Orthodontics I
Development, assessment and treatment planning
Chapter Contents
9.1 Craniofacial growth and occlusal development
9.2 Malocclusion: classification and aetiology
9.3 Patient assessment in orthodontics
Overview
Orthodontics relates to facial and occlusal development as well as to the supervision, interception and correction of occlusal and dentofacial anomalies. The practice of orthodontics, therefore, spans from birth into adulthood, with current practice aiming to establish optimal and stable occlusal relationships with dentofacial harmony. An appreciation of facial and occlusal development is fundamental to understanding the possible aetiology of some orthodontic problems as well as being critical for their assessment and the planning of any likely treatment.
This chapter commences with an account of the rudiments of facial and occlusal development. It then details the elements of comprehensive clinical and cephalometric orthodontic assessment. Finally, the principles of treatment planning are considered.
9.1 Craniofacial growth and occlusal development
An understanding of both craniofacial growth and occlusal development is essential to orthodontic practice as the former has a significant impact on the latter.
Craniofacial growth
Pattern of craniofacial growth
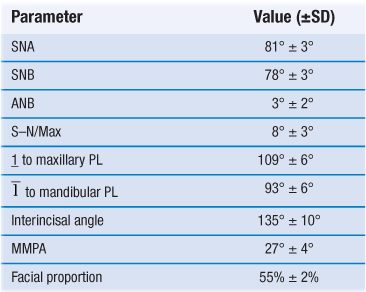
At birth, the face and jaws are underdeveloped compared with those in the adult. More growth, therefore, occurs of the facial skeleton than of the cranial structure postnatally. Growth patterns have been established for four major body tissue systems – lymphoid, neural, general or somatic, and genital – and it is important to have an appreciation of these as some patterns are followed by tissues involved in craniofacial growth (Fig. 9.1). Lymphoid growth is rapid up to about 10 years but undergoes involution as the genital growth is accelerating at puberty. Neural growth, however, is virtually complete by 6–7 years, while somatic growth increases in early childhood, then slows, before increasing dramatically at puberty.
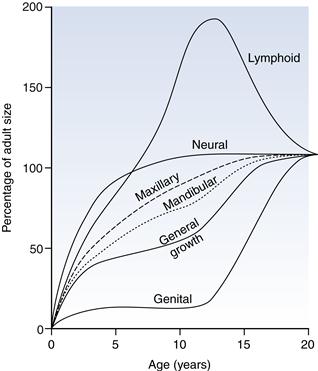
Fig. 9.1 Postnatal growth curves of various tissue types with superimposed maxillary and mandibular curves.
The pattern of neural growth affects skeletal growth of the calvarium and orbit, whereas the somatic growth pattern is followed approximately by the mandible and maxilla. More precisely, the jaw growth pattern falls between that followed by the neural and general body tissues, with the mandible aligning itself more to the latter than the maxilla. The spurt in jaw growth at puberty almost coincides with the spurt in height, on average at 12 years in girls and 2 years later in boys, although considerable individual variation exists.
For both the maxilla and mandible, on average, growth in width is completed in advance of that in length, which ceases before growth in the vertical dimension. The transverse dimensions of the jaws and dental arches do not tend to alter during puberty, as growth in width is largely completed before the growth spurt. Growth in length usually continues until 14–17 years in girls and 17–19 years in boys, while vertical growth may extend into the late teens in girls and into the twenties in boys. For males and females, growth of the maxilla in all dimensions is completed before that of the mandible.
Growth continues into adult life, with vertical changes in the facial skeleton predominating over anteroposterior changes, and least change taking place laterally. In the twenties, growth tends to resume slightly in females who overall exhibit a backward mandibular rotation. Although a late resumption of growth is not witnessed in males, a forward rotation of the mandible is usual in adulthood. Irrespective of the direction of mandibular growth rotation, compensatory adjustment occurs in the occlusal relationships. Facial growth should, therefore, be seen as a process that continues well into adult life and not as one that is complete in the late teens.
Control of facial growth
Both genetic and environmental factors impact on the regulation of craniofacial growth but the exact mechanisms are unclear. In theory, genetic control may be expressed primarily via bone, cartilage or the adjacent soft tissues (‘functional matrix theory’); the current concept is a merging of these second and third theories, bone largely having being discounted. Sutures and periosteal tissues do not determine craniofacial growth primarily, as sutural growth is reactive rather than inherently programmed. The maxillary sutures are not growth centres, but rather growth sites. The synchondroses of the cranial base and the nasal septum, to a lesser degree, probably act as independent growth centres but the cartilage of the mandibular condyle appears to react to, rather than initiate, growth.
Growth of the cranium and of the orbit in direct response to growth of the brain and of the eyes respectively lend support to the ‘functional matrix theory’. Growth of the cranial base, although mainly by endochondral growth coupled with bony replacement at the synchondroses, may be influenced by growth of the brain. Cartilaginous growth of the nasal septum and growth of the surrounding soft tissues probably contributes to moving the maxillary position forward but the amount apportioned to the former is unknown.
The soft tissues, including the masticatory muscles, are also contributors to spatial translation of the mandible and to addition of new bone at the condyle.
Growth prediction
At present, no method is available to predict accurately the amount, direction and timing of facial growth. Instead, the assumption is usually made that for most patients whose direction and amount of facial growth are about average, the likelihood is that their growth pattern will follow the same pattern through orthodontic treatment.
Methods attempting to predict the pattern of facial growth to assist orthodontic treatment planning include:
As the amount and direction of growth may not be ‘average’ in an individual, there is a considerable amount of imprecision with regard to ascertaining clinically useful growth prediction. The assumption is often made, however, that the direction of mandibular growth rotation is likely to continue.
Growth of the craniofacial skeleton
Craniofacial growth can be considered conveniently in relation to the calvarium, the cranial base, the maxillary complex and the mandible.
Calvarium
The precursors to the skull bones develop in membrane, and six open spaces (fontanelles) that exist at birth are eliminated by 18 months. Contact between the bones is at sutures. Bone apposition occurs at these periosteum-lined sites in response to brain growth and they fuse eventually in adulthood. The contour of the cranial vault also changes by periosteal remodelling at the inner and outer surfaces. The growth in size of the calvarium is complete by 7 years.
Cranial base
The cranial base forms initially in cartilage, which is transformed to bone by endochondral ossification. Sutural growth and surface remodelling occur laterally in response to brain growth. Of greater significance are primary cartilageous growth sites (synchondroses): sphenoethmoidal, intersphenoid and, most importantly, the spheno-occipital. The spheno-occipital synchondrosis grows until the early to mid-teens in females and somewhat later in males (15–17 years), having a profound impact on the anteroposterior skeletal pattern; it finally fuses at about 20 years. Because of its location in front of the temporomandibular joints but behind the anterior cranial base, both growth in length and in shape of the cranial base affects the maxillary–mandibular relationship. A long cranial base or large cranial base angle is associated with a class II skeletal pattern, while the converse is generally associated with a class III pattern (see Section 9.3 for definitions).
Maxillary complex
The frontal process and a mesenchymal condensation in the maxillary processes of the first pharyngeal arch form the maxilla which then ossifies intramembraneously, starting in the lateral aspects of the cartilagenous nasal capsule. Growth of the maxilla occurs via:
• bone apposition at the circum-maxillary suture system
• passive displacement from its articulation with the cranial base
Growth at the maxillary sutures assumes a greater role after age 7 years, when neural growth is complete and growth at the cranial base synchondroses lessens. As the maxilla moves downwards and forwards in response to growth of the surrounding soft tissues, the space opened at the superior and posterior sutures is obliterated by bone deposition on either side of the suture. Resorption of the anterior maxillary surface occurs simultaneously. Displacement of the maxilla inferiorly is accompanied by bone resorption from the nasal floor and deposition on the palate, while the alveolar process also develops vertically with tooth eruption. Bone is deposited also at the midline suture in response to lateral displacement of the maxillary halves, leading to an increase in midfacial width. The increase in maxillary dimensions lag behind those of the nasal structures, especially at puberty where a 25% differential is recorded. Maxillary growth is complete by about 17 years in males and on average 2 years earlier in females.
Mandible
Like the maxilla, the mandible is derived from the first pharyngeal arch. It begins development as a mesenchymal condensation just lateral to Meckel’s cartilage. Ossification proceeds intramembraneously, spreading posteriorly along Meckel’s cartilage without directly replacing it by newly formed bone. Condylar cartilages are formed distant to the mandibular body but fuse with it at about 4 months. These secondary cartilages are not primary instigators of mandibular growth but respond to other controlling influences. Endochondral ossification at the condyles accounts, in part, for mandibular growth. Elsewhere, bone apposition and remodelling are responsible for an increase in size and shape. As the mandible is translated downwards and forwards, largely in response to muscular forces, contact with the base of the skull is maintained by cartilagenous growth at the condylar heads, which increases ramal height. The alveolar processes also increase in height with tooth eruption.
Mandibular length is increased by periosteal apposition along the posterior border and simultaneous bone removal from the anterior aspect of the ramus. An increase in mandibular width occurs principally by remodelling posteriorly. The chin is almost passive as a growth area but, by the late teenage years, it has become more prominent particularly in males. On average, mandibular growth is complete by about 17 years in females and 2 years later in males, but it can proceed for longer.
