Paediatric dentistry I
Chapter Contents
Overview
The successful practice of paediatric dentistry requires an intimate knowledge of normal child development and behavior, as well as the technical and clinical skills that are necessary to work in a small mouth. The aim of every clinician who treats children should be to deliver that child into adolescence and young adulthood without fear and with tolerance for dental treatment. If that is achieved and, in addition, the young adult has an appreciation of the importance of oral health to overall general health, then the hours spent in behavior management and delivery of prevention will have been worthwhile.
7.1 Tooth development and eruption
Tooth development
Tooth germs develop from the dental lamina, which itself develops from the primary epithelial band. The dental lamina forms a series of epithelial buds that grow into surrounding connective tissue. The buds become associated with a condensation of mesenchyme and together they represent a tooth germ at its early ‘cap’ stage of development. The epithelial bud becomes the enamel organ and the mesenchymal cells the dental papilla and follicle. The cells at the margin of the enamel organ grow to enclose some mesenchymal cells, the ‘bell’ stage of development. Histodifferentiation of the enamel organ now forms the external and internal enamel epithelia, stratum intermedium and stellate reticulum.
On the lingual aspect of each primary tooth germ, the dental lamina proliferates to produce the permanent successor tooth germ. Permanent tooth germs with no primary precursors are produced by distal extension of the dental lamina.
Dentine formation occurs after differentiation of dental papilla cells into odontoblasts, which is induced by the internal enamel epithelium. Once dentine formation has begun, the adjacent cells of the internal enamel epithelium differentiate into ameloblasts and produce enamel. The dentine of the roots of teeth is produced in a similar fashion by differentiation of odontoblasts induced by the internal enamel epithelium, and root growth is controlled by the epithelial cells at the margins of the enamel organ – the root sheath of Hertwig. Root growth is not complete until 1–2 years in the primary dentition and 3–5 years in the permanent dentition after eruption of the crowns of the teeth. The beginning of mineralisation for both dentitions is given in Tables 7.1 and 7.2.
Table 7.1
Typical times for calcification and eruption of deciduous teeth
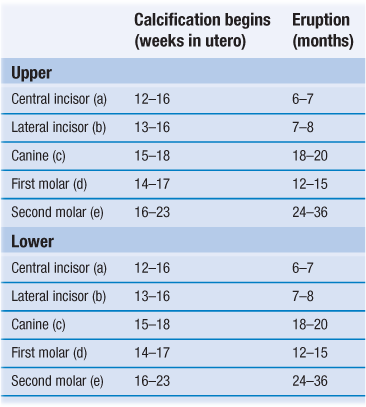
Root calcification is complete 1–1.5 years after eruption.
Typical eruption sequence is a, b, d, c, e.
Table 7.2
Typical times for calcification and eruption of permanent teeth
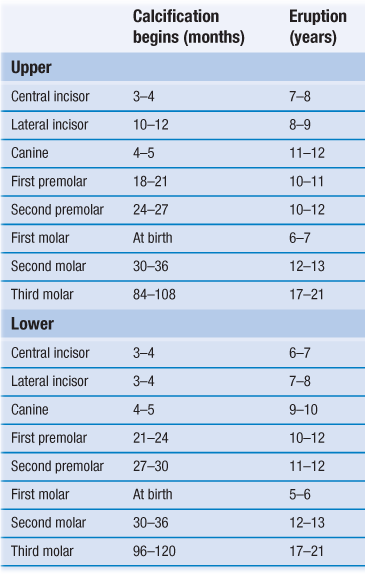
Root calcification is complete 2–3 years after eruption.
Typical eruption sequence: upper 6 1 2 4 5 3 7 8; lower 6 1 2 3 4 5 7 8.
Eruption
The exact controlling mechanism of eruption has not yet been identified. It is likely that the dental follicle has a major part to play as the connective tissue of the follicle is a rich source of factors responsible for the local mediation of bone deposition and resorption. Typical eruption times are given in Tables 7.1 and 7.2.
7.2 Management of the child patient
Psychological aspects
Child development
Development should be regarded as a continuum as it may differ from child to child. It is an uneven process and is influenced by periods of rapid bodily change. There are certain ‘psychological signposts’ that are important for the dentist and their staff to recognise.
Motor development
Motor development occurs in a predictable order and failure to attain ‘motor milestones’ enables remedial intervention that will aim to improve motor skills. The environment can influence motor development, and generalised motor development is completed in early life. Skills or changes that follow walking are refinements rather than new skills. Dominance of one hand emerges early. Motor retardation in a child may be manifested by no specific handed dominance. At 6–7 years of age, a child will have sufficient co-ordination to brush their teeth reasonably well. Below 6–7 years, many areas of the mouth will be inaccessible without parental help.
Cognitive development
Sensorimotor at 0–2 years
The infant can think of things as permanent without having to see them directly.
Preoperational at 2–7 years
Thought patterns are not well developed; the child is egocentric and inflexible.
Concrete operations at 7–11 years
The child can apply logical reasoning and consider another person’s point of view.
Formal operations at 11 years or older
Transition to adult thinking results in the development of logical abstract thinking and different possibilities for action can be considered.
Perceptual development
By age 7 years, children do develop selective attention and can determine which advice merits attention and which can be ignored. Concentration skills also improve. By age 9 years, children achieve adult proficiency.
Language development
Language and thought are inter-related and lack of stimulation will retard both. Keep dental jargon to a minimum and always assess patients before offering advice.
Social development
Separation anxiety is high until age 5 years and then declines rapidly so do not expect a child younger than this to enter the surgery on their own.
Adolescence
Increasing independency and self-sufficiency develops in adolescence. Young people do tend to be moody, are oversensitive to criticism and often feel miserable for no apparent reason. Therefore, do not criticise adolescents excessively and try to give them support and reassurance.
Parental influence and dental treatment
Parents are vital for positive reinforcement over any treatment objective. Programmes of treatment must be designed to reduce any chances of making parents or their children feel guilty. Design of treatment programmes should also allow goals to be achieved one by one, never overloading parent or child.
Dentist–patient relationship
Each patient is a unique individual and should be treated as such. Overall, it is fair to conclude that while the technical skill of a dentist is of concern, the most important factors for a patient are gentle friendly manner, explanation of treatment procedures and the ability to keep pain to a minimum.
The structure of the dental consultation
Anxious and unco-operative children
The extent of anxiety does not relate to dental knowledge but is an amalgam of personal experiences, family concerns, disease levels and general personality traits. It is, therefore, not easy to pinpoint aetiological agents and measure anxiety. In addition, there is no standard measure of anxiety.
Helping anxious patients cope
Several approaches can help to reduce coping problems:
Care programme
History involves social, medical and dental information
Social
Name, address, age, school, siblings, parental occupations. This allows the clinician to establish rapport. Try and assess social background, knowledge of dentistry and the family’s expectations.
Medical
Apart from allowing safe delivery of dental care, two additional factors can be gleaned: children with medical conditions may have a negative attitude to treatment because of the time they have spent in hospitals; they may also be more likely to fail dental appointments owing to the disruption in education that the medical problem has already caused.
Dental
Past dental experiences may give an indication of how the child will cope with proposed treatment. Parental attitude to treatment is important. A treatment plan must be modified to accommodate this. Establish exactly why they have come. The answers from child and parent may be different!
Examination
Clinical examination
The clinical examination need not involve sitting in the dental chair at the first visit. Examine the child as a person not just a mouth.
Extraoral
General appearance is noted; percentile charts are a useful way of monitoring height and weight. The head and neck are examined making a sketch of any lesions/marks.
Intraoral
Soft tissues may be an indicator of systemic disease. The relationship between periodontal condition and oral hygiene may indicate an underlying condition. Occlusion factors include crowding, malalignments, mandibular deviations and habits. The condition of the teeth is noted; they must be clean and dry in order to facilitate caries diagnosis.
Radiographic examination
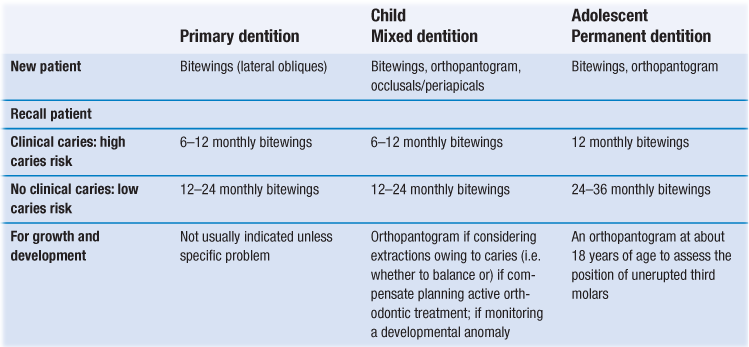
Guidelines for prescription of radiographs in children are shown in Table 7.3.
There are three general indications for taking radiographs in children:
Caries diagnosis
At least 50% more approximal lesions can be diagnosed by bitewing radiographs than with clinical examination. High-resolution digital orthopantogram (OPT) films at the appropriate setting (that which will separate the interproximal contacts) are efficient at diagnosing occlusal and approximal caries. Many standard OPT films are, however, still inadequate for caries diagnosis and, in this case, intraoral bitewing radiographs remain the method of choice.
Abnormalities in dental development
All children at age 8 or 9 years should have an OPT to identify disturbances in development of the dentition in terms of the number, position and form of the teeth. Precise location of maxillary canines can then be achieved by intraoral parallax technique.
Detection of bony or dental pathology
Periapical radiographs for individual teeth; OPT views for larger pathology or bony trauma.
Special investigations
There are a number of special tests that are sometimes relevant:
Treatment planning
Planning should incorporate:
• management of pain: consider all teeth of poor prognosis
• long-term treatment planning: to include attitudes and motivation
• preventive care: tailored to each individual
• restorative care: realistic aims are important
• aesthetic considerations: children can be under considerable peer pressure over their appearance.
7.3 Caries
Development of caries
Fermentation of dietary sugars by micro-organisms in plaque on the tooth surface produces organic acids. This rapid acid formation lowers the pH at the enamel surface below the level (critical pH 5.5) at which enamel will dissolve, a process known as demineralisation. When sugar is no longer available to the plaque micro-organisms, the pH within plaque will rise through the outward diffusion of acids and their metabolites. As a result, remineralisation of enamel can occur.
Dental caries progresses only when demineralisation is greater than remineralisation. The early caries lesion is subsurface with white surface demineralisation (precavitation). This may be because a layer of dental plaque on the tooth acts as a partial barrier to diffusion. Plaque forms on tooth surfaces that are not cleaned and is visually obvious within 2–3 days of ceasing toothbrushing. Plaque composition is 70% micro-organisms. Diet influences plaque flora composition; in diets rich in carbohydrate, Streptococcus mutans predominates and is very efficient at metabolising sugars to acids. Precavitated carious lesions can be reversible by remineralisation if the plaque pH is high (alkaline). This can occur during the periods where there is no sugar intake. The concentrations of calcium, phosphate and fluoride in plaque are very important in the remineralisation process.
Once cavitation has occurred and the thin white surface layer has collapsed, it is necessary to restore the tooth surface with a restoration. Cavitated lesions are not reversible.
Epidemiology of caries
The size of the problem of caries in the population has changed over time. Prevalence and extent have fallen markedly since the late 1970s in many countries and this fall can largely be attributed to fluoridated toothpaste. However, caries is becoming more of a problem in preschool children in many countries.
Diagnosis of caries
• Visual tactile (eye plus probe).
• Radiography (usually bitewing radiographs).
• Fibre-optic transillumination.
Visual and tactile detection supported by bitewing radiographs remain the most satisfactory combination for the diagnosis of occlusal and approximal caries. ERM shows great promise and is worthy of further development. However, overall systematic and random errors in diagnosis are great.
Caries risk assessment
Each child should undergo a caries risk assessment which will assist in future planning for the child, particularly in relation to the preventive regime you offer.
An effective caries risk assessment comprises seven elements:
Prevention
The preventive regime offered will relate directly to the child’s caries risk assessment. A full preventive plan contains eight elements:
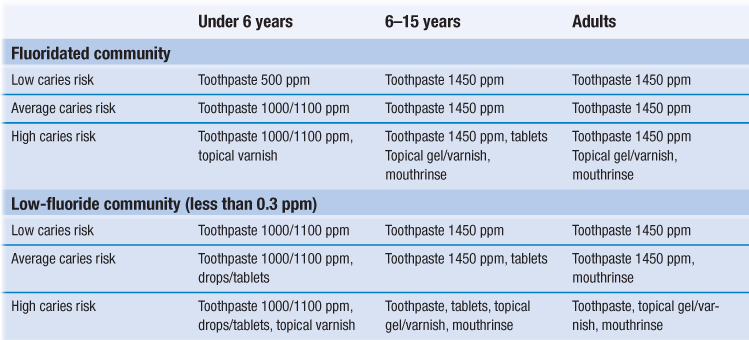
5. Supplemental fluoride: fluoride mouthrinses for age 6 years and over are a valuable daily adjunct. The 0.05% NaF (225 ppm F−) mouthrinse probably has better compliance than weekly 0.2% NaF (900 ppm NaF) application. Fluoride drops and tablets for systemic use are now increasingly difficult to source and have been largely superseded by increased toothpaste strengths and regular professional application of fluoride varnish. Although each individual method of fluoride application is effective, a combination of methods may achieve greater benefit (Table 7.4).
A 3- or 4-day diet diary is more effective than simply asking a child and parent about their diet. The diet diary, if filled out correctly, will provide information about frequency and time of day with regard to sugar intake. It is also good practice for the diary to include toothbrushing times and bedtime which will increase the accuracy of your dietary analysis. The general advice here is to restrict sugary foods and drinks to mealtimes and not to consume them within 20 minutes of bedtime. Use of a feeder cup or bottle overnight with milk or juice should be strongly discouraged. If a child wants to drink throughout the night, the only safe liquid is plain water. In general, bottle-fed babies should not require overnight milk after 4–6 months old and on-demand breastfeeding overnight should also be discouraged from this time.
1. Bulk: sorbitol, mannitol, isomalt, xylitol, lactitol and hydrogenated glucose syrup.
2. Intense: saccharin, acesulphame K, aspartame, thaumatin.
Bulk sweeteners have a laxative effect and should not be given to children under the age of 3 years.
Treatment
The treatment of carious teeth should be based on the needs of the child; the long-term objective should be to help the child to reach adulthood with an intact permanent dentition, no active caries, as few teeth restored as possible and a positive attitude toward their future dental health.
Restorative materials
Amalgam
Its main advantage is that it is economical and simple to use. However, there is current concern over its safety. In Scandinavia, its use is banned in children, with concern over environmental issues rather than amalgam toxicity itself. It does seem prudent to avoid its use whenever possible, especially in the paediatric population where other materials may give sufficient longevity.
Glass ionomer cements (GIC)
These consist of basic glass and acidic water-soluble powder; they set by an acid–base reaction between the two components. The cement bonds to enamel and dentine and releases fluoride to the surrounding tissues. This should be used as a temporary filling material only or for stabalisation of caries.
Resin-modified GIC
A hybrid of GIC/resin that retains significant acid–base reaction in its overall curing process to set in the dark. There are two setting reactions: the acid–base reaction between glass and polyacid and a light-activated, free radical polymerisation of methacrylate groups of the polymer. This material has some physical advantages over conventional GIC, together with its ability to ‘command set’. Again, this should be considered as a temporary or intermediate restorative material.
Polyacid-modified composite resin (compomer)
This contains either or both essential components of a resin-modified GIC but it is not water based and, therefore, no acid–base reaction can occur. It will not set in the dark. This technique is very sensitive to moisture contamination and should be placed under rubber dam isolation.
Composite resins
Their introduction revolutionised clinical dentistry and their aesthetic benefits especially for the anterior teeth are unquestioned. Posterior composite resins have overcome initial problems of wear resistance, water absorption and polymerisation contraction. This technique is very sensitive to moisture contamination and should be used under rubber dam isolation.
Preformed crowns
These preformed extra-coronal restorations are essential in the restoration of grossly broken down teeth, primary molars that have undergone pulp therapy, hypoplastic primary and permanent teeth and teeth in those children at high risk of caries, particularly those having treatment under general anaesthesia. The Hall technique is currently gaining favor in the treatment of high caries risk children or for those with poor co-operation for treatment. In this technique, caries is hermetically sealed inside the tooth by the preformed crown and its glass ionomer cement, and by removing dietary substrate as an energy source for bacteria, the caries underneath arrests.
Isolation
Adequate isolation is necessary for any restorative material to have a chance of success. Rubber dam isolation is the optimum and may necessitate local anaesthesia for the gingival tissues. Clamps should be secured individually with floss ligatures. Additional advantages of the rubber dam include airway protection, soft tissue protection and reduced risk of caries infection from saliva aerosol. In the absence of rubber dam, good moisture control can be achieved with cotton wool rolls, dry tips and saliva ejector. When placing a preformed metal crown without the aid of rubber dam, it is prudent to have the child in an upright position using a sponge or gauze for airway protection and a pick-up stick or other sticky device to ensure you do not drop the crown once it has been delivered to the mouth.
Primary teeth
Pit and fissure caries
The primary fissures are shallower than their permanent counterparts and the presence of caries is a sign of high caries activity. The material of choice is an adhesive material: compomer or composite. Manufacturers’ instructions for these materials should be followed assiduously utilising tooth conditioners and bonding resins where stated.
Approximal caries
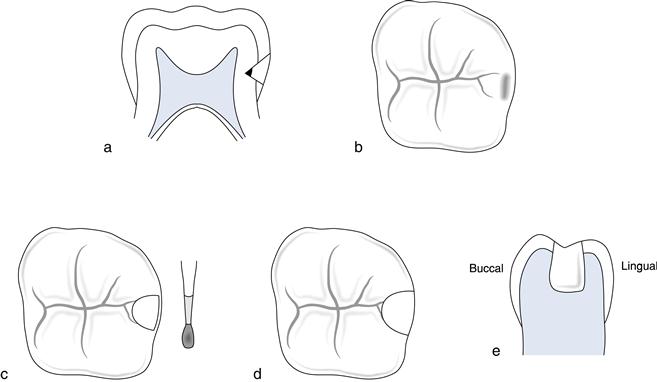
Minimal approximal cavity
A minimal approximal cavity with no occlusal dovetail is repaired using the ‘retentive box preparation’. The material of choice is a compomer or composite. The approximal box is prepared as in Box 7.1 but without an occlusal dovetail. Additional retention grooves may be achieved by placing grooves into dentine using half-round burs along the gingival floor and lingual wall. The buccal wall is avoided because of the large buccal pulp horn in primary molars (Fig. 7.1).
Approximal caries with occlusal extension
The success rate of amalgam in approximal caries with occlusal extension has been reported as being 70–80% (Box 7.1). The material of choice is amalgam or preformed metal crown where moisture control cannot be guaranteed. An alternative is to place compomer or composite where rubber dam is possible.
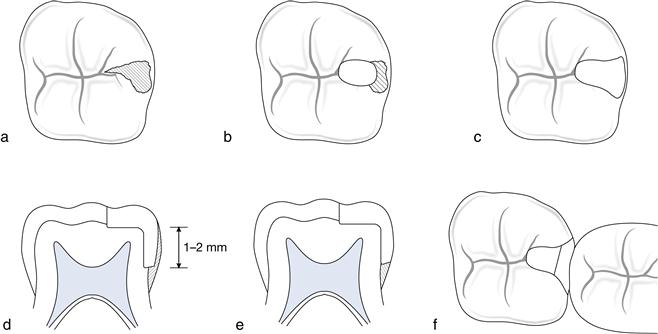
Restorations on more than two surfaces
Restorations extending onto more than two surfaces include cusp replacement and endodontically-treated teeth. The preformed metal crown is the material of choice, with survival times in excess of 40 months. Their replacement rate is low at 3% compared with 15% for amalgams. Although initially they are more expensive, in the long term they are cost-effective. There are some commercially available tooth-coloured veneer crowns but these lack the flexibility of conventional preformed metal crowns and hence require an increased loss of tooth structure. Once learnt, their conventional placement technique (Box 7.2) is less technically demanding than intracoronal restorations in primary teeth and they should certainly be considered for any tooth for which the dentist cannot be sure that an alternative restoration would survive until the tooth is exfoliated.
Anterior teeth
Treatment options for anterior teeth depend on the severity of the decay and the age and co-operation of the patient. In the preschool child, caries of the upper primary incisors is usually a result of ‘early childhood caries’: frequent or prolonged consumption of fluids containing NME sugars from a bottle or feeder cup. Progression of decay is rapid, commencing on the labial surface and quickly encircling the teeth. Early treatment could involve interproximal discing and topical fluoride therapy. For more advanced decay, the most suitable form of restoration is the ‘strip crown technique’, which uses a celluloid crown former with light-cured composite resin to restore crown morphology. In older children over 3 or 4 years of age, new lesions of primary incisors indicate high caries activity. These lesions usually occur approximally and do not progress as quickly as nursing caries. They can be restored with compomer or composite resin.
Permanent teeth
Bitewing radiographs should be taken prior to any instrumentation of a tooth surface. For a clean fissure with no radiographic evidence of caries, a fissure sealant is the treatment of choice in molar teeth. If the fissure is stained with no radiographic evidence of caries, it will require clinical exploration. If clinical exploration reveals dentinal caries, then a restoration will be required. If dentinal caries is detected radiographically, a restoration is obviously necessary.
Fissure sealants
Consideration needs to be given whether to use a clear, coloured or opaque resin sealant or whether to use a non-filled or filled resin (Box 7.3). Early sealants were clear in order to check that caries was not developing under the sealant. However, the margins were difficult to see and coloured and opaque materials were introduced in order to see areas of sealant fracture and loss. The final choice is with the individual clinician. Bitewing radiographs are an important part of sealant review as it only needs failure of one small part of the sealant–enamel bond for leakage to occur.
GIC may be useful as temporary sealants in individuals with highly active caries until teeth have erupted sufficiently to allow conventional sealants (Box 7.4). Indeed, they are similarly applicable for patients in whom isolation for placement of conventional sealants is impossible. They may require more frequent replacement because of their brittleness in thin section but they will provide occlusal protection and a reservoir of fluoride for release to surrounding enamel.
Stained fissure with no radiographic caries
The fissure should be explored with a small round bur. If the lesion stays within enamel, a fissure sealant is placed. If the lesion extends into dentine, the treatment is as for pit and fissure caries.
Pit and fissure caries
Occlusal restorations can be placed using composite or amalgam. If some fissure pattern is retained, this should be fissure sealed. A preventive resin restoration is described in Box 7.5.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses