Conservative dentistry
Chapter Contents
3.1 Examination, diagnosis and treatment planning
3.2 Caries management and direct restorations
Overview
This chapter reviews current methods for the repair and replacement of teeth using direct and indirect restorations. These contemporary techniques have evolved more or less simultaneously with developments in dental materials. The selection, properties, advantages and disadvantages of various materials are discussed.
3.1 Examination, diagnosis and treatment planning
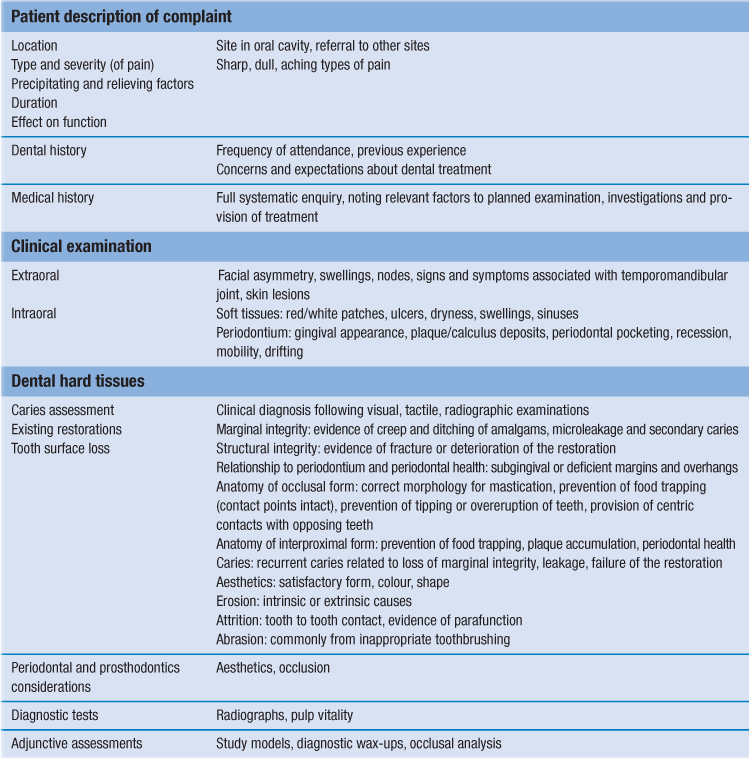
Examination of patients with a view to carrying out conservative procedures should follow the general principles for dental examination and history taking; treatment should address the underlying aetiology of the pathological process (Table 3.1).
Relevant anatomy
A knowledge of the anatomy and morphology of the dentition is essential in order to be able to recreate the shape and form of those teeth that require restoration. The properties of enamel and dentine allow us to understand how dental disease is initiated and progresses.
Enamel
Enamel provides a hard durable outer coating of teeth. It is an important element in defining the aesthetics of the dentition because of its opalescent/translucent qualities. Its highly crystalline structure (95–98% inorganic component by mass), while conferring important aesthetic qualities to the tooth, makes enamel particularly prone to acid demineralisation, both from caries and erosion. It is also brittle and liable to fracture, especially if unsupported by the more elastic dentine.
The inorganic component comprises 86–95% hydroxyapatite by volume. The organic component comprises 1–2%, while water contributes 4–12%. The rods and prisms are the main structural units of the material and are generally orientated at 90° to the external surface. Consequently, finishing of cavity margins and the interface with restorations should aim to provide maximum strength for the restorations and the supporting tooth structure.
Dentine
Dentine comprises 45–50% inorganic hydroxyapatite crystals, with 30% organic matrix and 25% water. Its shade varies through various hues of yellow and it is vital, elastic and permeable. As a result, it is not possible for any restorative material to provide a completely hermetic seal between itself and the cavity wall, although recent advances in bonding agents have significantly improved this.
Dentine consists of:
Dentinal vitality and its pathological derivative, hypersensitivity, have been hypothesised to arise from capillary action, differential thermal expansion or diffusion. No specific nerve endings lie within tubules; therefore, the ability of dentine to react to thermal stimuli is related to hydrodynamic fluid movement by which a thermal gradient results in fluid flow within the tubules (either into or out of the tooth substance) and this leads to a reaction of the tooth to this stimulus.