Growth rotations
The trend is for the facial skeleton to grow downwards and forwards away from the cranial base, although implant studies have indicated that rotations of both the maxilla and mandible occur during growth. These have more marked effects on the mandible than on the maxilla, where remodelling disguises their true impact. Mandibular growth rotations represent a growth imbalance in anterior and posterior facial heights. The direction of condylar growth and the vertical magnitude of growth at the spheno-occipital synchondrosis influence posterior facial height. Growth of the masticatory and suprahyoid musculature, including associated fascia and influenced partly by the vertical growth changes in the spinal column, affects the anterior facial height together with the eruption of teeth.
While mandibular growth rotations occur in all individuals, these are particularly different where the vertical facial proportions are markedly reduced or increased. A forward rotation, characterised by greater growth in posterior than in anterior facial height, is more common than a posterior growth rotation, where the change in facial height ratio is opposite to that observed in forward rotation (Fig. 9.2). Where forward rotation of the mandible is extreme:
• the lower border is convex with a reduced mandibular plane angle
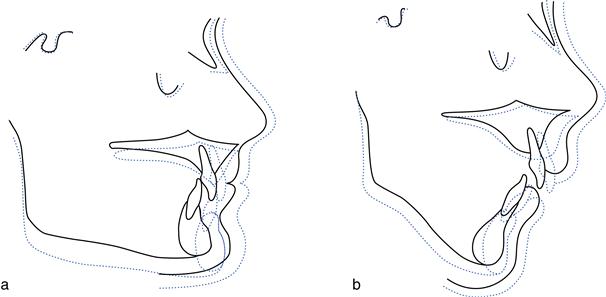
Fig. 9.2 Growth rotation.
(a) Forward growth rotation owing to greater increase in posterior than in anterior facial height, resulting in an increased overbite. (b) Backward growth rotation owing to a greater increase in anterior than in posterior facial height, resulting in a reduced overbite.
Conversely, a backward rotational pattern of mandibular growth results in:
• a pronounced antegonial notch with a high mandibular plane angle
The pattern of rotation has an impact on treatment. Whereas a forward rather than a backward rotation aids correction of a class II skeletal discrepancy, it also tends to increase overbite. Where the rotation is marked, overbite reduction is more difficult. Growth rotations also influence the inclination and anteroposterior position of the lower incisors. A forward growth rotation leads to retroclination of the lower incisors and an increase in lower labial segment crowding. With a posterior mandibular growth rotation, the incisors become upright, shortening the dental arch and producing crowding of the lower incisor area. Lower labial segment crowding is common in late teens particularly where mandibular growth continues after maxillary growth has ceased but other factors are likely contributors (see below).
Soft tissue growth
At birth, the orofacial musculature is well developed to allow suckling and breathing, and it soon responds to other functional demands of mastication, speech, facial expression and changes to the swallowing pattern. The light pressures from the lingual and buccolabial musculature affect tooth position, guiding the teeth towards a functional relationship and compensating, where possible, for any skeletal discrepancy. However, where a severe skeletal discrepancy or abnormal soft tissue behaviour exists (e.g. a lip trap with a class II division 1 malocclusion), the dento-alveolar compensatory mechanism will be insufficient.
Facial musculature lengthens with facial growth which increases the likelihood of lip competence. In girls, the greatest overall changes in soft tissues occur between 10–15 years but nasal growth is complete generally by age 16. In boys, however, the greatest soft tissue changes usually occur later (from 15 years) and most will be complete by late teens. In adulthood, soft tissue profile changes take place in both sexes in concert with, but are much larger than, those of the facial skeleton. Notably, the nose tends to lengthen and the lips move down relative to the teeth so, over time, less of the maxillary and more of the mandibular incisors become exposed on smiling; the fullness of the lips also decreases. An increase in chin prominence is common in males, whereas in females, the chin may become more retrusive or show minor change.
Occlusal development
What follows is an account of normal occlusal development: the changes one would expect to see in the ‘average’ child. It is important to appreciate the range that exists within normal boundaries, so that developing problems may be recognised early and appropriate orthodontic intervention planned, if required. A thorough knowledge of the calcification and eruption dates of the 20 primary and 32 permanent teeth is essential (see Tables 7.1 and 7.2, p. 194). As well as allowing comparison of dental and chronological age, this information also helps to identify the timing of any insult that has led to alterations in the enamel or dentine mineralisation and indicates if a tooth that is absent radiographically is likely to develop.
Development of the primary dentition
The gum pads, containing the primary teeth, enlarge and widen following birth, with the lower lying slightly behind the upper by the time the first primary teeth (lower incisors) start to erupt at about 6 months of age. These are followed closely by the other incisors. The first primary molars erupt 3–4 months later, followed by the primary canines and the eruption of the second primary molars at about 3 years. The incisors tend to be upright, and anterior spacing is normal. Spacing is most common mesial to the upper canine and distal to the lower canine – the anthropoid or primate spaces. With a 1–2 mm increase in the intercanine distance, spacing between the incisors often increases as the child grows. In the absence of generalised spacing of the primary teeth, crowding of the permanent teeth is likely. The overbite, which is often initially ‘deep’ in terms of lower incisor crown coverage, reduces, and by 5 years of age an edge-to-edge occlusion with incisor attrition is common.
Development of the permanent dentition
At about 6 years, the eruption of the first permanent molars, followed by the permanent incisors, signifies the transition from the primary to the permanent dentition, commonly referred to as the ‘mixed dentition phase’. The permanent successors are slightly larger than the primary teeth and the first permanent molars need to be accommodated. Existing space is present between the primary teeth. Additional space is provided by minor modifications in arch length, arch width and intercanine distance (Table 9.1). Once the primary dentition is fully erupted, however, the dental arch size remains more or less constant anteriorly apart from a modest change in shape with some growth in the intercanine distance. In addition, growth at the back of the arches is necessary to accommodate the permanent molars and to maintain the arch relationship while the face grows vertically.
Table 9.1
| Characteristic | Measurement | Developmental changes |
| Arch length | Perpendicular distance from 1/1 contact point to a line contacting the distal surfaces of e/e or 5/5 | Maxilla: slight increase 6–10 years; followed by a 1–2 mm decrease Mandible: no increase 6–10 years; at 10–17 years, 1–2 mm decrease |
| Arch circumference | Line drawn through the buccal cusps and incisal edges of the teeth from the distal surface of e/e or 5/5 | Maxilla: ~1 mm increase in male; ~0.5 mm increase in female Mandible: ~3.5 mm decrease in male; ~4 mm decrease in female |
| Intercanine width | Distance between the cusp tips of c/c or 3/3 | Maxilla: ~1–2 mm increase from 3–6 years; ~3.5 mm increase from 6–12 years Mandible: ~1–2 mm increase from 3–6 years; ~3 mm increase from 6–10 years |
| Arch width | Distance from the palatal/lingual cusps of second primary molars or 5 | Maxilla: ~2–3 mm increase from 3–18 years; greater in males than females Mandible: ~3.6 mm increase from 3–18 years in both males and females |
The permanent lower incisors develop lingual to their predecessors and are frequently misaligned on eruption, but this usually resolves with intercanine growth. The upper anterior teeth develop palatal to their primary predecessors and are accommodated:
• by the existing spacing in the arch
• by erupting downwards and slightly forward so that they are placed on a wider arc
• by a small increase in intercanine distance (see Table 9.1).
The upper permanent lateral incisors usually move distally and labially with eruption of the central incisors, but they may be trapped palatally in crowded arches. The upper central incisors are often distally inclined when they first appear. An associated diastema tends to reduce as the lateral incisors erupt. At this time, the upper central and, to a greater extent, the lateral incisors are divergent, the latter because of pressure on their roots from the unerupted canines; this has been referred to as the ‘ugly duckling’ phase of dental development, terminology that is best avoided in the company of concerned parents.
The maxillary canines migrate from their palatal developmental position to lie labially and distally above the roots of the lateral incisors, leading to approximation of the incisor crowns as they erupt.
The combined mesiodistal widths of the primary canines and molars in each quadrant are slightly greater than those of the permanent canines and premolars. This difference in dimension is known as the ‘leeway space’ and is about 1 mm in the upper arch and 2.5 mm in the lower arch. The larger leeway space in the lower arch, probably in combination with mandibular growth, allows greater forward movement of the lower first permanent molar, converting a ‘flush terminal plane’ relationship of the primary molars to a class I occlusion (see below).
Six features (keys) of a good (‘ideal’) permanent occlusion have been described by Andrews:
• Molar relationship: the mesiobuccal cusp of the upper first molar lies in the groove between the mesiobuccal and middle cusp of the lower first molar; the distal surface of the distobuccal cusp of the upper first molar contacts the mesial surface of the mesiobuccal cusp of the lower second molar; the mesiolingual cusp of the upper first molar occludes in the central fossa of the lower first molar.
• Crown angulation: mesial for all teeth.
• Crown inclination: labially for incisors; lingually for canines through molars.
In addition, the following functional occlusal relations should exist:
Maturational changes in the occlusion
The occlusion of any child must be seen as dynamic and responding to changes in the facial skeleton. As the face continues to grow throughout the late teens and into adulthood, changes in the dentition and occlusion follow:
• There is an increase in lower incisor crowding. This has been observed even in children with previously well aligned, spaced arches and can be regarded as normal. Factors implicated in its aetiology are listed in Table 9.2.
Table 9.2
Factors implicated in late lower incisor crowding∗
| Factors | |
| Skeletal | Increase in mandibular prognathism Mandibular growth rotations Minimal forward maxillary growth |
| Soft tissue | Increase in soft tissue tone of lips and cheeks Trans-septal fibre contraction |
| Dental/occlusal | Lack of approximal attrition Dento-alveolar disproportion Tooth size Mesial drift secondary to anterior component of occlusal force, eruptive force of third molars Uprighting of posterior teeth in response to increase in lower facial height Third molars prevent posterior teeth shifting distally relative to the mandibular body in late mandibular growth |
• The interincisal angle increases, with uprighting of the incisors.
9.2 Malocclusion: classification and aetiology
Malocclusion is an unacceptable deviation either aesthetically and/or functionally from the ideal occlusion. Prevalence of malocclusion varies with age and racial origin as well as according to the assessment methods, but not all malocclusion requires treatment.
Classification of malocclusion
Classification for diagnosis
Angle’s classification
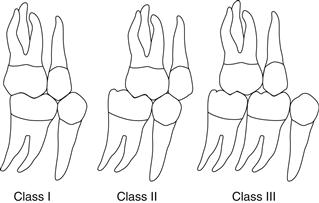
Angle’s classification is based on the first permanent molar relationship (Fig. 9.3).
Class II (also referred to as postnormal occlusion or distocclusion). The mesiobuccal cusp of the upper first permanent molar occludes anterior to the buccal groove of the lower first permanent molar.
Angle believed that the anteroposterior dental base relationship could be assessed reliably from the first permanent molar relationship, as its position, he maintained, remained constant following eruption. As this tenet is incorrect and difficulties arise in classification where mesial drift or loss of a first permanent molar has occurred, other classification systems are now used to categorise the anteroposterior dental base relationship.
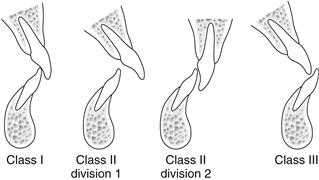
British Standards Institute classification
The British Standards Institute classification relates to the incisor relationship (Fig. 9.4).
Classification to assess treatment need and treatment outcome
Index of Orthodontic Treatment Need (IOTN)
The IOTN was developed to help to identify those malocclusions most likely to benefit in dental health and appearance from orthodontic treatment. It comprises two components.
The dental health component
Malocclusion is categorised into five grades (Table 9.3) based on the severity of occlusal characteristics that could increase the morbidity of the dentition and impair function. Grading, in relation to treatment need, is according to the single worst feature of a malocclusion.
Table 9.3
The Index of Orthodontic Treatment Need: dental health component
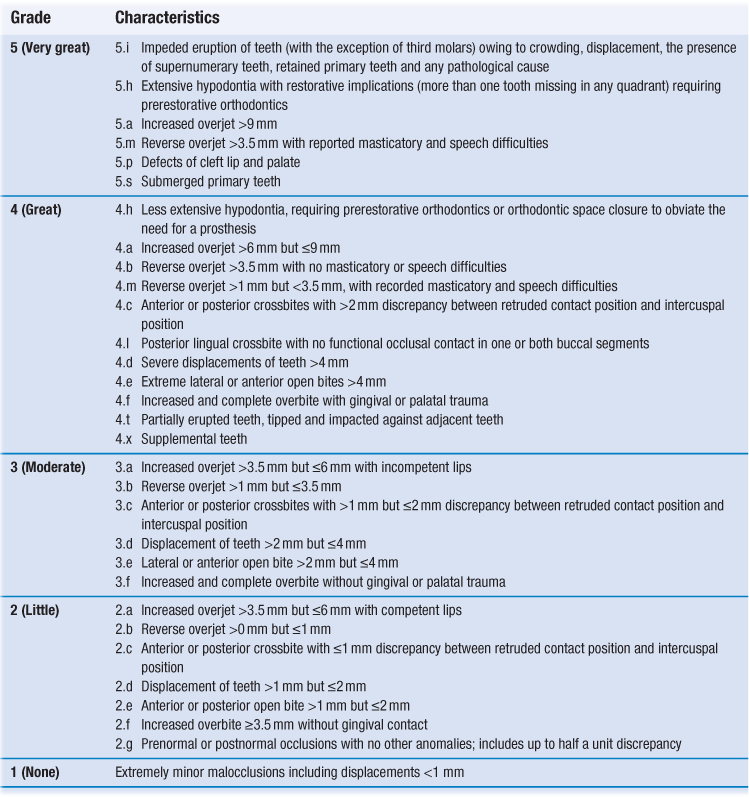
Reprinted from Brook P.H. and Shaw W.C., The development of orthodontic treatment priority, European Journal of Orthodontics, 1989, 11(3): 309-320, by permission of Oxford University Press
Table 9.4
Definition of commonly used cephalometric points and planes (Fig. 9.11)
| Points and planes | Definition |
| S | sella: midpoint of sella turcica |
| N | nasion: most anterior point of the frontonasal suture (may use the deepest point at the junction of the frontal and nasal bones instead) |
| P | porion: uppermost, outermost point on the bony external auditory meatus (upper border of the condylar head is at the same level, which helps location) |
| O | orbitale: most inferior anterior point on the margin of the orbit (use average of the left and right orbital shadows) |
| ANS | tip of the anterior nasal spine |
| PNS | tip of the posterior nasal spine (pterygomaxillary fissure is directly above, which helps location) |
| A | A point: most posterior point of the concavity on the anterior surface of the premaxilla in the midline below ANS |
| B | B point: most posterior point of the concavity on the anterior surface of the mandible in the midline above pogonion |
| Pog | pogonion: most anterior point on the bony chin |
| Me | menton: lowermost point on mandibular symphysis in the midline |
| Go | gonion: most posteroinferior point at the angle of the mandible (bisect the angle between tangent to the posterior ramus and inferior body of the mandible to locate) |
| S–N line | line drawn through S and N |
| Frankfort plane | line connecting porion and orbitale |
| Maxillary plane | line joining PNS and ANS |
| Mandibular plane | line joining Go to Me |
| Functional occlusal plane | line drawn between the cusp tips of the first permanent molars and premolars/primary molars |
To facilitate the grading process, a ruler (Fig. 9.5) has been developed. Occlusal features are assessed in the following order:
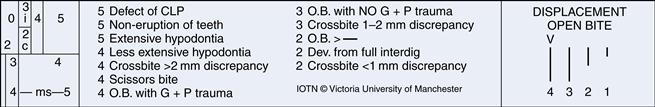
Fig. 9.5 The IOTN ruler (not drawn to scale).
Occlusal features are assessed in the order given by the acronym MOCDO. M = missing teeth; O = overjet; C = crossbite; D = displacement of contact point (i.e. crowding); O = overbite. (Reproduced by kind permission of Ortho-Care (UK) Ltd.)
The order above gives rise to the acronym MOCDO. With practice, it is possible to ascribe reliably and easily the treatment need category to a given malocclusion.
The aesthetic component
The aesthetic component of the IOTN (Fig. 9.6) consists of a set of ten photographs of anterior teeth in occlusion with increasing aesthetic impairment. These comprise class I and class II malocclusions; class III malocclusion and anterior open bite are not represented. Depending on whether the assessment is made clinically or from study models (with the anterior teeth in occlusion), colour or black and white photographs are used respectively. To categorise the treatment need, a score is given by selecting the photograph thought to be of an equal aesthetic handicap (and likely psychological impact on the patient), but judgement is very subjective. For this reason, treatment need tends to be based primarily on the dental health component of IOTN.
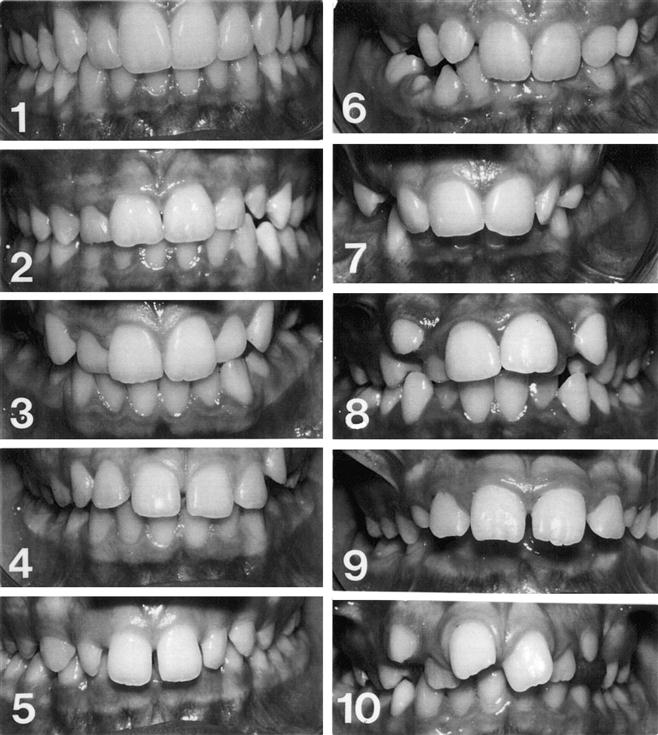
Fig. 9.6 The aesthetic component of the IOTN.
The need for treatment is categorised by subjective judgement based on the photographs: Score 1 or 2 = no need; 3 or 4 = slight need; 5–7 = moderate/borderline need; 8–10 = definite need. The Aesthetic Component was originally described as “SCAN” and was reprinted from Evans, R., and Shaw, W., Preliminary evaluation of an illustrated scale for rating dental attractiveness, European Journal of Orthodontics, 1987, 9(4):314-318, by permission of Oxford University Press
To assess treatment outcome
Assessment can be carried out objectively by applying the dental health component of IOTN and subjectively by application of the aesthetic component. In addition, the Peer Assessment Rating (PAR) may be recorded. A score is given to the pre- and post-treatment occlusion from the study models. The components and their weightings (by which the score is multiplied) are: crowding (×1), buccal segment relationship in anteroposterior, vertical and lateral planes (×1), overjet (×6), overbite (×2) and centrelines (×4). Measurement is facilitated by use of a specially designed ruler.
The percentage change in PAR score, obtained from the difference in pre- and post-treatment scores, is a measure of treatment success. A reduction of greater than 70% indicates a ‘greatly improved’ occlusion while a ‘worse/no different’ assignment is indicated by less than or equal to 30%.
To assess treatment need and complexity of treatment
In recent years, a new index, the Index of Complexity, Outcome and Need (ICON), has been developed. This incorporates scores for: the aesthetic component of IOTN (x7); upper arch crowding/spacing (x5); crossbite (x5); overbite/open bite (x4) and buccal segment relationship (x3). To indicate the improvement grade which reflects the outcome of treatment, 4× the post-treatment score is subtracted from the pretreatment score (intended to reflect need for and likely complexity of treatment).
Aetiology of malocclusion
A general overview of the aetiology of malocclusion is presented here while specific aspects related to the aetiology of each malocclusion type are considered in Chapter 10.
The aetiology of malocclusion is often the result of several interacting factors. These are principally genetic and environmental, although the precise role of inherited factors is not fully understood. Whereas the craniofacial dimensions and both size and number of teeth are largely determined genetically, the dental arch dimensions are influenced more by environmental factors.
Specific congenital defects with a genetic basis, which involve the maxilla or mandible, are rare, as is malocclusion caused primarily by trauma or pathology.
Skeletal problems
The majority of anteroposterior skeletal problems are caused by inherited jaw proportions, which are strongly genetically determined. Inherited characteristics (e.g. mandibular deficiency) account for almost all of moderate class II malocclusion, while the added insult of environmental soft tissue influences is likely in more severe cases. For class III malocclusion, mandibular prognathism has a strong racial and familial tendency although mandibular posturing, possibly caused by tongue or pharyngeal size, may stimulate growth and influence jaw size secondarily. Maxillary deficiency is also most likely due to inherited jaw dimensions and a simple environmental factor seems unlikely, but its exact aetiology is almost completely unidentified.
Vertical jaw proportions are also inherited, but soft tissue postural effects (e.g. anterior tongue position or mandibular postural changes induced by partial nasal obstruction) may contribute in particular to anterior open bite. Other environmental influences, such as a high lower lip line, may contribute to deep overbite.
A unilateral crossbite with displacement is often caused by a functional alteration, but it is usual for a skeletal crossbite to have an additional genetic input.
Crowding
Crowding is the most common orthodontic problem and is caused in part by a reduction in jaw and tooth size over the centuries. Interpopulation breeding has also been implied as arch width is influenced by jaw size, which is under tight genetic control.
Environmental influences, for example early loss of primary teeth due to caries or trauma or a digit-sucking habit, may also be instrumental in the aetiology of crowding. Also implicated is a softer, less abrasive modern diet which results in less interproximal tooth wear and less demands on jaw function; the latter may have added to a general tendency for smaller jaw size which was already happening. Soft tissue pressure of sufficient duration (more than 6 hours per day) in combination with the developmental tooth position may be responsible for a localised crossbite or malalignment.
9.3 Patient assessment in orthodontics
Orthodontic diagnosis consists of a list of all aspects that deviate from normal in relation to a particular occlusion. It is a prelude to treatment planning as it allows the relationship between the various factors and their likely impact on treatment and prognosis to be considered. Diagnosis is based on the accurate gathering of information about the patient from a logical case assessment.
Assessment
Timing
At 7–8 years, an assessment of the developing occlusion should be undertaken to note, in particular, the form, position and presence of the permanent incisors and to plan appropriate intervention should an abnormality be detected that is likely to interfere with the normal eruption sequence. The prognosis of the first permanent molars should be assessed routinely from age 8 years, and palpation of the maxillary permanent canines is carried out on a regular basis from about 10 years. Early detection of a skeletal discrepancy will allow also for optimal timing of treatment to maximise growth potential but, in most children, assessment is delayed until the permanent dentition has erupted.
All general dentists should be able to carry out a basic orthodontic assessment for their patients and recognise when referral to a specialist is appropriate. When dental and/or occlusal development deviates from normal, or when significant discrepancies in established dentofacial or occlusal relationships concern the patient and may compromise dental health over the long term, referral is indicated.
Apart from basic personal details, including relevant history with regard to medical, dental and social factors, the referral letter should give a brief summary of the salient features of the malocclusion incorporating the incisor and molar classifications (see Section 9.2). It should also include specific reference to:
• the patient’s perception of the problem
• the level of dental awareness including that of the parents (if appropriate)
Any recent radiographs should be forwarded with the referral. Study models are also of great assistance with treatment planning.
Orthodontic assessment comprises three stages:
Demand for treatment
The demand for orthodontic treatment is influenced by two main factors:
In general, demand for treatment is greatest when the orthodontist:population and orthodontist:general dentist ratios are small. Overall demand is increasing in adults, is higher in females, in those from better socioeconomic backgrounds and when a lower orthodontist:population ratio exists, as appliances become more common and their acceptance increases.
History
Initially the dentist must identify:
It is important to document whether the patient is unconcerned with the appearance of their teeth, particularly in the presence of obvious malocclusion, as any attempt to persuade the patient to undertake treatment is likely to be met with indifference. Attitude to treatment is best assessed from response to enquiries about their perception of orthodontic treatment for their peers, and by observing carefully their reaction when shown photographs or examples of appliances. Adults usually have a high level of dental awareness, are able to specify their concerns and motivation is high for treatment.
Medical history
A health questionnaire should be completed by each patient or a parent, and the findings verified by a clinical interview. Several medical conditions may impact on orthodontic treatment. Some are given below; where any uncertainty exists, liaison with the relevant medical specialist(s) is required.
Rheumatic fever/congenital cardiac defects
It is wise to consult the patient’s cardiologist to ascertain the need for antibiotic prophylaxis.
Recurrent oral ulceration
Appliance therapy should be avoided until this condition has been investigated thoroughly. Depending on the frequency and nature of ulceration, limited appliance treatment may be possible.
Epilepsy
Due to the risk of airway obstruction from appliance parts fractured during an epileptic attack and the difficulty with tooth movement in the presence of gingival hyperplasia, no orthodontic appliance should be fitted until the epilepsy is well controlled and the gingival condition healthy.
Diabetes
Patients with diabetes are more prone to periodontal breakdown, and active appliance therapy should be withheld until the periodontal condition is sound and the diabetes is stabilised.
Hay fever
Hay fever may interfere with the wearing of functional appliances over the summer months. An alternative approach to treating the malocclusion may be sought.
Nickel allergies
In patients with a confirmed severe hypersensitivity to nickel, nickel-free brackets and wires should be used; in some cases, clear aligner therapy may be considered as an alternative.
Latex allergy
Latex-free gloves, elastomeric separators, modules/chain, intraoral elastics and headgear components should be used.
Bleeding diatheses
If extractions are necessary, special medical arrangements will need to be in place.
Severe physical/mental handicap
In selected patients, extractions only may produce an improvement in dental aesthetics and facilitate tooth-cleaning measures. Appliance therapy is invariably not a viable option.
Arthritis or osteoporosis
Because juvenile or adult-onset rheumatoid arthritis often requires management with chronic steroid administration, lengthy orthodontic treatment is inadvisable due to the increased possibility of periodontal problems arising.
Oral doses of prostaglandin inhibitors or resorption-inhibiting agents (bisphosphonates) may be administered to adults being treated for arthritis or osteoporosis respectively; tooth movement may be affected. Orthodontic treatment and extractions are contraindicated if bisphosphonates are given intravenously due to the osteonecrosis risk.
Dental history
The nature, extent and frequency of previous dental treatment together with the level of patient co-operation should be recorded, along with details of daily oral hygiene practices. A history of early loss of primary teeth or of incisor trauma should be noted. If orthodontic treatment has been carried out previously, details relating to extractions and appliance type should be recorded. If treatment was abandoned, the patient must be questioned carefully for the reasons.
Social history
The ease with which regular appointments can be attended and any forthcoming events that may influence attendance should be noted.
Clinical examination
Before the child patient takes a seat in the dental chair, it is often worthwhile to attempt to estimate their chronological age from their height and general level of physical maturity. This may give some indication of future growth potential. If the patient is accompanied by a parent, obvious familial malocclusion traits may be observed. The purpose of the clinical examination is to assess and record facial, dental, occlusal and related functional aspects of a patient in order to request appropriate diagnostic aids. An extraoral followed by an intraoral examination should be performed.
Extraoral examination
The skeletal pattern, soft tissues of the lips, tongue position during swallowing, speech, temporomandibular joints and mandibular path of closure should be assessed and the presence of any habits noted.
The relationship of the mandible to the maxilla should be assessed in all three planes of space: anteroposteriorly, vertically and laterally. Before proceeding, it is important to ensure that:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses