Part 3: Radiological pathology of the jaws
Chapter 9
Radiolucencies
Introduction
A radiolucency is the black or darker area on a conventional radiograph. It suggests an osteolytic process, particularly when it presents in bone. Most lesions associated with this process remain radiolucent, whereas some subsequently acquire a central opacity or opacities or eventually become completely radiopaque. The latter are more fully addressed in Chapter 10.
The flowcharts are based on the best evidence, either from recent systematic reviews or, where they are lacking, traditional narrative reviews or recently reported large case series. As seen, particularly in Figures 9.1–9.4, it generally flows from the most important clinical and radiological findings, addressing systemic lesions and malignancies first and then cysts and benign neoplasms. These flowcharts focus on the most common and important lesions and are not exhaustive with regard to the rarer lesions, particularly if they respond well to the initial treatment—i.e., do not recur.
Figure 9.1. Radiolucencies occurring within the bony jaws.
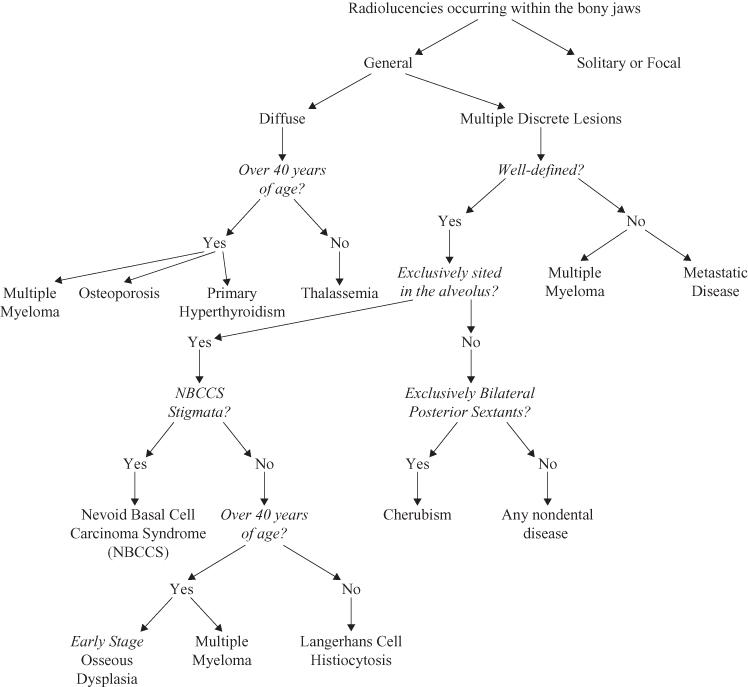
Figure 9.2. Radiolucencies occurring within the bony jaws; solitary or focal lesions.
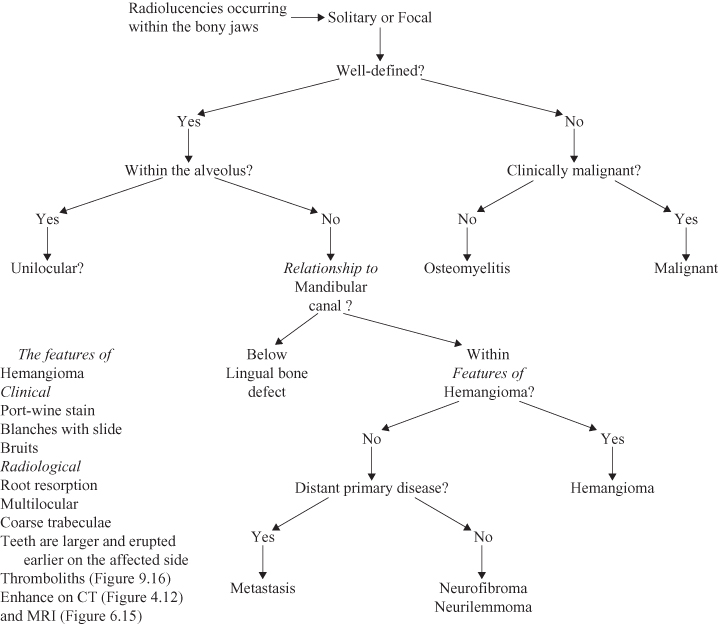
Figure 9.3. Radiolucencies occurring within the bony jaws; unilocular lesions
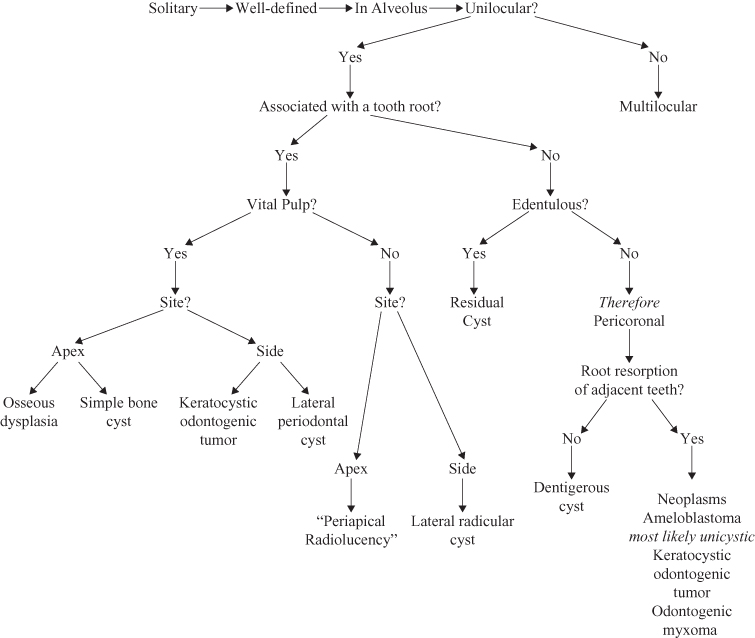
Figure 9.4. Radiolucencies occurring within the bony jaws; multilocular lesions.
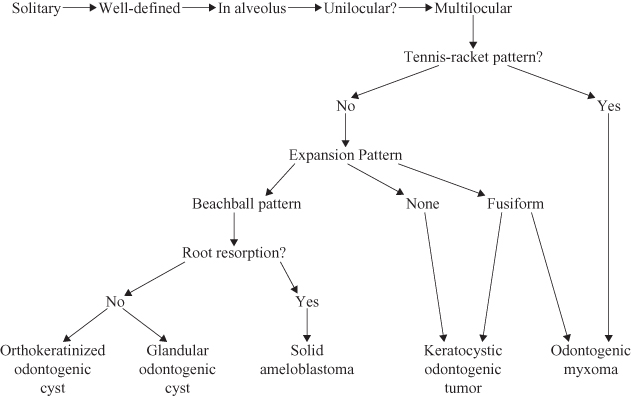
Multiple radiolucencies, particularly if they are distributed throughout the jaws suggest a systemic cause, whereas the single radiolucency suggests a local cause.
The degree of marginal definition is crucially important to determine potentially serious disease. If it is well defined, the radiolucency is more likely to be benign; it is likely to be a benign neoplasm or a cyst. A poorly defined radiolucency on the other hand could represent a malignancy or infection.
Locularity is essentially a feature of radiolucencies; most are either unilocular or multilocular. It is important to differentiate between multilocular and scalloped radiolucencies because the latter is a variant of a unilocular radiolucency. Although unilocular radiolucencies are more likely to be odontogenic or simple bone cysts, multilocular radiolucencies almost always are odontogenic neoplasms. Nevertheless, the early, and therefore the dimensionally small, stage of some odontogenic neoplasms may present as a unilocular radiolucency. The multilocular radiolucency could be characterized according to three patterns. Although the soap-bubble and honeycomb would appear to be nonspecific, the tennis racket is virtually pathognomonic of the odontogenic myxoma.
The radiolucency’s relationship to mandibular canal or the image of the hard palate (on panoramic or cephalometric radiographs) indicates whether it is likely to be of odontogenic origin. If the radiolucency is above the mandibular canal or below the image of the hard palate, it is within the dental alveolus and therefore likely to be of odontogenic origin. If the radiolucency is sited within the alveolus, its relationship to teeth is important to further refine the differential diagnosis. An association with the root of an erupted tooth, particularly if it has a large carious lesion or a large restoration, suggests the possibility of a necrotic pulp, and then the radiolucency is likely to have an inflammatory cause. If the radiolucency is associated with the crown of an unerupted tooth, a dentigerous cyst or an odontogenic neoplasm (assuming a secondary relationship to it) should be considered.
Lesions that commonly present as well-defined radiolucencies are cysts and neoplasms. Cysts are common and the majority are inflammatory. Almost all true cysts and most benign neoplasms expand by hydrostatic pressure and are therefore frequently spherical or nearly spherical in shape. This shape is achieved in larger cysts and neoplasms by displacing the buccal and lingual cortices and presenting as buccolingual expansion. Odontogenic lesions, arising within the alveolus, if sufficiently large will displace the mandibular canal downward. Additionally, all lesions can reduce the diameter of the canal or can completely erode its cortex (so that it is no longer visible) if they are enveloping it.
The effect of the radiolucency on the adjacent teeth or anatomical structures is important. This effect is manifested by either displacement or erosion. The latter when applied to teeth, particularly their roots, is termed root resorption. Although all lesions presenting as radiolucencies may in due course cause root resorption, this would appear to be a particular feature of certain odontogenic neoplasms. Displacement of teeth and buccolingual cortices are universal to all expansile lesions.
Giant cell lesions and hemangiomas each have an extensive range of presentations. As a result they appear in the differential diagnosis of several lesions.
Some lesions that are generally understood to be radiopaque, may appear initially as radiolucencies in their earliest stage. This apparent inconsistency is analogous to the clearing of a building site and first excavating to establish the foundations of the new building to be erected.
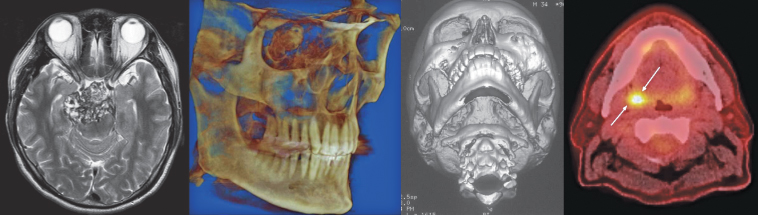
In addition to conventional radiography, advanced imaging modalities such as computed tomography (CT) and magnetic resonance (MRI) are frequently used to investigate jaw lesions. Although osteolytic lesions and structures are still “black” on bone-window images made by either helical computed tomography (HCT, see Chapter 4) or cone-beam computed tomography (CBCT, see Chapter 5), they appear “white” on soft-tissue window HCT (see chapter 4) and MRI (see Chapter 6). Furthermore they may enhance with iodine-based or gadolinium intravenous contrast for HCT and MRI, respectively.
The term significant will be used only when the feature it is qualifying is P <0.05.
Artifacts causing radiolucencies arise from three main sources, image development, normal anatomy and variants, and earlier treatment. Because these have already been addressed in other texts, they will not be considered further.
Multiple Radiolucencies
An early consideration in the review of the clinical and radiological findings is whether the patient is suffering from a generalized or systemic condition or whether it is of a local nature. Generalized disease can manifest itself in the context of radiolucencies by a generalized osteopenia—a reduction in trabeculae, both in their number and thickness, and thin cortices.
THALASSEMIA
In younger patients, generally of Mediterreanean, Middle Eastern, and South Asian extraction, such a presentation may be indicative of thalassemia, the most common genetic disease. The classical features of thalassemia are hair-on-end appearance of the vault of the skull, obliteration of the air-sinuses and replacement of the normal trabecular pattern by fewer coarse straight trabeculae (Figure 9.5; see also Figures 11.6 and 17.22 for other images of the same patient).
Figure 9.5. A lateral projection of the skull and a panoramic radiograph of thalassemia. (a) The lateral projection of the skull displaying typical radiological features of thalassemia; hair-on-end appearance of vault of skull, completely obturated air-sinuses (the frontal, ethmoidal sphenoidal, and maxillary). The mandible is also affected. (b) Panoramic radiograph exhibiting few, but coarse and linear, trabeculae within the enlarged mandible.
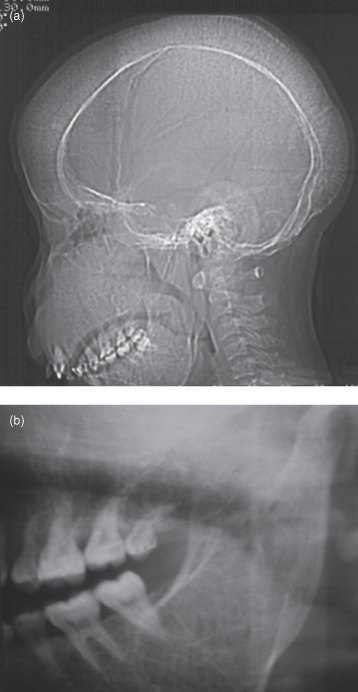
The conventional radiological features of thalassemia affecting the jaws were reported in a Middle Eastern community by Hazza et al.1,2 The maxillary antrum was obliterated in every case (see Figure 11.6). The teeth displayed “spiky” roots, an increased crown/root ratio, a reduction in the lamina dura and taurodontism. In addition the teeth display some delay in their development.
Thalassemia has not only a specific presentation upon diagnosis but also subsequently according to the mode of treatment. Hypertransfusions and chelating agents also affect changes in both the skeleton and the extraskeletal organs,3 which may be observed by radiology.
SICKLE CELL DISEASE
Although sickle cell disease is most frequently found among West Africans and their Afro-Caribbean and African-American descendants it is also found among Mediterranean and Middle Eastern communities. White et al.4 reported that its detection by fourier analysis is more effective than counting struts. Fourier analysis revealed increased trabecular spacing in sickle cell disease.5
MULTIPLE MYELOMA
Multiple myeloma is a plasma cell malignancy. Its most frequent manifestation is that of widespread disseminated disease. The multiple radiolucencies affecting the vault of the skull classically confers a pepper-pot appearance (see Figure 18.1). Ninety percent of patients develop bone lesions, making it the most common cancer to affect bone.6
It accounted for 43% of all bone malignancies in one report’s patient database.7 Although the jaws are affected in 30% of cases, 16% of multiple myeloma first manifest in the jaws.7 Generally whole-body scanning is achieved by PET-CT (see Chapter 7) using 18 fluorodeoxyglucose (FDG) rather than technetium 99 m.6 Sixty percent of patients develop pathological fractures.6
Observation of solitary osseous plasmacytoma (SOP) in a radiograph of the jaws may enhance the patient’s prognosis by earlier local treatment prior to it becoming widespread disease. Seventy percent of cases, if untreated, progress to multiple myeloma. Thirty percent progress to multiple osteolytic (radiolucent) lesions without marginal sclerosis; in other words they present the classical “punched-out” radiolucent presentation of multiple myeloma going onto diffuse osteoporosis and finally diffuse osteosclerosis.8 Witt et al. declared that neither diffuse osteoporosis nor diffuse osteosclerosis was observed in their case series.8 Half of the SOPs affecting the jaws were observed on radiographs, they were radiolucent.8 Pisaro et al. reported plasmacytoma of the oral cavity frequently appeared superimposed upon the roots of adjacent teeth and were accompanied by pain and a raised red mucosal lesion on the alveolar ridge. They need to be distinguished from a periapical radiolucency of inflammatory origin.9
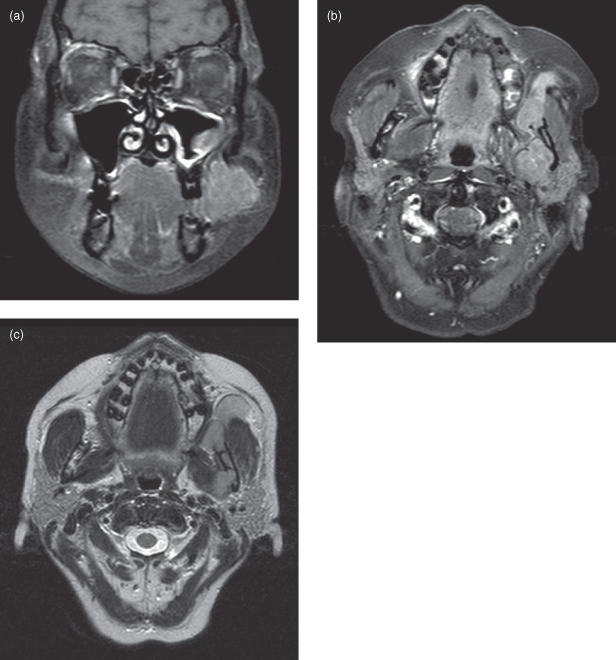
The literature emphasizes multiple myeloma’s widespread manifestation of the skeleton. Nevertheless, it should be appreciated that this multisystem disease also affects soft tissues as made obvious by the MRI images of Figure 9.6a–c.
Figure 9.6. Magnetic resonance imaging (MRI) of a case of multiple myeloma. See Figure 18.1 for a lateral conventional radiograph of the skull displaying the salt-and-pepper pattern or pepper-pot pattern skull. (a) Coronal T2-weighted magnetic resonance imaging (MRI) displays the neoplasm as a mass within the buccal tissues. It has a heterogeneous hyperintensity within it. The mucosa of the ipsilateral maxillary antrum is very hyperintense, suggestive of sinusitis. The lateral exophytic mass is suggestive of the neoplastic invasion. There is also a hyperintense area within the bone marrow superolateral to the contralateral orbit, the cortex is absent, and the lesion is in continuity with a hyperintense lesion within the orbit. This is suggestive of multiple lesions. (b) Axial T2-weighted magnetic resonance imaging (MRI) displays the neoplasm as a mass within the buccal tissues. It is more hyperintense that the adjacent isointense masseter around whose anterior margin it expands into the deep tissues of the cheek displacing the parotid duct and the subcutaneous tissues outward. The posterior aspect of the lesion abuts the deep pole of the left parotid gland. The neck of the condyle appears substantially eroded. The ipsilateral lateral pterygoid muscle has been substantially infiltrated. (c) Coronal (non–fat-saturated) T1-weighted magnetic resonance imaging (MRI) displays the neoplasm as a mass within the buccal tissues. It appears more isointense in contrast to the more hyperintense fat tissues. Although it is clearly distinguished form the parotid gland the lingual cortex of the base of the neck of the condyle is absent suggesting its infiltration of the marrow space. The attachment of the ipsilateral lateral pterygoid to the neck of the condyle has been completely infiltrated.
Figure courtesy of Dr. Montgomery Martin, British Columbia Cancer Agency.
LANGERHANS CELL HISTIOCYTOSIS
Ninety percent of Langerhans cell histiocystosis (LCH), formerly called “histiocytosis X,” is present in individuals younger than 40 years of age; the mean age is 19 years.10 Dagenais et al.11 were the first to identify and qualify the radiological features of LCH affecting the jaws. They reported that almost all cases affected the posterior sextant of the mandible and in a third of cases also affected the posterior sextant of the maxilla. They found that almost all cases presented as circular or elliptical radiolucencies (Figure 9.7). Although most were well defined, particularly those affecting the alveolus, a cortex or sclerosis was generally observed only in that part of the lesion close to the alveolar crest. Those in the alveolus were multiple, whereas those in the basal process were solitary. The majority of the alveolar lesions were sited about the apices. The lamina dura was absent. Root resorption though common was slight. Although periosteal new bone was observed on occlusal radiographs of lesions affecting the basal process, buccolingual expansion was not observed, except for involvement of the condyle and coronoid processes. Their report, largely consistent with most earlier literature, did not mention “floating teeth,” perhaps because almost all their lesions were small, not one case presented with such a feature. Tooth displacement was observed in one-half of cases.10
Figure 9.7. Panoramic radiograph of Langerhan’s histiocytosis. There are two well-defined radiolucencies in the posterior mandible superimposed upon the mandibular canal. The more distal radiolucency is more translucent and the mandibular canal appears not only widened but does not exhibit the canal’s superior or inferior cortex. Its margin is delimited by some sclerosis. The mesial radiolucency’s mesial border has the contralateral lower border of the mandible superimposed upon it.

OSTEOPOROSIS
Osteoporosis is a serious disease, but can be treated if detected early, thus avoiding a hip fracture, which, in the elderly, can be fatal.12 Not only is osteoporosis most frequently observed in postmenopausal women, in which it is most severe, it also affects men.13 A radiological diagnosis of osteoporosis may be readily determined from examination of the thickness of the lower border of the mandible on a panoramic radiograph. This has been simplified even more and can now be applied to the trabecular pattern on intraoral radiographs.14 This can be achieved visually.15 The Osteodent research project has recently indicated that dentists now can have a role in the detection and referral of patients with osteoporosis.12
HYPERPARATHYROIDISM
The radiology of hyperparathyroidism affecting the jaws, in addition to generalized bone resorption, osteopenia, and osteosclerosis, may reveal localized lesions. These are “brown tumors” and are rarely reported. They may appear either as radiolucencies or leontiasis ossea (discussed further in Chapter 10). A brown tumor presenting as a radiolucency is displayed in Figure 10.9b.
There are three types of hyperparathyroidism, and they all have their effects by disrupting normal calcium homeostasis.16,17 The most common type is primary hyperparathyroidism, which presents as a disease in middle- to old-aged patients, principally women. Its most common cause is a secreting adenoma arising in one of the 4 parathyroid glands. Occasionally, a secreting carcinoma can cause it.18
The secondary type frequently is secondary to chronic renal insufficiency (CRI)16 and familial disease,17 The third type may arise from neoplasia within the parathyroid glands. These glands’ hyperactivity is induced by the above and other diseases and generally persists even after the disease that induced them has been treated. Although hemodialysis has greatly improved the longevity of patients suffering from CRI, its side effect renal osteodystrophy (ROD) still remains a real risk, particularly in those patients whose adherence to the recommended diet is poor. ROD manifests itself as calcified deposits. Although Asaumi et al.19 indicated that these calcified deposits around the jaws can be adequately displayed by conventional radiography and that advanced imaging such as HCT and MRI add little, Chang et al. illustrated that extent and structure of ROD within the hard palate was best displayed by HCT.16 Calcification within the arteries is discussed further in Chapter 10.
Localized Poorly Defined Radiolucencies
Localized poorly defined radiolucencies suggest both lesions of local origin and of an aggressive nature. Such disease could be either infections or malignant neoplasms. The primary differentiation between them, in the majority of cases, is made upon the clinical findings.
The majority of malignant neoplasms, particularly squamous cell carcinomas (SCC), are poorly defined (Figure 9.8; see also Figure 1.31) and destroy rather than displace bony structures. On occasion, malignancies may present with well-defined margins (Figure 9.9). In such cases other features such as widening of the periodontal ligament space and “floating teeth” and the “spiking” pattern of root resorption (Figure 9.10) may direct the clinician toward consideration of a malignancy.
Figure 9.8. Conventional radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) of a carcinoma arising from odontogenic lesion. (a) The panoramic radiograph displays an unerupted third molar with the apex of its completely formed root displaced through the lower border of the mandible. Although a normal follicle space is apparent on the mesial and distal aspects of the crown of this tooth, the occlusal part has been irregularly expanded and largely delineated by a band of sclerosis. Outside this band there is a large area of radiolucency that has a poorly defined periphery. (b) The posterioanterior projection of the mandible does not delineate the buccal cortex, which must now be presumed to have been perforated. The axial (c) and coronal (d) bone-window computed tomography confirm the substantial loss of the buccal cortex. The neoplasm has now substantially expanded into the adjacent soft tissue. (e) Fragments of bone are observed at the anterior periphery of the lesion. The precontrast axial soft-tissue window (c) shows that the neoplasm is subjacent to the subcutaneous tissue of the facial skin. (f) The axial contrast section reveals enhancement at the periphery but also as chords extending toward the neoplasm’s center indicating an extensive intralesional vasculature. The nonenhanced areas are likely to represent necrosis. (g) The coronal section contrast soft-tissue window displays substantial peripheral enhancement, but the center is substantially necrotic.
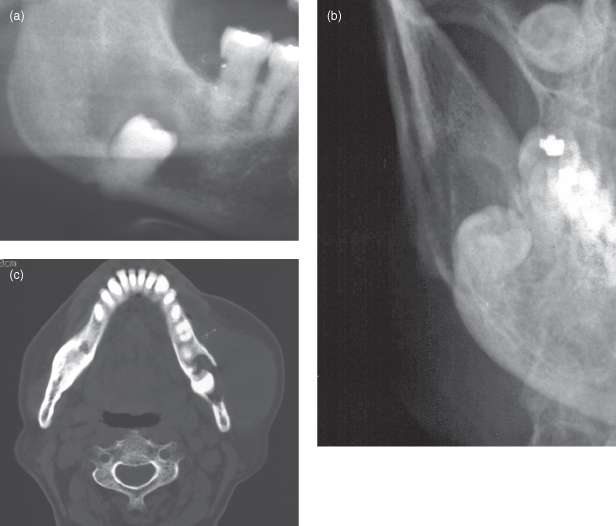
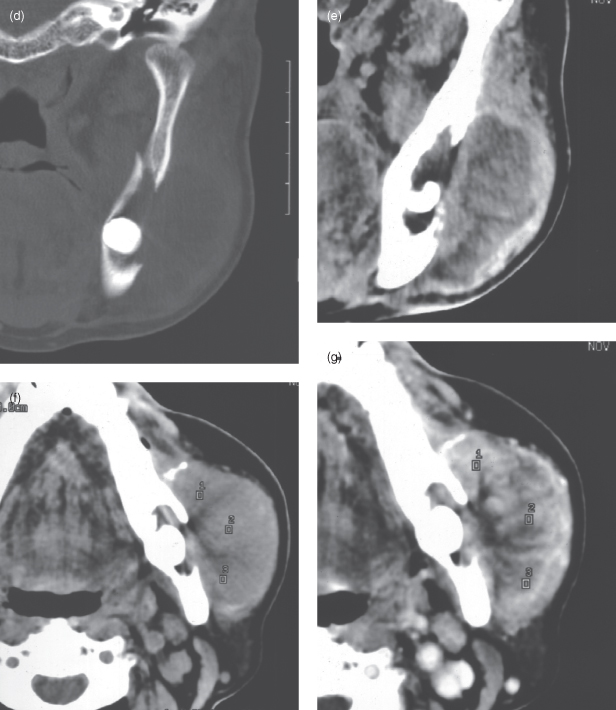
Figure 9.9. Panoramic radiograph of a well-differentiated carcinoma. Although its margin is largely well defined, the widening of the periodontal ligament space on the mesial root of the first molar and the “floating” premolars directs the clinician to consider a malignancy; there is also some resorption of the apices of the premolars. Note: This case should be assessed for paresthesia of the lip. The lesion is sited at the mental foramen.
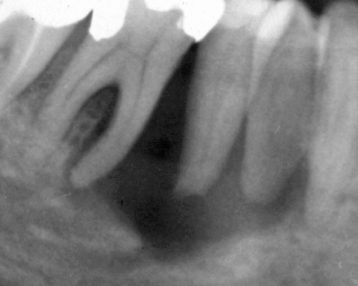
Figure 9.10. Conventional radiographs and computed tomography (CT) of a case of poorly differentiated mucoepidermoid carcinoma. (a) Periapical radiograph exhibiting irregular bone loss (radiolucency) around the left lateral incisor. It is “floating” and its root apex displays spiking pattern resorption. The canine’s root has also be resorbed but largely upon its mesial surface. There is some spiking pattern root resorption on the ipsilateral central incisor. A mesiodens is also included within the radiolucency. (b) Periapical radiolucency in addition shows periapical radiolucencies on the contralateral restored incisors. (c) Anterior occlusal displays involvement of the floor of the nose. (d) Axial CT (bone window) reveals radiolucency displacing the left lateral incisor buccally. It has a soft-tissue radiodensity at the periphery and a air-or-gas-filled center.
SCC is the most frequent malignancy of the oral cavity and oropharynx. The World Health Organization’s Oral Health Program reveals that its age-standardized rate (ASR) is equal to or exceeds 6.9 cases per 100,000 world standard population for males in North America, most of Europe (except Northern Europe), the Indian subcontinent, Australia, Brazil, and Southern and Eastern Africa.20 For females, the ASR is similar or greater than 6.9 cases per 100,000 in the Indian subcontinent, Ethiopia, some Southern African states, and New Guinea.20 Although it primarily presents as a lesion on the oral mucosa, which will be primarily addressed in Chapter 18, some arise within the odontogenic epithelial remnants or “rests,” within the jaw bones.
Although SCC far more frequently affects the mucosa rather than the bony jaws, this chapter will focus only on the latter, whereas the former is especially considered in the Chapter 18.
Primary Intraosseous Squamous Cell Carcinomas (ICD-O 9270/3)
Eversole et al. defined the primary intraosseous squamous cell carcinoma (PIOSCC) as “a central jaw carcinoma derived from odontogenic epithelial remnants. Subcategories of PIOSCC include (1) a solid tumor that invades marrow spaces and induces osseous resorption, (2) squamous cancer arising from the lining of an odontogenic cyst and (3) a squamous cell carcinoma in association with other benign epithelial odontogenic tumors. When the tumor destroys the cortex and merges with the surface mucosa, it may be difficult to distinguish between a PIOSCC and a true carcinoma arising from the oral mucosa. Invasion from an antral primary must also be excluded.”21
Eversole et al. also report that PIOSCCs are found twice more frequently in males.21 Although they generally first present with a mean age of 55 years, cases affecting infants have been reported. They are usually found in the posterior sextant of the mandible (Figures 9.8 and 9.11). If they affect the maxilla, they are most frequently observed in the anterior sextant. Although some produce swelling and/or mental paresthesia, the majority are symptom-free and found incidentally on radiographs. Radiographically, early lesions are often indistinguishable from odontogenic cysts (Figure 9.11). Cortical destruction and invasion of the adjacent soft tissue are features of late lesions (see Figure 9.8).21
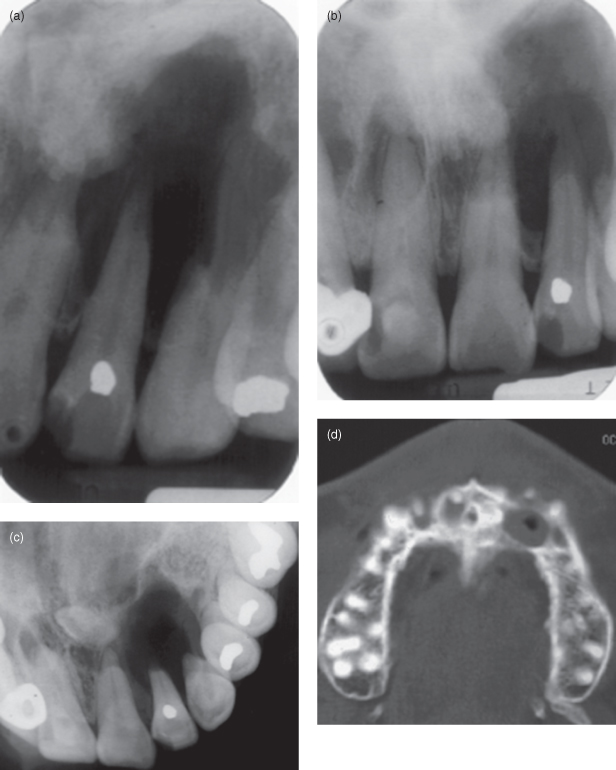
Figure 9.11. Panoramic radiograph and computed tomography (CT) of a primary intraosseous carcinoma. (a) Panoramic radiograph exhibits a well-defined corticated unilocular radiolucency occupying the anterior half of the vertical ramus from the coronoid process to the posterior body of the mandible. The last molar’s roots have been displaced mesially. (b) Axial CT (bone window), at the level of the occlusal plane, displaying buccolingual expansion. The content of the lesion is soft tissue at the periphery and air or gas at the center. (c) Coronal CT (bone window), at the level of the condyle, reveals the same features observed in (b).
A PIOSCC associated with an impacted mandibular third molar (see Figure 9.8) is associated with a more favorable prognosis. They are, nevertheless, infrequently reported.21
Huang et al.’s recent report on Chinese solid-type PIOSCCs reported them as high-grade malignancies which frequently metastasize to regional lymph nodes.22 They also have a high recurrence rate (76% at 5 years posttreatment) and thus a high mortality.22
Radiolucency of Inflammatory Origin
Radiolucencies of inflammatory origin arise from a dental infection. This most frequently arises from a necrotic pulp secondary to dental caries or trauma. The radiolucencies that result are most frequently sited at the apex of the affected tooth and are unilocular. When observed on a radiograph, these are best simply termed periapical radiolucencies. On occasion such a lesion may arise from a lateral canal; it is called a lateral radicular cyst, which is entirely different from a lateral periodontal cyst (see later). Periodontal disease can also produce in radiolucencies. These are associated with pockets arising within bone, including loss of bone at the furcation. Radiolucencies associated with inflammation can also arise secondarily in a preexisting lesion such as a cyst or neoplasm. These infected cysts or neoplasms can appear both clinically and radiologically difficult to distinguish from a malignant neoplasm. Infected keratocystic odontogenic tumors affecting the maxillary antrum can present clinically and radiologically as antral malignancies (Figure 11.20).23
Periapical Radiolucencies of Inflammatory Origin
The periapical radiolucency is classically juxtapositioned to the apex of a tooth, which has a large carious lesion or large restoration or is fractured and/or is unresponsive to vitality testing, suggesting pulpal necrosis. Nevertheless, such a finding should prompt pulp-vitality testing of affected tooth/teeth because any lesion can present first as a periapical radiolucency, such as osseous dysplasia (Figure 9.12), the already-mentioned PIOSSC,21,22 and SCC (see Figures 9.9 and 9.10). Other clinically significant lesions that have been reported recently to present as a periapical radiolucency have been the ameloblastomas (Figure 9.13)24,25 and the giant cell lesion.26
Figure 9.12. The periapical radiographs display periapical radiolucencies associated with noncarious and pristine lower incisors. These are most likely to represent early-stage osseous dysplastic lesions. A positive response to pulp vitality testing is sufficient to confirm their diagnosis.
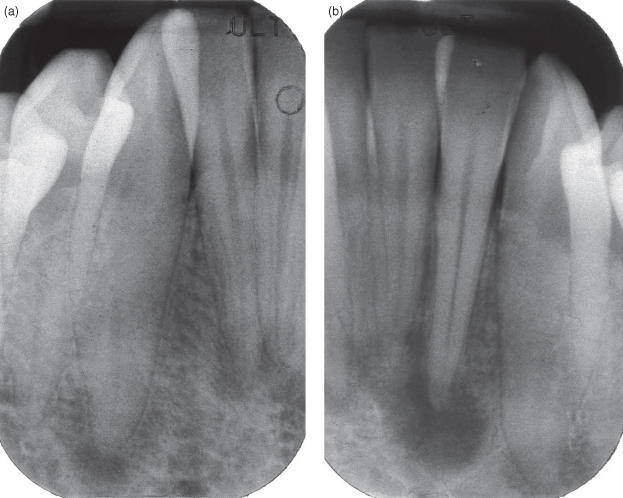
Figure 9.13. A periapical radiolucency of a multilocular ameloblastoma. It presents aa a radiolucency, which has a well-defined inferior margin, but a poorly defined superior margin subjacent to a grossly carious first molar with a large furcation radiolucency. The two clues that this lesion is not primarily of inflammatory origin are its multilocular appearance and the fact that its epicenter is not at or close to the origin of inflammation.
The term periapical radiolucency is the most appropriate to use when an inflammatory process is suspected because it encompasses the granuloma, the cyst, and the abscess, which differ histologically. Many attempts have been made to correlate the various radiological features of the periapical radiolucency (including its size) with its resultant histopathology. Almost all have substantially failed, other than to report that the periapical radiolucency is more likely to be a cyst if it is large and it has a well-defined margin.
The second edition of the WHO’s histological typing of odontogenic tumors describes the radicular cysts as “a cyst arising from the epithelial residues (rests of Malassez) on the periodontal ligament as a consequence of inflammation, usually following the death of the dental pulp.”27 Radicular cysts are the most common cyst found in the jaws. Although they may occur in relation to any nonvital tooth, they are infrequently associated with deciduous teeth. They are most frequently associated with teeth of the maxillary anterior sextant. Their peak age at first presentation is the third and fourth decades. Males are more frequently affected.27
Gundappa et al. compared the images of periapical lesions of ultrasound (US) with analogue (film) and digital (charge-couple device) dental radiography.28 The two dental radiographic technologies did not allow differentiation between cysts and granulomas, whereas US did in each of the 15 cases. They concluded that while dental radiography determines the existence of the periapical disease and its extent, US can determine whether the lesion is or is not cystic if sufficient buccal cortex has been resorbed. The underestimate of the lesion’s size by US was attributed to the acoustic shadow cast by the bony edges of the lesion on its lateral walls.28
Paradental Cyst
The paradental cyst also called the buccal bifurcation cyst (BBC) was defined by the second edition of the WHO histological typing of odontological tumors as “a cyst occurring near to the cervical margin of the lateral aspect of a root as a consequence of an inflammatory process in a periodontal pocket” … “the histological features are … the same as those of the radicular cyst.”29 It arises from the odontogenic epithelium of the periodontal ligament of a vital tooth. Its distinctive feature is its association with the buccal or distal aspects of an erupted mandibular molar tooth. This tooth is most frequently the third molar (Figure 9.14). Similar cysts can arise from the buccal aspect of the first molar tooth in 6- to 8-year-old children.29
Figure 9.14. Panoramic radiograph of buccal bifurcation cyst. A well-defined partially corticated radiolucency is superimposed upon the root of an unerupted third molar. If has displaced the mandibular canal downward in addition to reducing its diameter.

Pompura et al. reported the largest case series of 44 cases in 31 patients presenting in a children’s hospital over 3 years.30 They all presented with tenderness and discomfort about the time of eruption of the first molar. The eruption of the lingual cusps occurs first, Some buccal swelling may be present. The true occlusal radiograph best displays most of the radiological characteristics of the BBC and is recommended projection to complete the investigation of the BBC. Figure 3 in Pompura et al. is a panoramic radiograph that displays a BBC that looks identical to a dentigerous cyst.30
The rarity of reports other that the preceding indicates the infrequency of this lesion. Iatrou et al. found it in only 9% of all intraosseous lesions of the jaws of children.31
Lateral Periodontal Cyst
The lateral periodontal cyst was defined by the second edition of the WHO’s classification of odontogenic neoplasms, as “a cyst occurring on the lateral aspect or between the roots of vital teeth and arising from odontogenic epithelial remnants, but not as a result of inflammatory stimuli.”32 According to Shear and Speight, the term lateral periodontal cyst should be “confined to those cysts that occur in the lateral periodontal position (the side of the tooth between the apex and cervical margin of the root) and in which inflammatory etiology and diagnosis of collateral OKC (now the keratocystic odontogenic tumor—my parentheses) have been eradicated on clinical and histopathological grounds.”33 In other words a biopsy is required for a definitive diagnosis. The reason for this necessarily rather long and vague definition is that most recent reports on this lesion have been case reports and have not led to a consensus on the pathogenesis of the lesion. Nevertheless, a feasible pathogenesis, suggested by Shear and Speight, is the lateral periodontal cyst’s histopathology of a reduced enamel epithelium lining, representing a lateral(-positioned) dentigerous cyst, which was displaced apically as the tooth erupted. The most classical image is Shear and Speight’s Figure 6.9.33 Two other potential origins they discuss are the clear cell rests of the dental lamina and cells of Malassez.33
The lateral periodontal cyst accounts for 24 cases referred to Shear’s South African pathology service, at a mean annual rate of 0.7 cyst per year.33 Their average age of 6 reports34–39 is 47 (37–55) years. Almost all lateral periodontal cysts first present in the fifth to seventh decades, peaking in the sixth. Overall there appears to be equality between the sexes. Rasmussen reports that females present younger than the males.37 Although the sites vary between the reports, there is a general predilection for anterior sextants.
The clinical presentation ranges from symptomless and discovery incidental to a radiological investigation for another clinical indication, to pain and swelling, which may be fluctuant.33
According to Altini and Shear,34 on radiographs the lateral periodontal cysts present as round or ovoid well-defined radiolucencies with a “sclerotic margin.” They are generally smaller than 1 cm. These features differ from those of “botryoid cysts,” which are larger, multilocular and extend apical to the periapical area. They do not display root resorption.34
All lateral periodontal cysts occur anterior to the molars; Formoso Senanda et al. report 3 mandibular lateral periodontal cysts were sited in the premolar region.39 Figure 1.26 displays an image that is classical for a lateral periodontal cyst, except that this is of a keratocystic odontogenic tumor (KCOT), reinforcing the need to include the latter in the differential diagnosis.
The mandibular premolars are the most frequent site, followed by the maxillary anterior sextant. Furthermore, Formoso Senande et al. noted that all their 8 maxillary lateral periodontal cysts were found between the lateral incisor and the canine.39 This presentation recalls the globulomaxillary cyst, which, while it is no longer considered to be a true lesion, represents in most cases either a lateral periodontal cyst or a KCOT.
Although the treatment is simple enucleation without sacrifice of the associated tooth, if possible, Shear and Speight advise that those cases that prove on histopathological examination to be of the encapsulated multicystic variety, should be followed up for a number of years because its behavior is not yet completely certain.33
Botryoid Odontogenic Cyst
This is microscopically similar to the lateral periodontal cyst, but additionally it is multicystic with thin fibrous connective tissue septa.40 The name botryoid is derived from its bunch-of-grapes–like presentation reflecting its purported multilocular radiological presentation.41
Méndez et al. synthesized the literature.41 Their synthesis revealed that 85% affected the mandible, mainly the premolar-canine region, whereas the maxillary cysts affected the anterior sextant.41 These sites are identical to those of the lateral periodontal cyst. Two-thirds presented with symptoms; therefore a third would have been detected incidentally. The median age at first presentation was 54 years,41 older than that for lateral periodontal cysts.
Like the lateral periodontal cyst its margins are well defined.
Although multilocular lesions, hitherto considered an essential characteristic of the botryoid cyst, accounted for only 40% of all botryoid cysts, they were significantly more frequently observed among the 12 cases that recurred. Eleven cases that recurred were multilocular, whereas only 5 of the 21 cases that did not recur were multilocular.
The slight predilection for females was not reflected among the recurrences where there was no gender bias. It was noted that those subjects who had recurrence had a median age of 48 in contrast to a median age of 55 years for those who did not. A third recurred after a median of 8 years.41
Perhaps potential markers for a lesion that is more likely to recur are multilocular radiolucencies of 31 mm in contrast to 10 mm first presenting in early middle age (circa 40 years old).41
In summary, although this cyst has the broad clinical and radiological appearance of a lateral periodontal cyst and may be considered to be a botryoid variant of the lateral periodontal cyst, it is generally multilocular, presents with symptoms, and tends to recur.41
Hemangioma
Waner and Suen substantially reclassified congenital vascular lesions of the head and neck into hemangiomas and vascular malformations. The former are “usually not present at birth, proliferate during the first year and then involute,” whereas the latter are “always present at birth, never proliferate and never involute.”42
Zlotogorski et al.’s synthesis of 86 cases of hemangiomas affecting the jaws revealed predilections for females (56%), the mandible (77%), and the posterior sextants of both jaws (64% for the mandible and 82% for the maxilla). The mean age was 23.3 (0–74) years.43
Of the 32% of hemangiomas displaying well-defined borders, none were sited in the maxilla (Figure 9.15). Ninety-six percent of the lesions were radiolucent. Thirty-seven percent of the mandibular lesions and 25% of the maxillary lesions were unilocular. Of the 38 multilocular lesions affecting the mandible, 47%, 34%, and 8% were honeycomb, soap-bubble, and spokelike, respectively. Of the 12 multilocular lesions affecting the maxilla, 42%, 42%, and 8% were honeycomb, soap-bubble, and spokelike, respectively. Root resorption was reported for 20 cases, 17 in the mandible. Tooth displacement was reported in 14 cases, 11 in the mandible. Of the 41 cases that affected the posterior sextant of the mandible, 10 exhibited involvement of the mandibular canal. This usually presented as an enlargement of the canal’s width.43
Figure 9.15. Anterioposterior projection of the mandible displaying a hemangioma affecting the buccal half of the posterior body of the mandible. It is well defined with minimal buccolingual displacement. The only hint as to its presence on the accompanying panoramic radiograph was that the trabeculae, but not the teeth, appeared out of focus.

Further clinical and radiological features that may indicate the presence of a hemangioma are port-wine stain on the skin, which may blanch under pressure from a glass microscopic slide. Ascultation may reveal bruits. Teeth may appear larger and have erupted earlier on the affected side. Thromboliths (Figure 9.16) may be observed in hemangiomas that affect soft tissue. The hemangioma enhances on HCT (Figure 4.12) and on MRI (Figure 6.15).
Figure 9.16. Panoramic radiograph displaying thromboliths within a hemangioma. The radiopacities are well defined. The larger one in the center exhibits the alternating concentric radiopaque and radiolucent rings typical of the target pattern, which is almost pathognomic of the thrombolith.

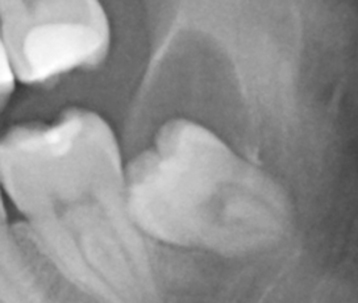
Pericoronal Radiolucencies
Pericoronal radiolucencies, particularly of mandibular third molars, occur frequently. They are particularly important because they not only suggest cystic change within the follicle of the unerupted tooth but may represent perhaps a neoplastic change within that follicle or a secondary envelopment of it by a neoplasm. This neoplastic change is most frequently benign, but it can be malignant (see Figure 9.8). The mandibular third molar site is also the most frequent site for occurrence of many odontogenic neoplasms; some recur if misdiagnosed and inappropriately treated.
Radiolucencies associated with the crown of a unerupted tooth are usually suggestive of dentigerous cysts, but not always. The review by Curran et al. of the over 2,600 pericoronal surgical specimens that had been referred to their pathological service over 6 years revealed that only 67% were not pathological, they were simply normal dental follicles.44 Twenty-eight percent were dentigerous cysts of which 35 included mucous cells. Of the remaining 5%, 71 were “keratocysts” (see KCOT later), 13 each were ameloblastomas and carcinomas, 6 were calcifying cystic odontogenic tumors, 4 were calcifying epithelial odontogenic tumors, and one was an odontogenic myxoma. The reader should note that the authors considered that only a fraction of all specimens arising from unerupted teeth within their community had actually been referred to them. Furthermore, the specimens sent were considered by the referring surgeon to be potentially pathological. Not only did most come from older patients but also, on subsequent histopathology, those were found most likely to be pathological.
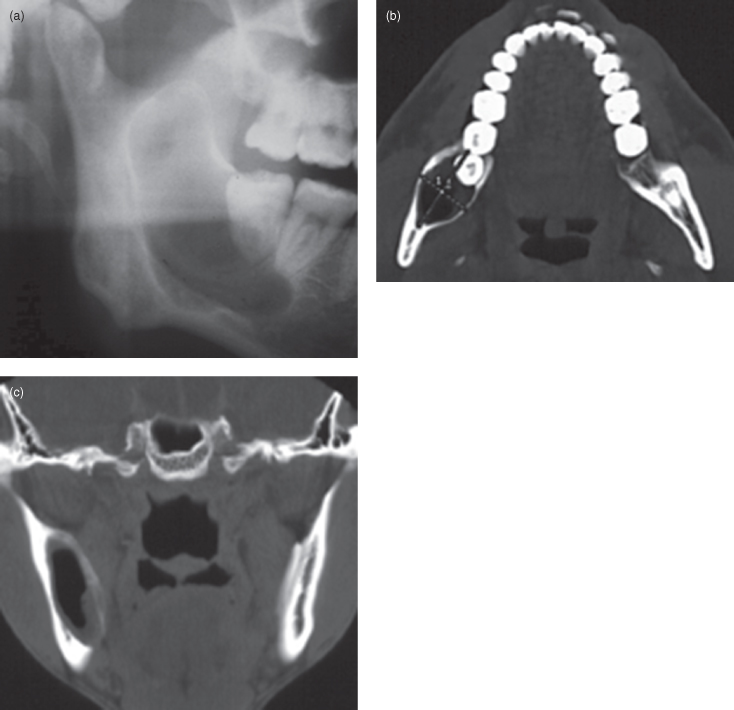
An important feature, which distinguishes dentigerous cysts and follicle spaces from more serious lesions, is the relationship of the cyst to the cementoenamel junction (CEJ) (Figure 9.17). Ikeshima et al. noted that the dentigerous cyst attachment was closer to the CEJ than that of the ameloblastoma.45 Other important features that tend toward the likelihood of a dentigerous cyst are unilocular radiolucency and an absence of root resorption.
Figure 9.17. This is a panoramic radiograph displaying a classical “central” pattern dentigerous cyst (DC) on the left. The coronal radiolucency is attached at the cementoenamel junction at the mesial and distal aspects. The symmetrical enclosure of the crown within the radiolucency is typical of the “central” pattern of radiological presentation of a DC. Note 1: The DC has essentially two parts: the cystic cavity itself and the tooth it is attached to. Therefore the DC can affect adjacent structures directly (due to direct contact between the cyst and them) or indirectly (by the tooth it is attached to and them). This DC is affecting the mandibular canal both directly (reducing the mandibular canal’s diameter mesially to the unerupted third molar) and indirectly (reduction in the mandibular canal’s diameter and its downward displacement by the tooth).

Dentigerous Cyst
The dentigerous cyst, as defined by the second edition of the WHO, is a “cyst which encloses the crown and is attached to the neck of an unerupted tooth. It develops by accumulation of fluid between the reduced enamel epithelium and the crown, or between the layers of the reduced enamel epithelium.”46
The relationship of the radiographic periphery of the radiolucency surrounding the crown to the “neck” or CEJ is crucially important to a diagnosis of a dentigerous cyst radiologically. Based upon a study by Ikeshima et al.,45 I conclude that an attachment that is less that 1 mm apical to the CEJ is strongly suggestive that the lesion could be a dentigerous cyst.
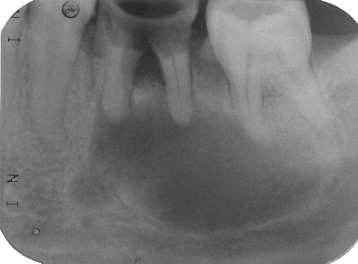
The global distribution of reports included in the systematic review47 upon which much of the following is derived is set out in Figure 1.41 and their details in Table 9.1.
Table 9.1. Dentigerous cyst: systematic review
*Advises that the percentages were derived from either one report or from a synthesis of no more that 50 cases. Ant : Post, Anterior : Posterior; INA, Information not available; LatinAmer, Latin American; Mand : Max, Mandible : Maxilla; subSaharan, sub-Saharan African; ToothDispl, Tooth displacement; ToothResorp, Tooth resorption; Western, predominantly Caucasian. Y : N, Yes : No.
The prevalence of the dentigerous cyst could be high at least in one Turkish community. Yildirim et al. reported that pathological changes among symptom-free third molars was 23%, of which two-thirds were dentigerous cysts, the rest were calcifying cystic odontogenic tumors and “odontogenic keratocysts.”48
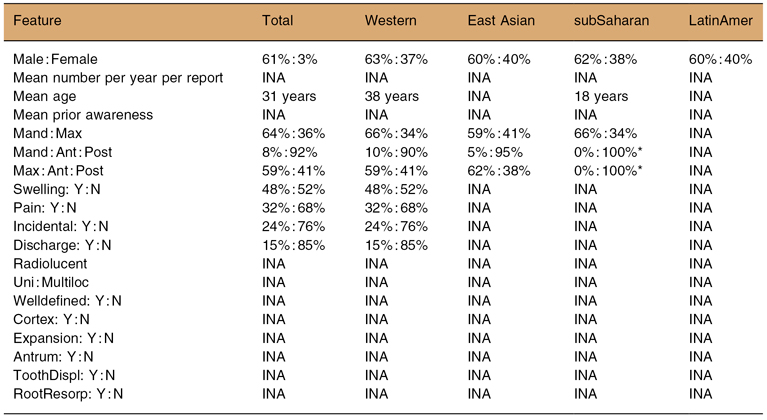
The dentigerous cyst is most commonly associated with a mandibular third molar (48%) (see Figure 9.17), a maxillary canine (17%) (Figure 9.19), a mandibular premolar (10%) and a maxillary third molar (4%).49 It is also associated with supernumeraries; 90% of such cysts are associated with mesiodens (Figures 9.18, 11.26). Kaugars et al. reported that 28% of odontomas had dentigerous cysts.50
Figure 9.18. This standard anterior occlusal radiograph displays a well-defined radiolucency associated with the crown of an inverted mesiodens as it arises from the cementoenamel junction. This is a “central” pattern dentigerous cyst (DC). This DC is also associated with root resorption.
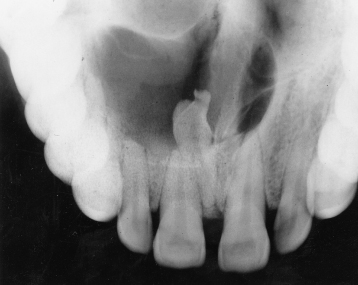
Figure 9.19. This cone-beam computed tomograph (CBCT) of a “lateral” pattern dentigerous cyst (DC) affecting a maxillary canine. The tangential sections display not only buccolingual expansion but also perforation of the labial (buccal) and palatal cortical plates. Note: The radiopacity within the left maxillary antrum is most likely to be an antrolith or an exotosis.
Dentigerous cysts affect males in 61% of cases of all ethnic groups (Table 9.1). Shear and Speight report it more frequently in South African Whites than in South African Blacks.49 The mandible is affected in nearly two-thirds of cases (64%). Ninety-two percent are found in the posterior sextant of the mandible. This feature was significantly more likely in the East Asian global group than in the Western. In the maxilla, it is found in the anterior sextant in 59% of cases. It is found as an incidental finding in 24% of cases and with a swelling or pain in 49% and 32%, respectively.49
Although the dentigerous cyst is a reasonably common lesion (18% of jaw cysts in a recent report)51 and has been reasonably frequently reported (see Figure 1.41) its radiology as revealed in a recent systematic review has not yet been subject to a single detailed reported series of consecutive (nonselected) cases affecting a community.47 The only systematic review-included reports that feature such details are Ioannidou et al.,52 who reported all dentigerous cysts as well defined, and Ledesma-Montes et al.,53 who reported them as radiolucent. Clearly these observations do not take us beyond what we already know. Nevertheless, it is generally recognized, in addition to their intimate relationship to CEJ, that all dentigerous cysts present on radiographs as unilocular radiolucencies. A multilocular appearance should direct the clinician straightaway to consider other lesions; these lesions (see Figure 9.4) are locally invasive and are more challenging to treat because they have a tendency to recur. The dentigerous cyst is simply enucleated with the attached tooth, with no recurrence.
The dentigerous cyst presents as one of three radiologic patterns.49 In the central or “classical” pattern the cyst is attached to both the mesial and distal CEJ and symmetrically envelops the crown of the unerupted tooth (see Figure 9.17). As it expands it can displace the tooth in an apical direction toward the lower border of the mandible or as far as the floor of the orbit in the maxilla. The second pattern, the “lateral” pattern arises from the side of the crown (Figures 9.19 and 9.20). This pattern is frequently associated with teeth, which are mesially or vertically impacted. The third pattern, the “circumferential,” is an exaggerated version of the central pattern; the cyst cavity expands down past the level of the CEJ. Its attachment to the root is still at the CEJ. The cyst is separated from the rest of the root by a bony sleeve containing the lamina dura. Frequently this pattern is seen when the tooth cannot be further displaced apically (see Figure 11.26). This pattern of dentigerous cyst needs to be distinguished from the KCOT or ameloblastoma. The last two generally do not appear to be attached at the CEJ.
Figure 9.20. The panoramic radiograph displays a dentigerous cyst (DC) associated with the left unerupted third molar tooth. This DC is obviously attached to the distal cementoenamel junction and covers the occlusal surface. The mesial surface of the tooth is in contact with the distal root of the adjacent second molar tooth. This pattern of radiological appearance is “lateral.” The root formation is complete. The apices have reduced the diameter of the mandibular canal.
Trying to distinguish between a dentigerous cyst and a follicle space can be difficult, particularly when the suspected dentigerous cyst is small, about 3 to 4 mm wide. Daley and Wysocki, following their study of this problem, concluded that certainty can be achieved only at the time of surgery.54
Struthers and Shear reported that a high percentage of dentigerous cysts in their report were associated with root resorption.55 This phenomenon does not appear to have been reported elsewhere in the literature. Root resorption of multiple adjacent teeth was observed in an exceptionally large dentigerous cyst (see Figure 11.27).
The dentigerous cyst is unlike most other odontogenic lesions. The dentigerous cyst has both a direct and indirect effect on adjacent structures by virtue that the associated unerupted tooth is an integral part of it. In addition to its direct effect on adjacent teeth, cortices, and mandibular canal, it can exert the same indirectly by its displacement of the attached tooth. Thus, in addition to a complete evaluation of the cyst itself, attention should be paid to the associated tooth and its effects on related structures to ensure minimal injury to them upon its extraction along with the enucleated cyst.
The treatment of choice for the dentigerous cyst is enucleation. Although it does not recur, 15 out of 19 unicystic ameloblastomas were clinically diagnosed as dentigerous cysts.56 Therefore, the surgical specimen derived from enucleation of such a dentigerous cyst should be submitted for histopathology. Wang et al. also reported that three partial surgical specimens, one derived from a marsupialization and two biopsies, displayed no histopathology suggestive of the ameloblastoma that was subsequently definitively diagnosed after histopathological examination of the entire surgical specimen.56
Shear and Speight address a common misapprehension that dentigerous cysts can readily undergo transformation to ameloblastomas which was the definitive diagnosis once the whole lesion had been removed and histopathologically reviewed.49 Their argument challenging this view is that dentigerous cysts in Shear and Singh’s South African study were far more common in Caucasian patients than in Black patients, in which they were uncommon, whereas the ameloblastoma was far more common in the latter, but infrequent in the former.57
Ameloblastoma (ICD-O 9310/0)
The WHO 2005 edition defined the ameloblastoma as “a slowly growing, locally invasive epithelial odontogenic tumor of the jaws with a high rate of recurrence if not removed adequately, but with virtually no tendency to metastasize.”58 Although this definition was specifically applied to the intraosseous-sited solid or multilocular ameloblastoma (see Figures 1.18 and 1.30, 11.21), it equally applies to the other three variants. These variants are unicystic (see Figures 1.6, 1.16, 1.34–1.37), desmoplastic, and peripheral ameloblastomas. “The unicystic variant is an ameloblastoma which presents as a cyst. The peripheral variant is an extraosseous counterpart of the intraosseous solid/multilocular ameloblastoma. The last is the desmoplastic ameloblastoma, which exhibits pronounced desmoplasia.”58
In a case series, 20% of the solid variant was radiologically unilocular.59,60 As a result, “solid” rather than “multilocular” will be solely used to refer to this variant.
The global distribution of reports included in the systematic review59,60 upon which much of the following is derived is set out in Figure 1.38 and their details in Table 9.2.
Table 9.2. Ameloblastoma: systematic review
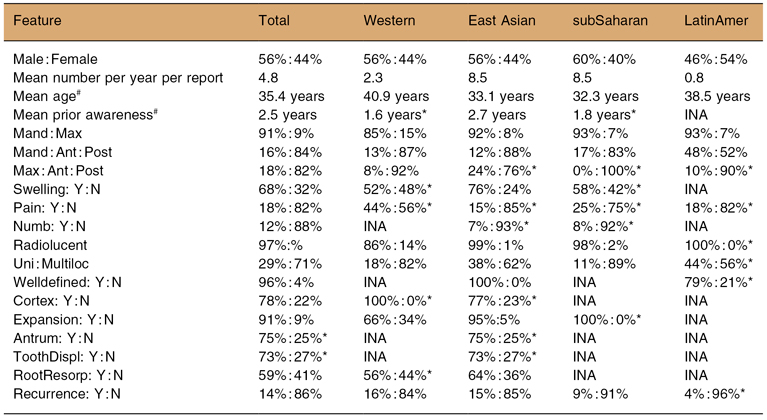
#Advises that this is not the cumulative mean calculated for the published report.
*Advises that the percentages were derived from either one report or from a synthesis of no more that 50 cases. Ant : Post, Anterior : Posterior; INA, Information not available; LatinAmer, Latin American; Mand : Max, Mandible : Maxilla; subSaharan, sub-Saharan African; ToothDispl, Tooth displacement; ToothResorp, Tooth resorption; Uni : Multiloc, Unilocular : Multilocular; Western, predominantly Caucasian; Y : N, Yes : No.
The proportion of the variants varies with the community reported. Some East Asian communities report more unicystic variants,59,60 whereas the desmoplastic variant may be more frequent in North American and European communities.61
The mean number of ameloblastomas per year is globally 4.8. It is significantly greater for both the East Asian and sub-Saharan African global groups, 8.5 ameloblastomas per year for each, than it is for either the Western (2.3) and Latin American (0.8) global groups.
This significantly higher “incidence” is also accompanied by a significantly younger age on first presentation for the East Asian and sub-Saharan African global groups, both about 33 years old. These differences may in part reflect the proportions of the solid, desmoplastic, and unicystic variants. The desmoplastic variant generally has an older mean age. After a synthesis of the literature, Philipsen et al. reported the mean age of the desmoplastic variant was 42 years in contrast to the solid variants’ 36 years,61 whereas, the mean age of the unicystic variant first presents at a significantly younger age.59,60
There were significant differences in mean age between the unicystic and solid variants in an East Asian report (Hong Kong Chinese).59,60 The mean age of the former was 24.6 years of age, whereas the mean age of the latter was 39.0 years of age. The Mainland Chinese report of Luo et al. mirrored the Hong Kong Chinese results closely, except that the proportion of unicystic cases was 31% rather than the latter’s 59%.62 Arotiba et -al.’s subjects were all under 20 years of age. Only 15% were unicystic, whereas the rest were of the solid variant.63 This clashed with the two Chinese reports, which found the unicystic cases to be significantly younger than the solid variant cases. In Arotiba et al.’s younger case series, if the Chinese results were applied, a markedly larger proportion would have been expected to be unicystic.
The age at first presentation was earliest for Bangladeshis and the Koreans and oldest for the Chinese, among which the earliest, a mean of only 30 years old, was for the Hong Kong Chinese.59 This early age of first presentation may have been affected by the very short period of prior awareness of the lesion before presentation in this community. This 0.7 years compared to 4 years overall for the systematic review. This period was even shorter for the younger patients in this Chinese community.59
Although overall ameloblastomas are almost equally distributed between sexes, Western, East Asian, and sub-Saharan African repo/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


