Implant Placement with Simultaneous Guided Bone Regeneration
At the conclusion of this chapter, the reader will be able to:
 . Explain the basic clinical and radiographic evaluation of a potential implant patient
. Explain the basic clinical and radiographic evaluation of a potential implant patient
 . Understand the advantage of three-dimensional tomography
. Understand the advantage of three-dimensional tomography
 . Describe the benefits of flapped implant placement
. Describe the benefits of flapped implant placement
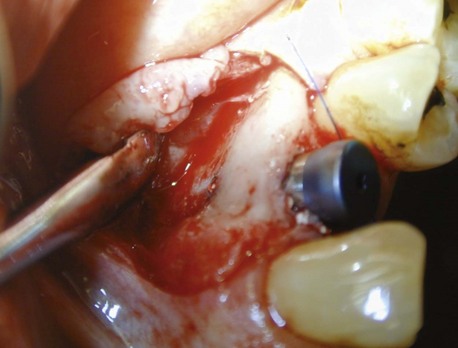
 . Explain proper flap design and the importance of adequate periosteal release
. Explain proper flap design and the importance of adequate periosteal release
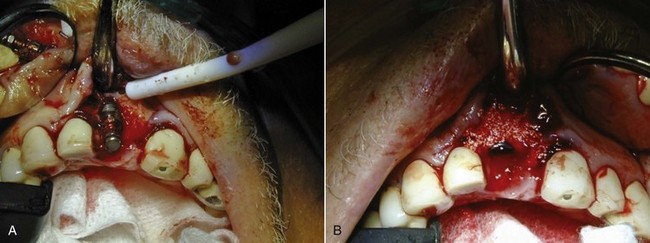
Since the first report of dental implant placement in a fresh extraction socket, interest in this concept of immediate tooth replacement has grown.1–3 However, tooth removal is often accompanied by varying degrees of loss of alveolar bone. If not corrected, this loss tends to impede the ideal positioning of a dental implant replacement. Fortunately, this deficiency can be successfully overcome through the use of barrier membranes and bone grafts for guided bone regeneration (GBR). The GBR procedure can be performed before or at the time of dental implant placement to preserve the width and height of the existing alveolar ridge or to regain volume that was previously lost (Figure 7-1).
Criteria for Simultaneous Implant Placement and Guided Bone Regeneration
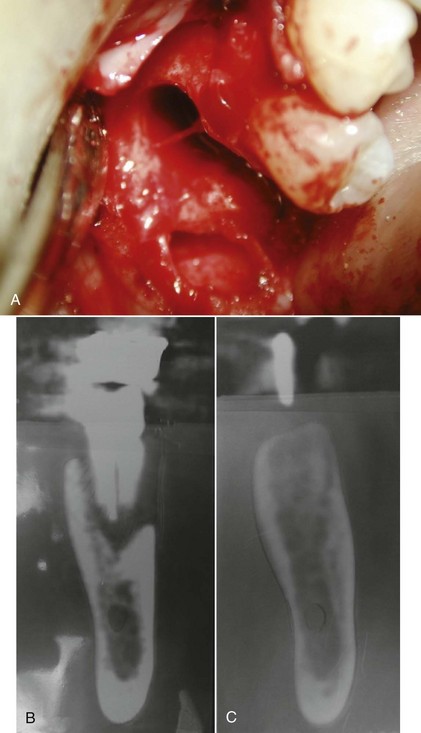
During the clinical examination for implant placement, the dental practitioner may encounter horizontal, vertical, and intraalveolar bone defects (Figure 7-2). These are common, and they are therapeutically important. The practitioner can choose either to perform GBR simultaneously with implant placement or to use a staged approach.

Figure 7-2 Clinical view of a bony defect.
As mentioned, primary implant stability in a position to meet the high demands of esthetics and function must be achieved during implant placement to have successful osseointegration. Brånemark et al.,4 Albrektsson et al.,5 and Buser have described the importance of primary stability as a prerequisite for osseointegration during the initial healing period.
Correct three-dimensional placement, both in position and in direction (mesiodistal and buccolingual), is important to achieving esthetics and function. This principle was introduced by Garber and Belser,6 who found that in any restoration or natural tooth, the surrounding soft tissue profile played an integral role in the final esthetics. Similarly, in implant restorations, merely attaching a prosthetic device to the underlying fixture is no longer sufficient; for optimal esthetics, it is essential to reconstitute the implant site in a three-dimensional approach. This invariably involves redevelopment or replacement of lost hard tissue and redevelopment of the correct soft tissue profile so that the implant can be placed in the desired position, as determined by the restoration, while the soft tissue profiles are generated by the actual form and contours of the prosthetic device. As a general rule, the implant should be placed along the palatal wall of the extraction socket in the maxilla and toward the buccal side in the mandible.
Bone morphology to achieve predictable bone regeneration of the defect around the implant is another important determinant for performing GBR. Bone defects may be classified as vertical, horizontal, and intraalveolar. Numerous studies have shown that treatment of this type of defect is highly predictable. Horizontal bone defects include dehiscence (Figure 7-3) and fenestration (Figure 7-4). With a facial osseous dehiscence defect, the shape and size of the defect determines the predictability of the GBR procedures.7 A variety of graft materials, barrier membranes (both reabsorbable and nonreabsorbable), and techniques have been used for bone augmentation or grafting.8 It has been shown that new bone formation depends mainly on the surface area of the exposed bone and its marrow cavity. The periodontal literature has shown that the most important local factor in regeneration is the ratio between the surface area of exposed bone and the defect volume. Sculean et al.9 noted that the more bone wall available in a defect area, the better and more predictable the regeneration outcome. These authors concluded that no additional benefits of combination treatments (graft and barrier membrane) were detected in models of three-wall intrabony defects. However, in supraalveolar and two-wall intrabony (missing buccal wall) defect models of periodontal regeneration, combination of grafts and barrier membrane results in superior bone repair.
The established method adopted from periodontal regeneration9/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 .
.