survival rates, both biologic and mechanical complications have been reported.1 In fact, another systematic review concluded that crown complications are common.2
A literature review of clinical complications provided the following data on mechanical complications with single crowns attached to single implants: 20% of abutment screws loosened with early screw designs; 7% loosened with newer screw designs and the use of torque devices; and 2% of abutment screws fractured.3 The same literature review reported that 1% of implants fractured, but the data were related to all types of implant prostheses and were not specific to single crowns. However, multiple reports of implant fractures associated with single posterior implants have been published.
A third systematic review presented data from both short-term studies (6 months to 5 years) and long-term studies (5 to 10 years) of single crowns and fixed partial dentures.4 The long-term data on single crowns showed that abutment screw loosening ranged from 1% to 10% in the nine studies that provided data on abutment screw loosening with single crowns. Abutment screw loosening occurred with both external and internal abutment connections.
Design Principles
Rangert et al.5 evaluated the forces and moments that occur on Brånemark implants. Based on theoretical considerations and clinical experience with Brånemark implants, these authors presented guidelines for controlling the forces applied to implants. They recommended that the restoration not extend lateral to the implant more than approximately one implant diameter in the molar region and no more than two implant diameters in the incisor region.
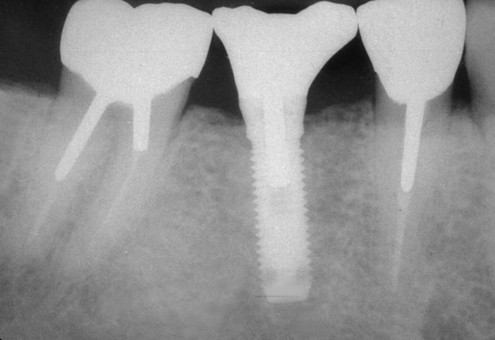
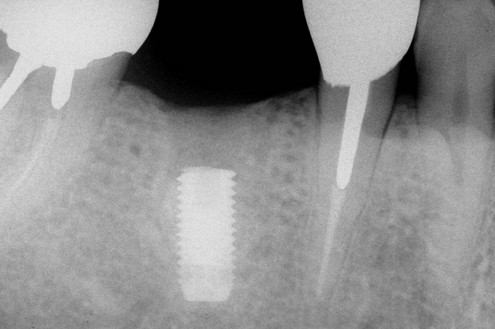
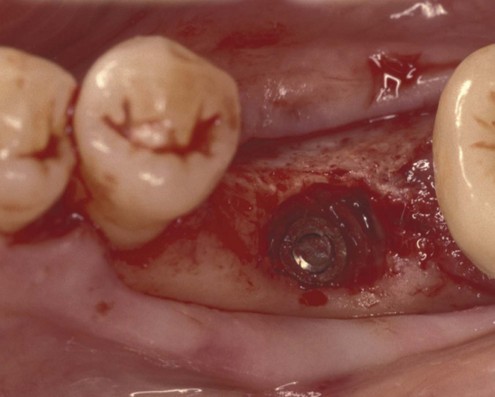
In another article, Rangert et al.6 discussed the probable causes of 39 implant fractures. All nine fractures of implants supporting single crowns occurred in the mandibular molar area (eight first molars and one second molar) (Figures 9-1 to 9-5). Several factors that result in adverse loads on implants were discussed, including:
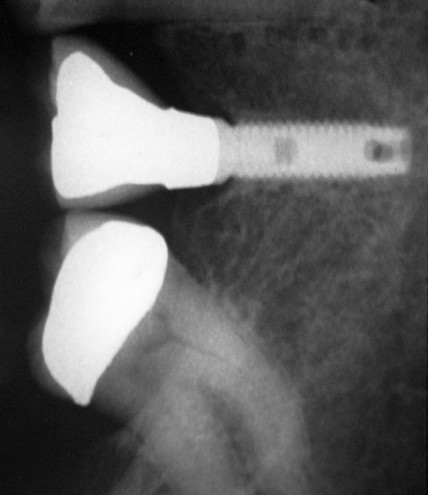
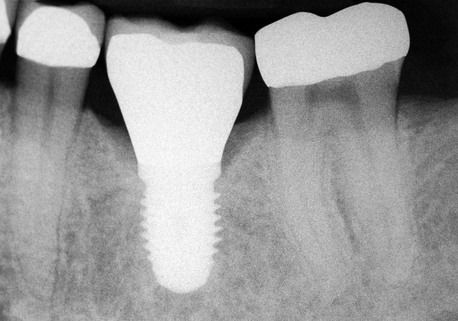
Figure 9-4 Radiographic image of the implant-supported crown made for the implant shown in Figure 9-3 that shows the mesial cantilever.
 Excessive height of the occlusal surface above the implant
Excessive height of the occlusal surface above the implant
 Deviation of the long axis of the implant from a perpendicular relationship to the occlusal plane
Deviation of the long axis of the implant from a perpendicular relationship to the occlusal plane
 Substantial differences between the dimension of the occlusal surface and the diameter of the implant
Substantial differences between the dimension of the occlusal surface and the diameter of the implant
Implant fractures are not common, and statistical differences in fracture rates based on location in the mouth have not been shown. However, Eckert et al.7 analyzed the incidence of fracture among 4,937 implants. They determined that the only implant fractures associated with single crowns occurred in molar areas. Based on the observation that single implant fractures were associated only with molar crowns, the authors stated, “Despite the lack of statistical significance, this clinical observation makes it appear prudent to consider the single implant–supported molar to be at a higher risk of fracture.”
Rangert et al.8 identified risk factors that increase the load applied to implants. The following factors related to implant single crowns: (1) extension of the occluding surface lateral to the implant; (2) increasing the distance between the occlusal surface and the implant; (3) use of one implant to support the replacement of a multi-rooted tooth; and (4) bruxism or the presence of heavy occlusal forces as evidenced by tooth wear/tooth structure fractures. When a molar is replaced using a single implant, the authors emphasized the importance of controlling occlusion so as to avoid heavy centric occlusal contact. They suggested light centric occlusal contact as a means of avoiding heavy contact.
Biomechanics
Anterior Biomechanics
In light of the guidelines set by Rangert et al.,5 a reasonable conclusion is that anterior implant single crowns can extend laterally a moderate distance beyond the periphery of the implant. This is possible because the maximum occlusal load in the anterior region of the oral cavity is less than the maximum load in the posterior region. Depending on the material used for fabrication of the implant, abutment, and retaining screw and the clamping force achieved when the retaining screw is tightened, an implant-supported crown can resist a specific load before the retaining screw deforms. The practitioner must understand the anticipated load that will be placed on the implant and limit the dimensions of the crown to prevent occlusal overload.
The average dimensions of anterior teeth are 5 to 8.5 mm mesiodistally and 6 to 8.3 mm faciolingually; therefore, adverse leverage is unlikely to be created by the mesiodistal or faciolingual dimensions of the crown. Biomechanical overload of an anterior crown is more likely to occur in an incisocervical dimension, because the distance from the top of the implant to the location of occlusal contact can be substantial, especially if the implant is placed deep below the soft tissue for esthetic reasons (Figure 9-6) or if a significant alveolar defect exists before implant placement.
If risk factors create the potential for implant overload, alterations in the incisal guidance and implant angulation in the bone may help reduce that risk.9
Posterior Biomechanics
If the previous recommendations about forces and moments5 are applied to posterior single crowns placed on implants, the conclusion is that the crown should not extend lateral to the implant more than one implant diameter. Therefore, for an implant 4 mm in diameter, the maximum lateral cantilever should be about 4 mm; this means that the crown should extend mesially, distally, facially, or lingually only 4 mm lateral to the implant.
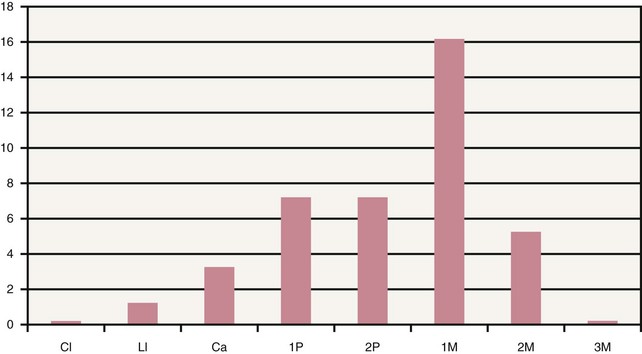
Figure 9-7 documents the relative number of fractures found by Rangert et al.6 for implants located in different sites. Biomechanical overload is more likely if a single molar implant is not centered under the crown. In addition, the possibility of overload increases as the distance from the occlusal surface to the implant increases. The combination of a tall crown and an implant that is not centered beneath it compounds the potential for overload.
Weinberg and Kruger10 mathematically compared four clinical variables that can affect torque production and implant loading: (1) cuspal inclination, (2) implant inclination, (3) horizontal implant offset, and (4) apical implant offset. A knowledge of these factors can help the practitioner design crowns that transfer more favorable forces to the implant system. Cuspal inclination and horizontal implant offset have the greatest effect on torque, and implant inclination and apical implant offset have a lesser impact. The effects are as follows:
 For every 10-degree increase in cuspal inclination (steepness), torque increases approximately 30%
For every 10-degree increase in cuspal inclination (steepness), torque increases approximately 30%
 For every 1 mm of horizontal offset (i.e., the implant is not centered beneath the occlusal surface of the crown), torque increases approximately 15%
For every 1 mm of horizontal offset (i.e., the implant is not centered beneath the occlusal surface of the crown), torque increases approximately 15%
 For every 10-degree increase in implant inclination relative to the angle of applied occlusal force, torque increases approximately 5%
For every 10-degree increase in implant inclination relative to the angle of applied occlusal force, torque increases approximately 5%
 For every 1 mm increase in the vertical implant offset (i.e., the distance from the occluding surface to the implant, also known as the crown-to-implant ratio), torque increases approximately 5%
For every 1 mm increase in the vertical implant offset (i.e., the distance from the occluding surface to the implant, also known as the crown-to-implant ratio), torque increases approximately 5%
Implant Location and Alignment
In esthetically critical locations, a faciolingually centered position is preferred when existing bone dimensions permit. Lingual positioning of the implant produces a crown with deficient facial cervical contour or one in which porcelain must overlap the facial soft tissue to create the desired cervical crown morphology. The overlapping makes oral hygiene more difficult and will not be esthetically pleasing if the soft tissue recedes apically. Conversely, if the implant is placed too far facially, the facial bone becomes thin and subsequent remodeling may result in soft tissue recession and/or gray discoloration of the overlying soft tissue. Placing an implant too far facially can create such a substantial esthetic challenge that the implant may have to be removed, bone grafting performed, and another implant subsequently placed in a more favorable position (Figure 9-8).
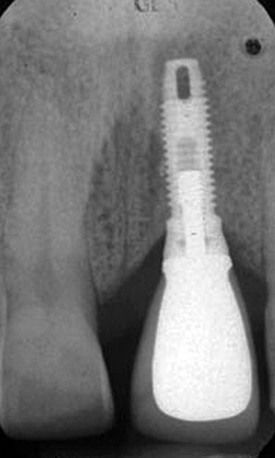
The incisocervical/occlusocervical location of the implant is largely determined by the location of existing bone (Figure 9-9) and the esthetic need to transition from a smaller diameter round form to a larger diameter form with a different geometric perimeter. Typically, implants have been placed apical to the cementoenamel junction of adjacent teeth to permit the required changes in morphology to occur somewhat gradually. While an early textbook11 recommended that implants in the esthetic zone be placed 4 mm or more apical to the cementoenamel junctions of adjacent teeth, it is currently felt that implants should not be positioned this deep but should be located so the implant platform is approximately 3 mm apical to the predetermined midfacial margin of the mucosa.
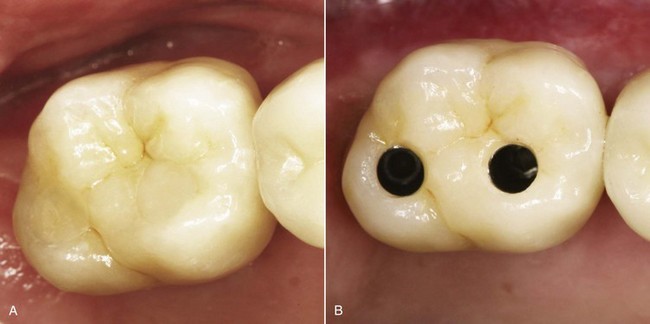
Methods of Compensating for Potential Overload
In some cases, because of the position or dimensions (or both) of the residual bone in the edentulous area, implants cannot be placed in an ideal location. In such cases bone grafting should be used to enhance the location of the implant. If grafting is used and a positional deficit remains, or if grafting is not possible because of the patient’s choice or the added expense, compensatory designs should be used to reduce the overload potential. These design modifications are particularly important with molar implants because of the higher overload potential as a result of heavier occlusal forces and larger crown dimensions. Methods of overload compensation with molar implants include narrowing of the occlusal table, use of wider diameter implants (5 or 6 mm) (Figure 9-9), or use of two implants to support one molar crown (Figure 9-10 A, B).12
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses