Orthognathic Surgery
• Mandibular Orthognathic Surgery
• Maxillary Orthognathic Surgery
• Maxillomandibular Surgery for Apertognathia
• Distraction Osteogenesis: Mandibular Advancement in Conjunction with Traditional Orthognathic Surgery
• Inferior Alveolar Nerve Injury
• Computer-Assisted Surgical Simulation: Virtual Surgical Planning for Orthognathic Surgery
Mandibular Orthognathic Surgery
Examination
The maxillofacial examination of the current patient proceeded as follows.
• There is no facial asymmetry.
• Maxillary dental midline is coincident with the facial midline.
• Mandibular dental midline is coincident with the maxillary dental midline.
• Chin point is coincident with the maxillary and mandibular midlines.
• Maxillary occlusal plane is canted down 1 mm on the right.
• Mandibular angles are level.
• Maxillary and mandibular arch widths are well coordinated (evaluated by handheld models or by having the patient posture the mandible forward into a Class I relationship).
Imaging
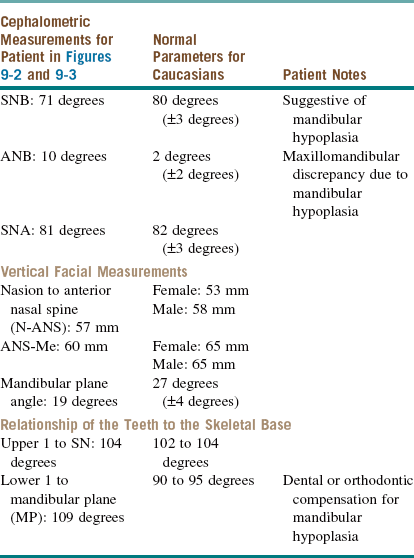
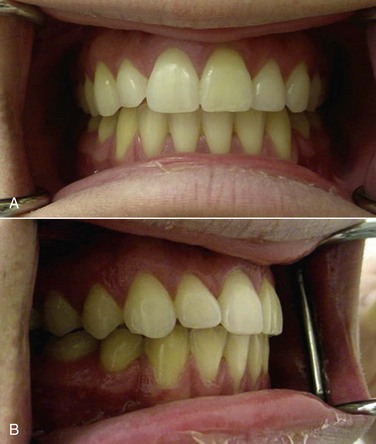
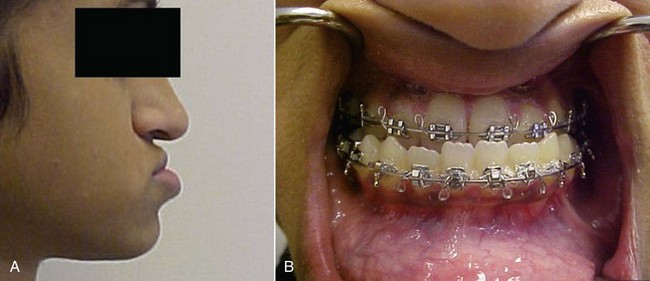
For the current patient, the preorthodontic cephalometric measurements and films are shown in Table 9-1 and Figure 9-2.
Treatment
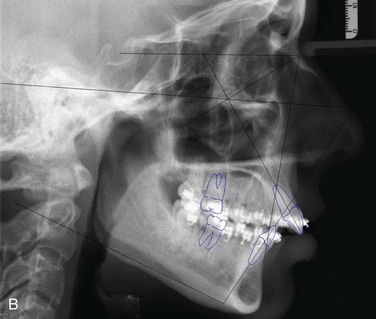
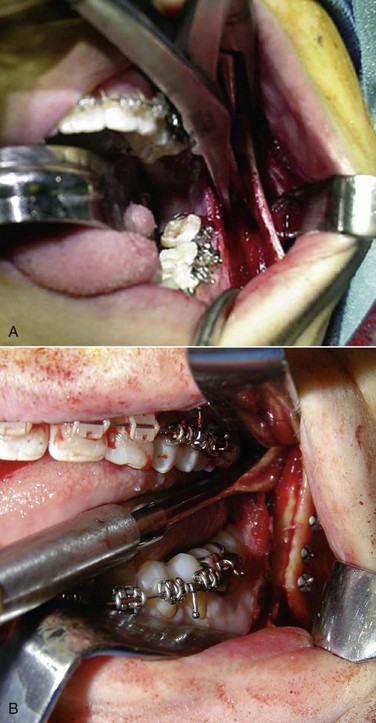
The current patient underwent a bilateral sagittal split osteotomy (Figure 9-3, A), resulting in a 10-mm advancement. The proximal and distal segments were fixated using three bicortical position screws at the superior border (Figure 9-3, B) on each side. Figure 9-4 shows the occlusion 9 months after the completion of surgery and 1 month after removal of the orthodontic appliances. Figure 9-5 shows the postoperative lateral cephalogram.
Baqain, ZH, Hyde, N, Patrikidou, A, et al. Antibiotic prophylaxis for orthognathic surgery: a prospective, randomised clinical trial. Br J Oral Maxillofac Surg. 2004; 42(6):506–510.
Bays, RA. Complications of orthognathic surgery. In: Kaban LB, Perrot DH, Pogrel MA, eds. Complications of oral and maxillofacial surgery. Philadelphia: Saunders, 1997.
Dalpont, G. Retromolar osteotomy for the correction of prognathism. J Oral Surg Anesth Hosp Dent Serv. 1961; 19:42.
Frey, DR, Hatch, JP, Van Sickels, JE, et al. Effects of surgical mandibular advancement and rotation on signs and symptoms of temporomandibular disorder: a 2-year follow-up study. Am J Orthod Dentofacial Orthop. 2008; 133:490.
Gerressen, M, Stockbrink, G, Riediger, D, et al. Skeletal stability following BSSO with and without condylar positioning device. J Oral Maxillofac Surg. 2007; 65:1297.
Hullihen, SP. Case of elongation of the under jaw and distortion of the face and neck, caused by a burn, successfully treated. Am J Dent Sci. 1849; 9:157.
Hunsuk, EE. Modified intraoral sagittal splitting technique for correction of mandibular prognathism. J Oral Surg. 1968; 26:250.
Lee, J. Bilateral sagittal split osteotomy for surgical management of mandibular deficiency. In: Bagheri SC, Bell RB, Khan HA, eds. Current therapy in oral and maxillofacial surgery. St Louis: Saunders, 2011.
Obwegeser, H. The indications for surgical correction of mandibular deformity by the sagittal split technique. Br J Oral Surg. 1962; 1:157.
Praveen, K, Narayanan, V, Muthusekhar, MR, et al. Hypotensive anaesthesia and blood loss in orthognathic surgery: a clinical study. Br J Oral Maxillofac Surg. 2001; 39(2):138–140.
Shepherd, J. Hypotensive anaesthesia and blood loss in orthognathic surgery. Evid Based Dent. 2004; 5(1):16.
Zijderveld, SA, Smeele, LE, Kostense, PJ, et al. Preoperative antibiotic prophylaxis in orthognathic surgery: a randomized, double-blind, and placebo-controlled clinical study. J Oral Maxillofac Surg. 1999; 57(12):1403–1406.
Maxillary Orthognathic Surgery
Examination
The maxillofacial examination of the current patient proceeded as follows.
• The muscles of mastication and the TMJ capsule are nontender, with no evidence of clicking or crepitus (seen with disk perforation). The maximal interincisal opening is 45 mm, with good excursive movements and no deviation upon opening or closing (normal TMJ examination).
• There is no vertical orbital dystopia. The intercanthal distance is 31 mm (normal). The nose is straight and coincident with the midline. Malar eminences are within normal limits.
• Maxillary dental midline is 1 mm right of the facial midline.
• Mandibular dental midline is 1 mm left of the maxillary dental midline and coincident with the facial midline.
• Chin point is coincident with the facial midline.
• Maxillary occlusal plane is canted down 1 mm on the left at the canine.
• Mandibular occlusal plane and angles are level.
• Maxillary arch width is adequate (evaluated by handheld models).
• Nasolabial angle is 45 degrees (normal is 100 degrees ± 10 degrees).
• Labiomental fold is within normal limits.
• Lower facial third is deficient (normal nasion-ANS–to–ANS-menton ratio is 7 : 8).
• Maxillary incisor length is 10 mm.
• Upper incisor show is 0 mm at rest (ideally, there is 2 to 4 mm of tooth show at rest) and 6 mm in full smile (in an esthetically pleasing smile line, the gingival papilla or 1 mm of gingival margin is visible at full smile).
3. Dental component (occlusion and dentition)
• There is deep bite (Figure 9-6, B).
• Overjet is −6 mm (normal is +3.5 mm ± 2.5 mm).
• Class III relationship is present at the first molars and canines bilaterally.
• Arch width is adequate on handheld models (transverse maxillary deficiencies may require a segmental Le Fort I osteotomy or surgically assisted rapid palatal expansion).
• Curve of Spee has been appropriately leveled, and additional postoperative leveling will be required (1 to 1.5 mm of arch space is required for each 1 mm of curve of Spee leveled).
• Maxillary and mandibular arch forms are ideal.
• Dental compensations have been adequately decompensated without the need for bicuspid extractions (retracting proclined incisors requires 0.8 mm of arch space for each 1 degree retracted; proclining incisors 1.25 degrees gains 1 mm of arch space).
• Dentition is in good repair, with no missing teeth (except for third molars).
Imaging
An initial lateral cephalogram was obtained with the patient in centric relation and lips in a relaxed/reposed position (Figure 9-7). Cephalometric analysis reveals anteroposterior maxillary hypoplasia. This preorthodontic lateral cephalogram illustrates the degree of skeletal discrepancies, in addition to the degree of dental compensations (proclined maxillary incisors); these are important considerations when calculating the adequacy of the existing arch space and determining the need for extractions (decompensating or retroclining flared incisors requires 0.8 mm of arch space for each 1 degree of retraction). It is important to note that measurements differ between Caucasians, Asians, and African Americans (normal values for Caucasian are listed in Table 9-2).
Table 9-2
| Patient in Figures 9-6 to 9-8 | Normal Parameters for Caucasians | Patient Notes |
| Cranial base angle: Normal | Sella-nasion (SN)-basion angle: 129 degrees ± 4 degrees Sella-nasion (SN) to Frankfurt horizontal (FH) angle: 7 degrees ± 4 degrees |
|
| SNA: 79 degrees | 82 degrees ± 3 degrees | Patient’s value is suggestive of a maxillary anteroposterior deficiency relative to the cranial base. |
| SNB: 88 degrees | 80 degrees ± 3 degrees | Patient’s value is suggestive of an excessive anteroposterior position of the mandible relative to the cranial base. |
| Harvold difference*: Excessive | Females: 27 mm Males: 29 mm |
Patient’s value is suggestive of maxillary hypoplasia or mandibular hyperplasia. |
| Mandibular plane (MP): Flat | SN-MP: 32 degrees ± 10 degrees FH-MP: 22 degrees ± 6 degrees |
|
| Long axis of upper incisor to SN angle: 134 degrees | 104 degrees ± 4 degrees | Patient’s value indicates severely compensated maxillary incisors |
| Long axis of lower incisor to MP angle: 100 degrees | 90 degrees ± 5 degrees | |
| Upper lip to E-plane: −5 mm | −3 mm ± 2 mm | |
| Lower lip to E-plane: +3 mm | −2 mm | Patient’s value shows retrusive soft tissue chin and concave profile. |
SNA, Sella-nasion, A point; SNB, sella-nasion, B point.
*The Harvold difference is the distance from condylion to pogonion minus the distance from condylion to A point.
Assessment
Maxillary retrognathia secondary to hypoplasia, resulting in a Class III skeletal facial deformity.
Treatment
• Align and level the occlusion
• Coordinate the maxillary and mandibular arches (progress is monitored with handheld models)
• Eliminate dental compensations in preparation for surgical correction of the skeletal deformities
• Diverge the roots of adjacent teeth for planned segmental osteotomies (only the roots should be diverged; the crowns retain interproximal contact)
• The mandible is in good position (dental midline and chin midline coincident with the facial midline).
• There is no mandibular occlusal cant.
• The mandible is aligned with the face (symmetrical).
• The mandibular arc of rotation positions the maxilla into a good anteroposterior position while maintaining an appropriate chin projection.
The final results for the current patient are shown in Figure 9-8.
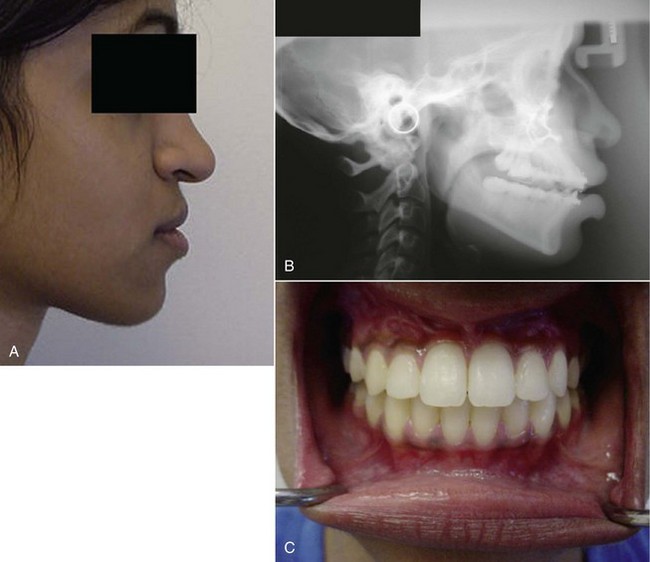
Figure 9-8 A, Postoperative profile showing correction of the midface hypoplasia and elongation of the short lower facial third. B, Postoperative lateral cephalogram showing correction of the maxillary hypoplasia and aesthetically pleasing facial profile. C, Postoperative intraoral view revealing the final occlusion.
Complications
An important aspect of orthognathic surgery is management of complications. A well-informed patient and attention to detail cannot be overemphasized. The most important complications of maxillary orthognathic surgery are (Box 9-1):
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses