Orthodontics III
appliances and tooth movement
Chapter Contents
Overview
Central to the success of any orthodontic treatment is selection of the appropriate appliance and competence in its handling. It is, therefore, necessary to be aware of the scope and limitations of each appliance system and the care required with its use.
In this chapter, removable, fixed, functional and headgear appliances are discussed. Histological aspects of tooth movement are then addressed and the factors that must be considered in planning retention are presented.
11.1 Removable appliances
Aside from clear vacuum-formed thermoplastic appliances that may be used in the upper and lower arches, removable appliances consisting primarily of wire and acrylic components are used almost exclusively in the upper arch. Lower appliances of the latter components are poorly tolerated because of encroachment on tongue space and the difficulty in achieving satisfactory retention due to the lingual tilt of the molars; they are, however, usually used for the sole purpose of retention post-treatment. Clear thermoplastic appliances may also be used in either arch as retainers; they are also capable of minor tooth alignment and have gained acceptance by adults for this purpose. Although functional appliances are also composed of wire and acrylic, they have a different mode of action and are dealt with in Section 11.3.
Indications for removable appliance therapy
In the contemporary management of malocclusion, the role of ‘traditional’ removable appliances composed of wire and acrylic is much more restrictive than it has been formerly; a greater awareness of their limitations and the widespread use of fixed appliances account mainly for this. Removable appliances, however, may be considered in the following situations:
• Where tilting movement of teeth is desirable and acceptable.
• To maintain space in the mixed or early permanent dentition.
• To free the buccal occlusion and facilitate crossbite correction or other tooth movement.
• To produce overbite reduction.
• As an adjunct to fixed appliance treatment.
• As a retainer following removable or fixed appliance treatment.
Designing a removable appliance
Some important points should be remembered in relation to appliance design for those that involve acrylic and wire components:
• Always design the appliance with the patient in the dental chair; this helps to avoid design errors.
• Keep the design as simple as possible: aim to carry out a few tooth movements with each appliance.
Active components
Springs
The force (F) delivered by a spring is expressed by the formula F α dr4/l3, where d is the deflection of the spring when activated, r is the radius of the wire and l is the length of the spring. Radius and wire length, therefore, have most effect on wire stiffness.
Screws
Where the teeth needed for retention of the appliance are those to be moved, a screw rather than springs may be useful. Screws, however, are more expensive than springs and make the appliance bulky. The sections of the base plate are moved apart by 0.25 mm with each quarter-turn activation.
Elastics
Intraoral elastics designed for orthodontic purposes may be used to apply elastic traction; the size and force of elastic chosen is determined by the tooth (root surface area) to be moved and the distance the elastic is stretched.
Retention component
The retention component maintains the appliance in the mouth, and it is generally advisable to have the clasps located to optimise retention. The following components are commonly used.
Adams’ clasp
Retention is achieved by the arrowheads, which engage about 1 mm of the mesial and distal undercuts on the tooth. This clasp is the most common means of gaining posterior retention. For molars, 0.7 mm wire is used, but 0.6 mm wire is advisable for premolars and primary molars. The clasp is easily modified to incorporate two teeth for retention, hooks for elastic traction or soldered tubes for extraoral anchorage. To move the arrowhead towards the tooth and to engage more gingivally, adjustment should be made in the middle of the flyover; otherwise close to the arrowhead is all that may be necessary.
Southend clasp
This 0.7 mm clasp is recommended anteriorly with the U-loop engaging the undercut between the incisors. Pushing the loop towards the base plate is the only adjustment usually required.
Long labial bow
This bow is constructed from 0.7 mm (0.8 mm if designed with reverse loops) wire and is useful in preventing buccal drifting of teeth during mesial or distal movement. Alternatively it may be fitted to the teeth as a retainer.
Adjustment depends on the design, but for a U-looped bow it is usual to squeeze the legs of the U-loop, followed by an upward adjustment anteriorly to restore its optimal vertical position.
Anchorage
Anchorage is the resistance to the force of reaction generated by the active components and is best thought of in terms of the available space for the intended tooth movement. The anchorage demands should be assessed before treatment commences and may be classified as:
• high: where all the space from an extraction is needed to align the remaining teeth or reduce an overjet; anchorage must be reinforced from the start of treatment
Patients for whom anchorage demands are high or very high are best treated by a specialist.
The anchorage demands are influenced by the following:
• Mesial drift tendency: this is greater in the upper than in the lower arch.
• Occlusal interdigitation: where this is good, mesial drift is less likely.
Intraoral reinforcement of anchorage
Anchorage may be reinforced:
Extraoral reinforcement of anchorage
Headgear may be used to pull upward and backward on a facebow attached to an upper removable, upper fixed or functional appliance, against the cranial vault. Forces of 200–250 g for 10–12 hours per day are needed. If distal molar movement is required, extraoral traction is necessary with forces of 400–500 g for 14–16 hours or more per day.
Safety with headgear
Safety is a priority because of the potential hazards to the eyes and face. Two safety mechanisms must be fitted to each headgear assembly, preferably a facebow with locking device (e.g. Ni Tom®) and a safety release spring mechanism attached to the headcap. Verbal and written instructions must be issued to the patient and parent or guardian emphasising that:
Base plate
The base plate connects the other components of the appliance and may be passive or active.
Anterior bite plane
An anterior bite plane is required when overbite reduction is necessary or when removal of an occlusal interference is required to allow tooth movement. Three essential elements must be addressed:
Posterior bite planes
Posterior bite planes are required to remove occlusal interferences and facilitate tooth movement when overbite reduction is unnecessary. This is commonly the case when correcting a unilateral buccal crossbite with mandibular displacement or an incisor crossbite. The acrylic coverage should be just sufficient to disengage the occlusion but must be adjusted to give even contact of the posterior teeth. The bite planes should be removed when the malocclusion is corrected and the appliance should then be worn as a retainer while the posterior occlusion settles.
Common tooth movements required
Table 11.1 summarises the common desired tooth movements and the active components to achieve these. Box 11.1 describes the technique involved in fitting a removable appliance.
Table 11.1
Common tooth movements and related active components
| Tooth movement required | Component and wire diameter | Activation |
| Retraction of 3 buccal | Buccal canine retractor: 0.5 mm sleeved with coil or 0.7 mm with U-loop | For 0.5 mm spring, bend anterior leg about 2–3 mm around the round beak of a spring-forming plier For 0.7 mm spring, cut 1 mm of wire from the free end, ensuring that the spring is curved into contact with the mesial surface of the canine |
| palatal | Palatal finger spring 0.5 mm | Ensure that spring is just above the gingival margin on the tooth and that movement tangential to the point of contact will keep the tooth in the line of the arch Bend in the free arm in the area between the coil and guardwire Half tooth width for single rooted teeth (3 mm) |
| Buccal movement of 4, 5 or 6 | Single tooth: T-spring, 0.5 mm Two or more teeth: screw |
Pull spring away from the base plate ~2 mm and at 45° to direction of desired movement Instruct the patient to turn screw once or twice per week |
| Palatal movement of single tooth other than 3 | Buccal retractor either 0.5 mm sleeved with coil or 0.7 mm with U-loop | As per buccal canine retractor but activation may be greater or less depending on root surface area of the tooth |
| Distal movement of upper first permanent molar (FPM) | 0.6 mm palatal finger springs to retract banded FPMs | 1–2 mm activation of springs, with headgear worn 12–16 hours per day with a force 200–250 g per side Must fit with two safety mechanisms (e.g. ‘Ni Tom®’ facebow and ‘Snap-away’ headcap) |
| Proclination of incisors | Z-spring 0.5 mm Double cantilever springs 0.6/0.7 mm Screw appliance |
Pull the spring 1–2 mm away from the base plate at ~45° angle to direction of wanted movement As for Z-spring Instruct patient to turn screw one or two turns per week |
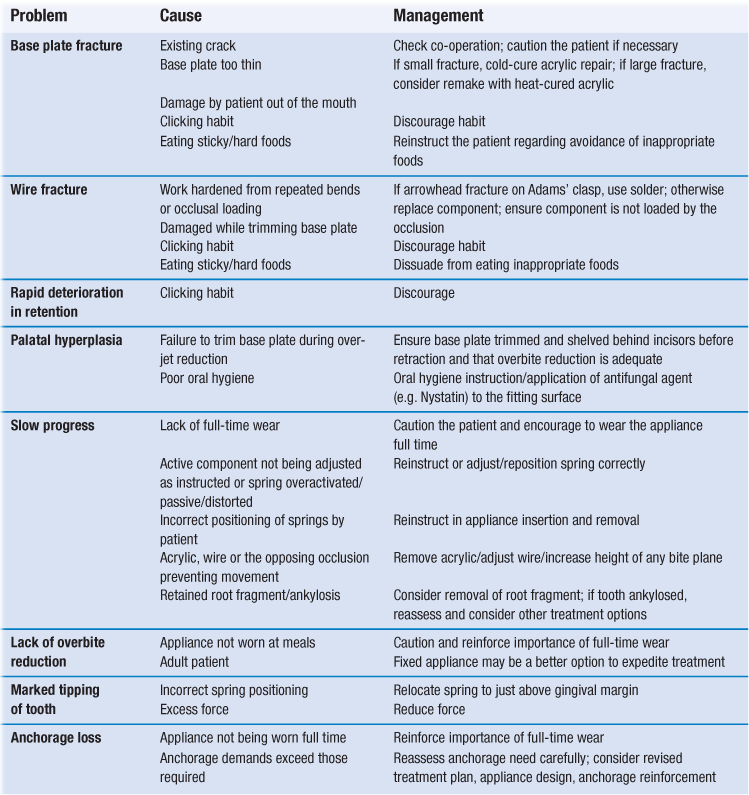
Managing problems during treatment
Problems that arise commonly during treatment are listed in Table 11.2 together with the most likely causes and necessary treatment.
Clear aligner therapy
This form of treatment involves creating a series of aligners (clear vacuum-formed thermoplastic appliances). Scanned dental casts are used to create a digital model to which small changes are then made to produce a stereolithographic cast on which the aligner is made. Subsequent incremental changes to the digital model are used to produce a matching series of altered casts for construction of a sequence of aligners. Currently, these appliances have been shown to perform well, particularly in adults, in the following circumstances: mild-to-moderate crowding in conjunction with interproximal stripping or expansion; lower incisor extraction for severe crowding; closure of mild-to-moderate spacing; posterior dental expansion; and intrusion of one or two teeth. Severely rotated canines and premolars, high canines, overbite reduction by relative intrusion and molar uprighting do not lend themselves to correction by these appliances. In conjunction with fixed attachments, however, it is possible to extend their use to closure of premolar extraction spaces, extrusion of incisors and molar translation.
These are fitted active following construction on a model to which minor tooth movement has been made. Further activation can be brought about by creating a divot in the aligner using a special plier heated to the correct temperature or by adding hard plastic bumps that snap into the aligner.
11.2 Fixed appliances
A fixed appliance is attached to the teeth.
Components
The appliance is composed of three elements: the attachments (brackets/bonded molar tubes/bands, the archwires and the accessories.
Brackets, bonded molar tubes and bands
It is becoming increasingly popular to place bonded attachments (brackets and molar tubes) on all teeth. Currently this is mostly undertaken using composite resin following acid etching of the enamel although self-etching primers (SEPs; which combine etchant and primer to avoid the need to wash the etchant away) may also be used. Resin-modified glass ionomer cements, which release and uptake fluoride in an attempt to prevent enamel demineralisation, are also available. These newer systems, however, are not as popular as the two-stage etch and prime systems due in part to reports of associated higher bond failure rates. Adhesive precoated brackets, claimed to minimise excess composite to save on clean-up time and give a more consistent bond, are also available.
The bonded brackets and molar tubes allow the teeth to be directed by the active components comprising the archwire and/or accessories. Brackets may be made from stainless steel, titanium, polycarbonate, ceramic or a combination of polycarbonate/ceramic. Molar tubes are made from stainless steel or titanium. Ceramic brackets are more aesthetic than metal but have disadvantages. They are hard and brittle so may wear the opposing teeth, increase friction with the archwire and can cause enamel fracture at debond due to the strong bond to the adhesive (common with the early-marketed types). These latter problems have now been overcome by a polycarbonate base on a ceramic-faced bracket with a metal insert in the bracket slot.
Despite the trend to use bonded tubes instead of bands on molars, bands are particularly indicated for the upper molars especially if headgear or a palatal arch is being used. Other indications include teeth with short clinical crowns, as placement of bonded attachments is difficult, and teeth with repeated bond failure. Bands are usually cemented using a glass ionomer cement. Separation of the teeth, commonly with elastomeric rings, is required for up to 1 week to facilitate band placement and guarantee best fit.
Archwires
Archwires may be round or rectangular.
With its easy formability, good stiffness and reasonable cost, stainless steel is the most popular archwire material; however, nickel–titanium, cobalt–chromium and beta-titanium – all with greater flexibility than stainless steel – have gained increasing popularity in contemporary practice. Nickel–titanium has two unique properties – shape memory and superelasticity – that relate to phase transitions between the martensitic and austenitic alloy forms. Even with a large deflection, a relatively constant low force is applied, making these archwires an excellent choice for initial alignment. They are, however, more expensive than stainless steel archwires, which because of the properties given above, are especially suitable later in treatment.
Cobalt–chromium alloy (Elgiloy) may be shaped while in a soft state and then hardened by heat treatment.
Beta-titanium has excellent strength and springiness, midway between nickel–titanium and stainless steel, making it ideal for intermediate and finishing stages of treatment.
Accessories
Elastics, elastomeric modules/chain/thread, wire ligatures
Latex elastics produced for orthodontic purposes may be used for intra- or intermaxillary traction. A range of sizes is available. Elastomeric modules are used to maintain an archwire in an edgewise bracket slot (see below) while elastomeric chain or thread may be used to move teeth along an archwire, or for derotation. Stainless steel wire ligatures continue to be used particularly when maximum contact is desired between the wire and the bracket slot or to maintain space closure.
Springs
Uprighting or rotation of teeth may be carried out by auxiliary springs, while space opening or closure may be undertaken by coil springs.
Indications for fixed appliances
Indications include:
• bodily movement of incisors to correct mild-to-moderate skeletal discrepancies
• overbite reduction by incisor intrusion
• alignment of grossly misplaced teeth, particularly those requiring extrusion
Tooth movement
As with a removable appliance, a fixed appliance may also tip teeth but has the additional possibilities of producing bodily movement (crown and root apex move in the same direction), uprighting, torquing, rotation, intrusion and extrusion of teeth.
Anchorage control
Because the palate is not covered by a base plate, anchorage control is more critical with a fixed than with a removable appliance. In addition, bodily rather than tipping movement places greater strain on anchorage.
Anchorage may be reinforced by:
• increasing the anchorage unit by bonding more teeth and ligating them together
• palatal and/or lingual arches: prevent molar tipping
• intermaxillary traction (see Section 11.1): as well as reinforcing anchorage, the incisor relationship (either increased or reverse overjet) may be corrected
• extraoral means, including reverse headgear (see Sections 10.4 and 11.1).
Appliance types
Preadjusted appliances
The preadjusted edgewise appliance uses an individual bracket with a rectangular slot for each tooth to give it ‘average’ tip, torque and buccolingual position and to allow the placement of flat archwires; some individual adjustment bends, however, are often required to the wire to compensate for these ‘average’ values. 0.018 and 0.022 systems (which describes the bracket slot width in inches) exist and bracket prescriptions by Andrews, Roth and MBT are available. Round flexible wires are used for initial alignment and rectangular wires are required for precise apical control. Clinical time is saved and good occlusal results are achieved consistently with these appliances but costs are increased due to the need for an individual attachment per tooth.
Tip-edge appliance
This uses special brackets with rectangular slots and was developed from the Begg appliance to overcome some of its deficiencies. That appliance system uses a bracket with a vertical slot and round wires exclusively held in place loosely with brass pins. Tipping movement is facilitated and auxiliaries are necessary for rotational and apical movement. With the Tip-edge appliance, although round wire is used for most of the treatment as with the Begg technique, the facility exists to place rectangular wire in the final stages, affording greater control of tooth positions.
Lingual appliance
Brackets are bonded to the lingual or palatal surfaces of the teeth and specially configured archwires are used. Recent advances include the construction, from laser scans of the study models, of customised precious metal pads to which low-profile brackets are attached, and the use of computer-controlled wire bending devices to individualise archwire fabrication.
Self-ligating appliances
These remove the need for elastomeric or stainless steel wire ligation of the archwire to the bracket. Available systems include Damon®, Speed® and Smartclip®. Because the archwire is not pressed firmly against the base of the bracket, as is the case with use of an elastomeric module or wire ligature, friction is reduced. Claims that overall treatment time is significantly shorter than with conventional preadjusted edgewise appliances have not been upheld.
Appliance management
An excellent standard of oral hygiene is essential prior to and during fixed appliance treatment. All patients must be instructed specifically in relation to diet and optimal oral hygiene practices following placement of the appliance to minimise the risk of enamel demineralisation. Mucosal ulceration is common in the early stages of treatment and it is wise to give the patient some soft ribbon wax to place over any components that are causing minor trauma. Adjustment visits are usually at intervals of 4–6 weeks. Repairing fixed appliances occupies more chair-side time than does removable appliances. Some discomfort is normal for a few days following adjustment and is usually overcome by mild analgesics.
11.3 Functional appliances
Functional appliances correct malocclusion by using, removing or modifying the forces generated by the orofacial musculature, tooth eruption and dentofacial growth.
Mechanism of action
How functional appliances work is not completely understood. They are generally devoid of active components, such as springs, and are incapable of moving teeth individually. Instead, they operate by applying or eliminating forces that are generated through the facial and masticatory musculature and by harnessing those that occur through natural growth processes. They are, therefore, only effective in growing children, preferably just prior to their pubertal growth spurt.
The specific force system set up by any appliance will depend on its particular design. Essentially, forces are developed by posturing the mandible – either downward and forward in class II or downward and backward in class III. This applies intermaxillary traction between the arches, as can be produced by elastics with fixed appliances. As the scope for posturing the mandible backward is far less than for posturing it forward, functional appliances are more successful in, and are indicated almost exclusively for, class II malocclusion. For this reason, the possible mechanisms of action will only be considered for class II malocclusion. In th/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses