9
Management of Incisor Diastemas
Prevalence of Maxillary Diastemas
The prevalence of a diastema between the maxillary central incisors of 2-mm or greater width in the U.S. population is shown in Table 9.1 (Brunelle, Bhat, and Lipton 1996). When all race groups are pooled, males had a diastema significantly more frequently than females. The prevalence of diastemas in blacks (16.2%) was significantly higher than the prevalence in whites (4.9%) and in Mexican Americans (6.6%), who had statistically similar frequencies of occurrence. Eight- to 11-year-old children in all groups had a higher prevalence of maxillary diastemas than did 12- to 17-year-old adolescents and 18- to 50-year-old adults, primarily because the younger subjects did not have a full complement of erupted permanent teeth.
Table 9.1. Prevalence of Maxillary Diastema ≥2 mm by Age, Gender, and Race in Americans 1988–1991
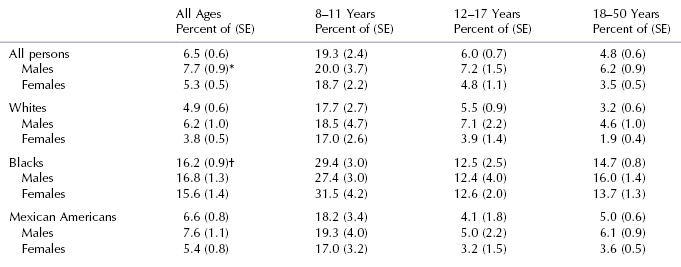
*Males are different from females, p < 0.01.
†Blacks are different from whites and Mexican Americans, p < 0.001.
From Brunelle, Bhat, and Lipton (1996).
Etiologic Factors to Consider
Many opinions about the cause and relapse of the median diastema between the upper central incisors have appeared in the periodical literature (Shashua and Årtun 1999). A follow-up study of 97 consecutively treated patients 4 to 9 years after orthodontic correction gives reliable evidence about the diagnosis and treatment of median distemas (Shashua and Årtun 1999). The relapse incidence was 49%. Logistic regression analysis showed only two significant associations between pretreatment factors and high risk for relapse: (1) diastemas wider than 2 mm and (2) having a family member with a similar diastema. Pretreatment spacing of the upper anterior teeth approached significance. At follow-up, fremitus (mobility of a maxillary incisor when sensed by a forefinger placed on the labial surface while the patient clenched his teeth) was the only parameter at follow-up that was significantly associated with the reopening of space. The following factors were not significantly associated with relapse of diastema closure: (1) abnormal frenum, (2) midline interosseous cleft, and (3) deep overbite. The authors stated that a frenectomy should not be performed to enhance the stability of treatment closing a diastema (Shashua and Årtun 1999). In a longitudinal study of a group of 9-year-old subjects with abnormal frenum, no difference was found in spontaneous closure of the diastema between subgroups that had and did not have a frenectomy (Bergström, Jensen, and Mortensson 1973).
When taking pretreatment records, it is important to ask whether another family member has a diastema similar to the patient. Familial associations indicate that an important genetic component is involved in the development of a median diastema (Shashua and Årtun 1999). In these patients, long-term retention should be mentioned before starting the treatment.
From these findings, clinicians must be prepared to retain indefinitely the closure of large median diastemas. Another approach is to use aesthetic dentistry to enlarge the widths of upper anterior teeth that are smaller than normal. Long-term retention must be the goal for adolescent and adult patients. Children in the mixed dentition who have diastema issues cannot be fully treated until all the upper teeth mesial to the first molars are erupted.
Size of Teeth and Bolton Analysis
On the basis of these findings, the size and spacing of upper incisors should be evaluated when planning treatment. Does the Bolton anterior analysis predict a mandibular excess? If so, closure of the upper diastema should be accompanied with esthetic dentistry to enlarge the upper incisors to correct the Bolton discrepancy. Does the lower arch have spaces that, in effect, create a Bolton mandibular excess? If so, the lower arch spaces must be closed along with the upper anterior diastema. If the lower spaces are not closed, aesthetic dentistry must unduly enlarge the mesiodistal size of the upper anterior teeth to achieve appropriate overbite and overjet.
Upper central incisors are usually stable with regard to size and shape, whereas the upper lateral incisors are prone to greater variation in size and shape (Dahlberg 1953). In most patients whose tooth size plays a role, the upper lateral incisors are too small. All four of the upper incisors may be too small in some patients with a diastema problem. Measurements can be taken of the mesiodistal widths of the incisors to determine the role of tooth size in the diastema problem of a particular patient. The widths of the anterior teeth in American whites with normal occlusion are given in Table 9.2.
Table 9.2. Mesiodistal Widths of Anterior Teeth in White Americans with Normal Occlusion (mm)
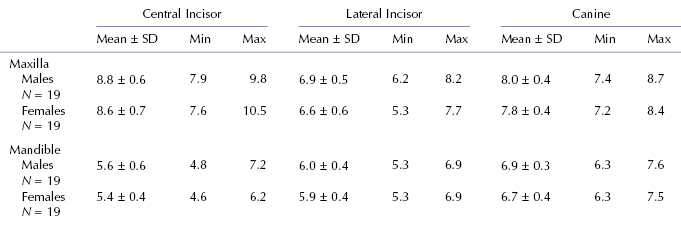
From R. N. Staley, T. L. Juhlin, and C. Kummet, 2009, unpublished data.
When a small Bolton mandibular excess occurs in a Class I patient with normal-sized upper incisors and small spaces between them, the upper spaces could be reduced in size by removal of some interproximal enamel from several lower teeth, such as premolars and canines, accompanied by retraction of the lower teeth (Bolton 1958). This treatment requires a full arch fixed appliance in the lower arch. Removal of enamel from lower teeth is best limited to a small amount, such as 1 or 2 mm for the entire arch. The space created by enamel removal in the lower arch must be closed before upper arch spaces can be closed or reduced in size.
Some patients with a small median diastema between the two upper central incisors associated with well-aligned upper and lower arches can be treated with composite resin build-ups without orthodontic treatment. This treatment is excellent from the viewpoint of tooth stability following closure of the diastema. Whenever orthodontic appliances move teeth, the potential for postorthodontic tooth movement must be recognized and controlled with a retainer.
Arch Size
If arch size is suspected as an etiologic factor, measuring the widths of the patient’s arches and comparing them with those in males and females who have normal occlusion will reveal the presence of this factor. Arch width norms for American whites are given in Figure 3.5, Chapter 3.
Patients who have large upper and lower arches associated with generalized spaces may have a large tongue or generalized small teeth, which are etiologic factors associated with some diastemas. Referral to a specialist is the best management decision for these patients.
Maxillary Labial Frenum
A median diastema between the upper central incisors may be associated with an abnormal maxillary labial frenum. Characteristics to be observed include (1) the frenum attaches into the soft tissues between the incisors or even into the palatal tissues lingual to the incisors, (2) the frenum that attaches to the soft tissues between the incisors is wider than normal, and (3) the soft tissues between the central incisors move and are blanched when the upper lip is pulled to stretch the frenum.
A frenectomy, the surgical removal and re-positioning of a frenum, is not recommended based on the evidence given earlier. A 20-year-old female patient with an abnormal maxillary frenum is shown in Figure 9.1. A periapical radiograph of the central incisors shows a midline interosseous cleft (Fig. 9.2). This 20-year-old patient had a frenectomy after closure of the diastema (Fig. 9.3). One potential negative outcome of a frenectomy is the development of an open gingival embrasure, or black triangle, as observed in this patient (Fig. 9.3) (Kurth and Kokich 2001).
Figure 9.1. Patient with an abnormal maxillary frenum.

Figure 9.2. Periapical radiograph of the patient with an abnormal frenum.
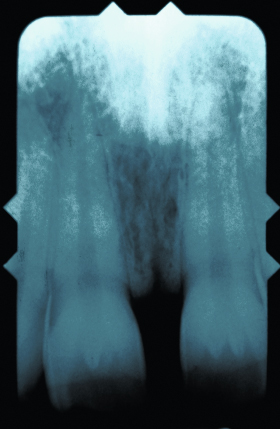
Figure 9.3. Patient’s teeth after a frenectomy was performed.

Rotated Incisors
When an incisor is severely rotated, a diastema may appear. Rotation of the tooth to its proper position with a fixed edgewise appliance will reduce or eliminate the diastema problem. Retention of the tooth after treatment to prevent relapse of the rotation is very important. Supracrestal fiberotomy and bonded fixed retainers are used to reduce relapse and retain rotated teeth (Edwards 1988).
Thumb-Sucking Habit
Patients who have a thumb-sucking habit may present with diastemas between the upper incisors. If the patient has a Class I occlusion, interceptive limited treatment involves first stopping the habit and then retracting the incisors. After the habit is stopped, the upper incisors usually return to a more normal position without active orthodontic treatment. Limited orthodontic treatment may be needed to properly position the teeth after the habit has ceased. The use of an appliance in conjunction with psychological support of the patient by the clinician has been shown to be an effective means to help a young patient break the habit (Bourne 2005; Haryett, Hansen, and Davidson 1970).
Angle Classification
Patients with Class I molar and canine occlusion are the most appropriate candidates for limited orthodontic treatment. Patients with Class II and Class III occlusions are best managed by referral to a specialist.
Management with Appliances
Removable appliances are useful when one or two teeth need to be moved, when the diastema is no larger than 2 mm, and when tipping movements from the appliance will not adversely affect the angulation of the tooth. Finger springs originating in the palatal or lingual acrylic are used when diastemas are small and the teeth are located on the crest of the alveolus. Loop springs, also known as arc springs, can be soldered on the labial bow of a Hawley appliance to close a diastema. The spring on a removable appliance should push against the tooth crown at the level of the gingiva to ensure the most favorable movement of the tooth. The anterior palatal acrylic of the removable appliance is given a parabolic shape to guide the tooth or teeth being moved and keep them in the central part of the alveolar ridge. The labial bow on a Hawley appliance can be used to retract all four of the incisors.
When more than one or two teeth must be moved, when rotated teeth must be corrected, and when centering a tooth in a space is required, a fixed edgewise appliance best accomplishes the treatment goals.
Treatment of a Diastema with a Removable Loop Spring Appliance
A 17-year-old patient with a Class I occlusion had a diastema between her maxillary central incisors (Figs. 9.4 to 9.7). In Figure 9.4, the removable appliance to correct the diastema contained two loop springs soldered to the labial bow of a Hawley />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