As a vital tissue, dentine continues to be deposited throughout life as secondary dentine, although at a slower rate than primary dentine. Deposition of irregular secondary dentine or tertiary dentine may result from chronic low-grade trauma such as attrition, erosion, abrasion, slowly progressive caries and tooth preparation.
Dental caries
Caries can be defined as progressive dissolution of the inorganic component of dental hard tissues mediated by dental plaque. The acidic demineralisation leads to cavitation and bacterial invasion, with progressive demineralisation. A pH level of less than 5.5 is required for demineralisation to occur.
It is possible for remineralisation to occur at neutral pH. This is achieved by the buffering capacity of both saliva and plaque with calcium and phosphate ions available at the tooth surface. The equilibrium between remineralisation and demineralisation depends upon the composition and thickness of the plaque, the frequency and character of sugar intake and the composition and flow rate of saliva. Fluorides have a modifying effect.
Aetiology and modifying factors
Bacteria
Specific bacterial species are identifiable as being involved in caries development, especially Streptococcus mutans, Streptococcus sobrinus and Lactobacillus spp. This involvement has been confirmed by gnotobiotic studies, effectiveness of antibiotics and in vitro studies of enamel demineralisation by oral bacteria.
Diet
Bacteria require a source of dietary carbohydrates, the frequency of consumption being more important than the quantity. Increased frequency leads to increased periods of pH reduction (Stephan curve) and demineralisation. Adherence of plaque is also important, with sticky carbohydrate producing particularly tenacious deposits.
Medical history, medication and salivary flow
Saliva has a protective effect in oral clearance of foodstuffs and in its buffering capacity. Some medical conditions directly cause a decrease in salivary flow, e.g. Sjögren’s syndrome and sarcoidosis. With an increasingly ageing population, many patients present with medical conditions controlled by prescription medications; a common side effect of many drugs is xerostomia (dry mouth). The most common groups of drugs causing dry mouth include antihistamines, antidepressants, antimuscarinics and antipsychotics. Relevant medical conditions, e.g. cerebrovascular events, rheumatoid arthritis and CNS disorders, may directly impact the ability to perform optimal plaque control or render them reliant on carers to aid with oral hygiene.
Salivary flow will also be severely reduced in those treated for head and neck cancer with radiotherapy and/or surgery to the major salivary glands. Significant emphasis on caries prevention is therefore required.
Development and progression
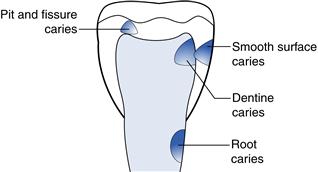
Caries can develop (Fig. 3.1):
• in pits and fissures, where it has a small site of origin with a wide base (inverted ‘V’)
Early enamel caries is subsurface: a ‘white spot’ with an intact surface with demineralisation occurring at a deeper level. The very early lesion progresses from shadowing to white spot to brown spot and surface breakdown, with resultant cavitation. Dentine caries progresses more rapidly because of the decreased resistance to acid dissolution. This is particularly evident with root caries.
Clinical diagnosis of caries
Diagnosis can be:
Caries management and prevention
Management varies with the stage of progression. A preventive approach is indicated for all patients presenting with caries but a combination of approaches may be required depending on risk and the presence of a fluoridated water supply (Box 3.1).
Fluoride
Adults at high risk of dental caries should be recommended or prescribed fluorides in order to modify their risk of caries. In surgery, fluoride varnish (22 600 ppm F–) may be applied on a quarterly basis by dentists or under prescription by therapists, hygienists or nurses with additional training. Alternative routes of administration most appropriate to adults are through topical application via daily or weekly mouthwashes and toothpastes.
Early white spot lesions and root caries lesions may respond to improvement in oral hygiene, modifying diet and through the use of fluorides. Cavitated lesions will usually require restoration and teeth of hopeless prognosis should usually be removed.
Tooth Wear
Aetiology
Tooth wear or tooth surface loss is a significant problem in patients of all ages; determining the aetiology is key to its successful management. There are three main categories of tooth surface loss reported in the literature: erosion, abrasion and attrition. These often occur in combination and the aetiology is multifactorial. The rate of progression of tooth wear, particularly from erosion, may be increased with xerostomia due to the decreased buffering capacity. There is some limited evidence for one further type of tooth surface loss, abfraction, that has also been reported in the literature.
Erosion
Dental erosion is attributed to the pathological loss of tooth tissue through acidic dissolution, but importantly not through the action of plaque bacteria. The clinical pattern of tooth wear often suggests the source of acid as either intrinsic, extrinsic or occupational (environmental):
Abrasion
Abrasion is tooth wear from extrinsic sources, for example toothbrushing (especially cervically in areas of gingival recession) and ‘occupational’ for those working in a dusty environment with inadequate protection.
Attrition
Attrition is tooth wear from tooth to tooth or tooth to restoration contact. Although physiological tooth wear occurs throughout life, parafunctional activity such as bruxism causes pathological wear. The clinical appearance of attrition develops initially as faceting and progresses to rounding of cusp tips and flattening of the occlusal surfaces and incisal edges. Rapid rates of wear may be observed if there is significant loss of posterior support and in natural teeth opposing unglazed or roughened porcelain.
Abfraction
Some lesions cannot be explained by erosion, abrasion or attrition. Abfraction has been defined as the pathological loss of tooth tissue resulting from biomechanical loading forces. Flexure and microfractures result in the failure of dentine and enamel at and around the cementoenamel junction.
Diagnosis
Diagnosis is achieved by clinical observation and history. Some aetiological factors can be difficult to elucidate (e.g. erosion arising from eating disorders) for obvious reasons, but careful and sympathetic questioning may allow this to be discovered.
Management
The first stage in management of tooth wear is to identify the aetiology and, where possible, modify or preferably eliminate the causative factor(s). This may involve education of the patient and provision of:
Thereafter, intervention is governed by the extent of the damage sustained by the dentition. Simple maintenance and monitoring are often the best policy where limited damage has occurred, and may include:
• analysis of accurate study casts and/or simple silicone indices
• provision of protective appliances (soft vinyl or hard acrylic mouth guards)
• adhesive restorations applied to the worn surfaces
• treatment of sensitivity, topical fluoride application and oral hygiene advice.
Active treatment requires careful planning, looking at all aspects of the dentition and its prognosis. It may involve:
If significant loss of tooth substance has occurred and dentoalveolar compensation has occurred, a reorganised approach may be considered.
3.2 Caries management and direct restorations
The destruction of tooth substance by caries or other factors requires restoration of lost tooth substance. This usually necessitates preparation of a cavity within that tooth to support and retain the chosen restorative material. GV Black classified the carious lesions by location. As restorations essentially conform to caries location, the cavities requiring preparation are similarly classified.
Black’s classification
Class II: proximal surfaces of molars or premolars.
Class III: proximal surfaces of incisors or canines.
Class IV: proximal surfaces of incisors.
Class VI: occlusal or incisal cusp tip wear (an addition to the original classification).
Cavity preparation requires instrumentation of a tooth to remove caries or any other congenital or acquired defects to allow placement of an appropriate restorative material that will re-establish form, function and/or aesthetics; retention and resistance form must be considered depending on the size of cavity and restorative material indicated for restoration.
Indications for restoration
Objectives and stages of cavity preparation
Access
Access should be sufficient to allow adequate visualisation of caries and to allow complete removal. It should also aim to retain as much sound tooth substance as is compatible with this objective. All stained and softened tooth substance should be regarded as carious. Stained and firm tooth substance requires careful evaluation before removal. Staining at the enamel–dentine junction should be removed wherever possible. The need for lining materials should also be evaluated to provide pulpal protection when deep excavation has occurred.
Outline form
Margins should be placed in areas accessible for cleaning and maintenance at a position on the tooth where functional loading will not adversely affect the restoration/tooth interface. Outline form should be compatible with the chosen restorative material’s properties and enamel unsupported by underlying dentine should be removed to reduce the risk of fracture under functional loading and subsequently restoration failure.
Adequate resistance/retention form
Resistance form is defined as an aspect of cavity design whereby both the restoration and tooth should, upon completion of the restoration, be able to withstand functional forces.
Retention form results from opposing cavity walls being parallel or slightly convergent to resist any forces that will tend to dislodge the restoration from the cavity.
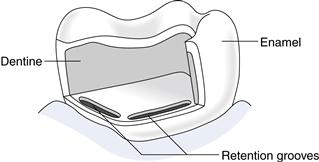
Historically, dentine pins have been utilised to provide additional retention to restorations, although placement has been shown to exert considerable stresses on the tooth. The use of bonding systems with resin composite and amalgam restorations coupled with the placement of small pits and grooves in the cavity floor and/or walls have made the use of pins obsolete (Fig. 3.2).
Cavity design in anterior teeth
The design of cavities for anterior tooth restoration should be governed by the extent of caries, as adhesive technology has, in most cases, superseded the need for incorporation of retentive elements such as grooves or slots. This allows retention of the maximum amount of tooth substance and therefore retains strength and aesthetics of the restored tooth.
Caries removal remains a priority especially at the enamel–dentine junction. The use of a lining material that is compatible with the final restorative material (i.e. not a liner based on zinc oxide/eugenol with composite materials) is necessary in deeper cavities. Calcium hydroxide bases (Life, Dycal) are useful, although more recent innovations in light-cured glass ionomer and compomer (combined glass ionomer and composite resin materials) also provide a satisfactory lining and often a better seal with the tooth substance because of their adhesive nature.
Cavity design in posterior teeth
These largely conform to Black’s classification I, II, V and VI. As with anterior direct restorations, cavity form should now be governed by the extent of the caries and the material to be used. Cavity preparation should therefore be as conservative as possible. Where direct posterior composite materials are used, the question of bevel placement remains controversial. Where enamel is available, the bevel will provide more area for acid etching and bonding. Additionally, the bevelling will result in exposure of transversely cut enamel rods, resulting in a significantly stronger bond being created. However, the bevelling also results in formation of very thin sections of composite that are vulnerable to occlusal stress. As such, occlusal placement of bevels should be avoided at points on the surface where occlusal stops may be present.
The placement of bevels is more appropriate at some sites of a cavity than others. A bevel of less than 1 mm on the buccal or lingual cavo–surface margin of a box improves retention and bonding and allows margins to be more accessible for finishing. Placement of a bevel at the gingival margin of the box is more technically demanding and there may also be limited enamel remaining. Accordingly, the gingival margin should only be bevelled when it is well above the enamel–cementum junction.
3.3 Materials for direct restorations
Amalgam
Amalgam has been used for over 150 years. The continued use of amalgam has become a controversial topic in recent years with concerns being raised about its safety, particularly in relation to the release of mercury during removal, placement, carving and, in the longer term, during chewing. There remains, however, considerable evidence to support its safety as a dental material, with no apparent firm scientific evidence to indicate an association with any systemic disease. Some EU countries have taken steps to ban its use but, at present, no direct restorative material exists that has the same ease of handling, relative cost-effectiveness and clinical serviceability.
Amalgam is an alloy of mercury with other metals. High copper alloys are most commonly used with 12–30% copper (by weight) in addition to silver, tin and zinc. The increase in copper levels results in elimination of the weak gamma 2 phase, which increases its tendency to corrode. The exclusion of moisture during packing of the restoration is highly desirable as moisture reduces the clinical effectiveness of the material.
Advantages
Amalgam has many advantages, such as:
Disadvantages
The disadvantages of amalgam are:
Adhesive dentistry and associated restorations
Adhesive techniques using composite resins have led cavity design away from the very prescriptive form originally described by Black, which often led to removal of excessive amounts of sound tooth substance. Minimal cavity preparations removing only caries-affected enamel and dentine are possible with subsequent replacement with resin-based restorative materials bonded to the tooth tissue.
Indications
Adhesive restorative techniques may be used for:
• restoration of carious cavities.
• aesthetic correction of dental anomalies (e.g. shape, position, dimension, shade).
• bonding of ceramic or metal to tooth substance.
Advantages
Composite remains the most common material used for tooth-coloured, anterior, directly placed restorations. The demand of patients for increasingly aesthetic restorations has seen a significant rise in the use of composite materials for posterior restorations in recent years. However, as with most dental materials, they have both advantages and disadvantages. In order to evaluate these, an understanding of the biology of bonding is required.
Biology of bonding
Enamel bonding
Bonding to enamel is principally micromechanical. Use of mild acids such as phosphoric acid (30–40%) results in dissolution and removal of approximately 10 µm of the surface organic component of enamel and leaves a microporous layer of 5–50 µm. The pitted surface enables an unfilled resin bonding agent (usually a low-viscosity bisphenol-α-glycidyl methacrylate (bis-GMA acrylic) resin) to flow into the pits and form resin tags, which then provide micromechanical retention. The tags are either ‘macro-tags’ between the prism peripheries or ‘micro-tags’ formed at the core of prisms in the individual crypts of dissolved hydroxyapatite crystals. The latter contribute most of the bond strength. The bonding resin is then chemically bonded to a filled acrylic resin restorative material.
The etching effect of the acid is dependent upon:
Dentine bonding or conditioning
The higher organic component of the smear layer means that it must be removed and hydrophilic monomers (such as 2-hydroxyethylmethacrylate (HEMA)) are required.
Dentine remains ‘wet’ as a result of a persistent fluid exudate from the dentinal tubules that have been cut during instrumentation. Also, dentine tends to vary in its composition, with areas of sclerosis and hypermineralisation.
The aim of dentine conditioning is to demineralise the surface dentine gently and dissolve or modify the smear layer to expose a microporous scaffold of collagen fibrils. These tend to collapse without the support of the inorganic component.
The depth of demineralisation depends on:
Techniques for enamel and dentine bonding
Acid etching of enamel should be carried out using a 30–40% solution of phosphoric acid in a gel form, which is applied for no less than 15 seconds. The enamel is then washed for 10–20 seconds. Excessive exposure to more concentrated solutions for increased periods of time results in poorer bond strengths as the critical ‘tag’ structure is lost and a precipitate of monocalcium phosphate monohydrate forms.
The use of a drying agent has sometimes been suggested to remove more water from the etched pattern to improve resin penetration. Most primers tend to consist of a hydrophilic monomer dissolved in an organic solvent such as acetone or ethanol. This leads to displacement of water from the dentine surface, allowing improved infiltration of the monomer into the collagen network.
Dentine conditioning may be carried out using a range of acids for varying periods of time, but it always should avoid extreme demineralisation of the dentine. The acids used include 10–40% phosphoric acid, 2.5% nitric acid, 10% citric or maleic acids and 1.6–3.5% oxalic acid.
Total-etch technique
The total-etch technique involves using one of the above acids to achieve etching of enamel simultaneously with conditioning of dentine. Desiccation of the dentine surface is undesirable, with slight dampness allowing hydrophilic materials to bond more successfully.
Self-etching acidic monomer primers or ‘condiprimers’ have been developed that form a continuum between the tooth surface and the adhesive material by simultaneous demineralisation and resin penetration with monomers and allow for the most recent ‘all-in-one’ self-etch or prime and bond techniques. These can be ‘air dispersed’ (but not rinsed) and polymerised by light activation in situ.
Bonding resins are used to link the resin primer to the restorative material. They are usually hydrophobic monomers based on the bis-GMA molecule or more hydrophilic monomers such as triethyleneglycol dimethacrylate (TEG-DMA) and HEMA. The resins act to stabilise the hybrid layer and form resin extension tags into tubules, providing retention (Fig. 3.3). They may be light or chemically cured. The light-cured types require the bonding agent to be applied before the restorative resin to avoid its displacement or inadequate curing through insufficient light intensity reaching the material. As a result of oxygen inhibition of curing, the most superficial 15 µm will remain uncured, but it still offers sufficient double methyl methacrylate (MMA) bonds for co-polymerisation of the adhesive resin to the restorative resin. Brush thinning of the material is preferred to air thinning to maintain sufficient film thickness to prevent the air-inhibited layer permeating the resin.
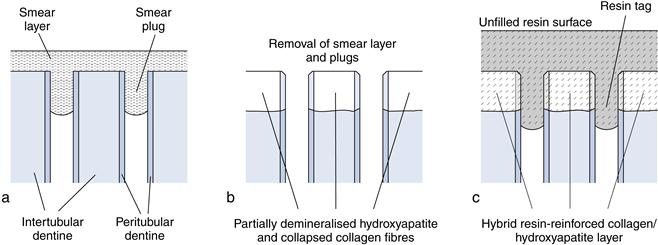
Fig. 3.3 Dentine conditioning and adhesion.
(a) Freshly cut dentine surface. (b) Conditioned dentine. (c) With bonding agent applied.
Adhesion or bonding of materials to enamel and/or dentine requires an intimate link between the restorative material and the tooth substance, with adequate ‘surface wetting’ to decrease surface tension. Bonding may occur by:
• weak physical electrostatic attraction (van der Waal forces)
• chemical bonding, with interatomic bonds developing across the tooth/restoration interface
The quality of bonding may depend upon:
• the materials being bonded and their properties
• the functional loads applied to the tooth and the restoration
Other factors affecting bonding include salivary pellicle and the ‘smear layer’ formed following instrumentation. The smear layer is defined as any debris, calcific in nature, that is produced by reduction or instrumentation of dentine, enamel or cementum.
Composite restorative materials
The material is based on a polymer resin matrix with filler particles, based on the bis-GMA resin developed by Bowen in 1962. A range of filler particles have been used, including quartz, fumed silica, barium, strontium, aluminium and zinc glasses and zirconia silica. The ratio of filler particles in composites varies, with the materials being defined as micro, mini, nanofilled or hybrid resins.
Microfilled resins usually incorporate fillers averaging 0.04–0.05 µm. Hybrid resin composites contain a mixture of submicron (0.04 µm) and small particle (1–4 µm) fillers, with a combination in most of glass particles and prepolymerised composite particles. These allow the maximum filler loading and, therefore, improved physical properties. Minifilled resins use a combination of 0.6–1 µm and 40 nm particles, while midifilled resins use 1–10 µm and 40 nm particles. Nanofilled resins with ultrasmall particles are now also being used (5–100 nm).
These inorganic filler particles increase the viscosity of the material, reduce polymerisation shrinkage and improve the surface finish. This allows high polishability, and the restorations can be used for maximum aesthetics. The filler content also makes the material more wear resistant, denser and harder; it also reduces the coefficient of thermal expansion. The coefficient of thermal expansion of composites is two- to six-fold higher than that of the tooth; as a result, thermocycling, as occurs during normal consumption of hot and cold foods and drinks, results in microleakage and loss of adhesion between the tooth and restoration.
The greater the filler content (volume or weight), the better the physical properties, although this has to be balanced by a reduction in clinical handling. The interface between resin and filler is a silane coupling agent. The material also incorporates an initiator to commence polymerisation and this may be mediated chemically or by light activation (usually visible light at the blue end (460–480 nm) of the spectrum). Chemically cured or dual cured composites are most often used as luting agents in resin retained bridgework, resin retained crowns or in restoration of root-filled teeth to retain fibre posts.
Physical properties
The development of composite restorative materials has progressed in recent years, resulting in materials that are aesthetically satisfactory, durable and handle well. They do, however, exhibit a number of properties that are undesirable. Polymerisation shrinkage can lead to a reduction in volume of up to 7% particularly of less filled materials and cause contraction forces of 4–7 MPa. The filler content reduces the amount of polymerisation shrinkage which can cause cracking or flexure of tooth substance. It can also lead to gap formation between the tooth and the restoration, causing microleakage, recurrent caries and sensitivity.
Sites deemed to be at further risk of caries (deep pits and fissures) can also be sealed at the same time as the restoration placement in so-called ‘preventive resin restorations’.
Posterior composites
Ongoing developments in composite technology have seen improvements in the compressive and tensile strengths of these materials for use in posterior teeth. Sufficient concerns remain about their wear resistance, setting characteristics and thermal properties to suggest that they should be used for posterior restorations with caution, following careful assessment of the tooth and occlusion.
Advantages of composite restorations
Aesthetics
Composite resins have been developed that give a wide range of shades, tints and opacity, allowing production of very aesthetically satisfactory restorations matching almost any natural tooth shade and appearance. Stability of this colour appears good, although extrinsic staining may result with time as a result of surface deterioration. Microfilled composites suffer less from this problem.
Reduced destruction of sound tooth substance
Adhesive technology allows limited removal of tooth substance beyond that required to eliminate caries and undermined enamel (preventive resin restorations). Tooth preparation differs from that for conventional amalgam cavities by being shallower and narrower (both of which reduce material volume and, therefore, polymerisation contraction). There is reduced undercutting of the cavity walls with rounding of internal line angles, thus reducing the development of stress and improving adaptation of the material during placement.
Further advantages include:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses