Implant Restoration of the Partially Edentulous Patient
Steven J. Sadowsky
University of the Pacific Arthur A. Dugoni School of Dentistry, San Francisco, California, USA
When the osseointegration concept was introduced to North America in 1982, it prompted a tectonic shift in how the completely edentulous patient could be restored to improve the quality of life of patients. No longer were compromised patients relegated to either highly invasive preprosthetic surgical procedures or tethered to a steady application of denture adhesive to function adequately. On the other hand, implant‐supported restorations for the partially edentulous patient were slower to evolve and treatment designs were mired in broadly accepted tenets applicable to the natural tooth instead of an ankylosed root analog. Why else has there been such inertia to accept tilted implants, 2:1 crown‐to‐implant ratios, posterior cantilever fixed dental prostheses, short implants, nonsplinted posterior multiple units, and occlusal schemes that do not demand the absence of nonaxial contacts? Mark Twain said, “It’s not what you don’t know that gets you in trouble. It’s what you know for sure that just ain’t so.” This chapter will address differential treatment planning decision‐making criteria relevant to implant‐borne prostheses for the partially edentulous patient.
An algorithm helpful to evaluate patient’s candidacy and design preference in implant restorative treatment is a pyramid of diagnostic considerations (Figure 9.1). At the base of the pyramid is the best available evidence to establish prognosis. Chapter 1 offers the reader a map to navigate the literature in order to identify externally and internally valid studies. The second block is systemic factors. Chapter 2 delineates the absolute and relative contraindications to implant placement. The third block is local factors. These include four “F”s: field (spatial allowance), foundation (quantity/quality of bone, soft tissue biotype/morphology), facial esthetics (high/low lip line, lip support), and forces (parafunction, occlusal loading). The fourth block is patient‐mediated factors. These also include 4 “F”s: financial considerations, forecast of treatment time, fixed splint vs. individual units, and fear of morbidity of treatment. Once the patient has been established as a candidate for dental implants, local and patient‐mediated factors often dictate treatment decisions.
Figure 9.1 Pyramid of success when considering critical factors in diagnosis and treatment planning of implant prostheses.
Local factors influencing implant therapy
The occlusocervical height of the residual alveolar ridge should be sufficient to accommodate a 7 mm long implant as documented in long‐term studies, unless augmentation is planned.1–3 In addition, the three‐dimensional position of the implant has been shown to impact the bony and soft tissue contours which plays a prominent role in restorative success, especially in the esthetic zone.4 There should be at least 2 mm of bone buccal to the implant on placement and approximately 1.5 mm proximal to the adjacent tooth, so a 4 mm diameter implant would require 7 mm interproximally (Figure 9.2).4 The coronal–apical position of the implant should be approximately 2–3 mm apical to the mid‐buccal cementoenamel junction of the adjacent teeth (Figure 9.3).5 Crestal bone height discrepancies may be rectified before tooth extraction with orthodontic forced eruption. In the maxillary anterior sextant, a cement‐retained crown may be designed because of the trajectory of bone and will require 1 mm of interarch space between the abutment and the antagonist tooth. On the other hand, if screw‐retained crowns can be designed in this region, they will require at least 2 mm clearance between the implant platform and the opposing tooth in order to house the screw access in the cingulum area. This may be problematic in class II, division 2 jaw relations or patients with significant vertical overlap and minimal horizontal overlap (Figure 9.4a). When there is inadequate interarch space even for cement‐retained implant prostheses, orthodontic intrusion is recommended (Figure 9.4b, c). In the posterior quadrants, a minimum of 5 mm of interocclusal space is required for screw‐retained designs (Figure 9.5a, b) and 7 mm for cement‐retained restorations (Figure 9.5c, d). With less than 5 mm of axial wall height for the abutment (Figure 9.5e), retention of the restoration is challenged. When any these aforementioned parameters cannot be achieved (Figure 9.6a), interceptive orthodontics (Figure 9.6b, c) has been instituted for space management and/or optimization of the occlusal plane in order to both retain and maintain the restoration in harmony with excursions. Inadequate horizontal dimension of the bone has been addressed with guided bone regeneration, onlay/veneer grafting, ridge splitting, and ridge‐preservation procedures.
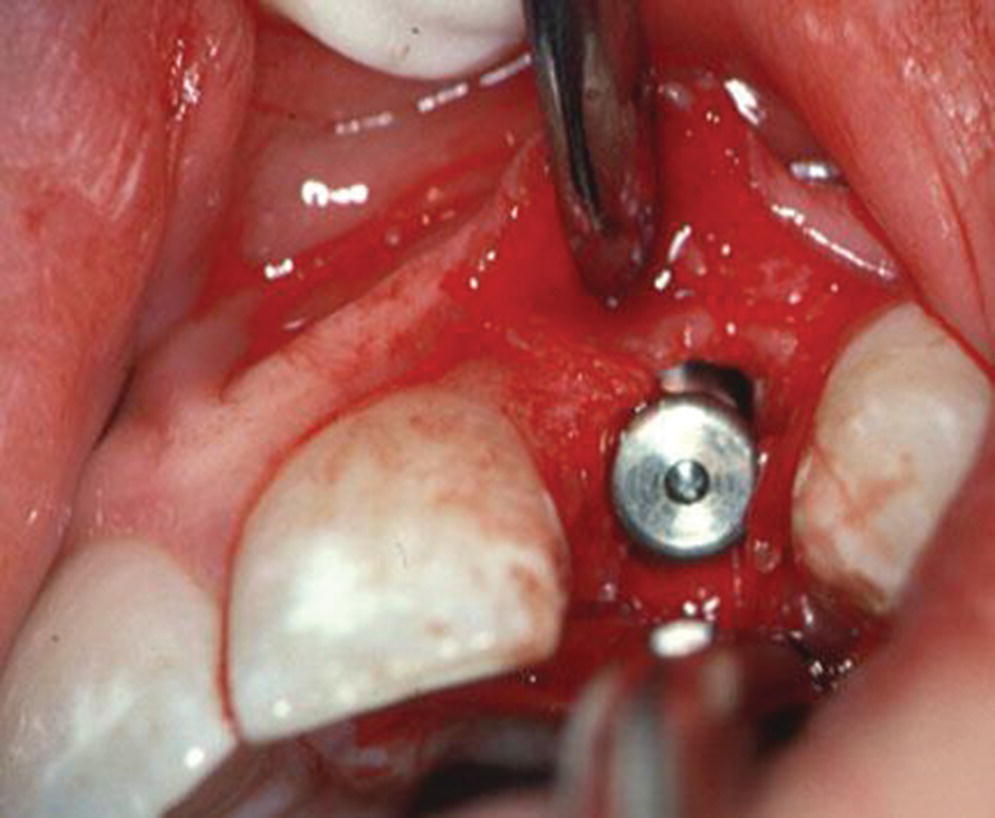
Figure 9.2 Placement of implant in horizontal plane with ≥2 mm bone facial to fixture.
Source: Reproduced with permission from Charles Goodacre.
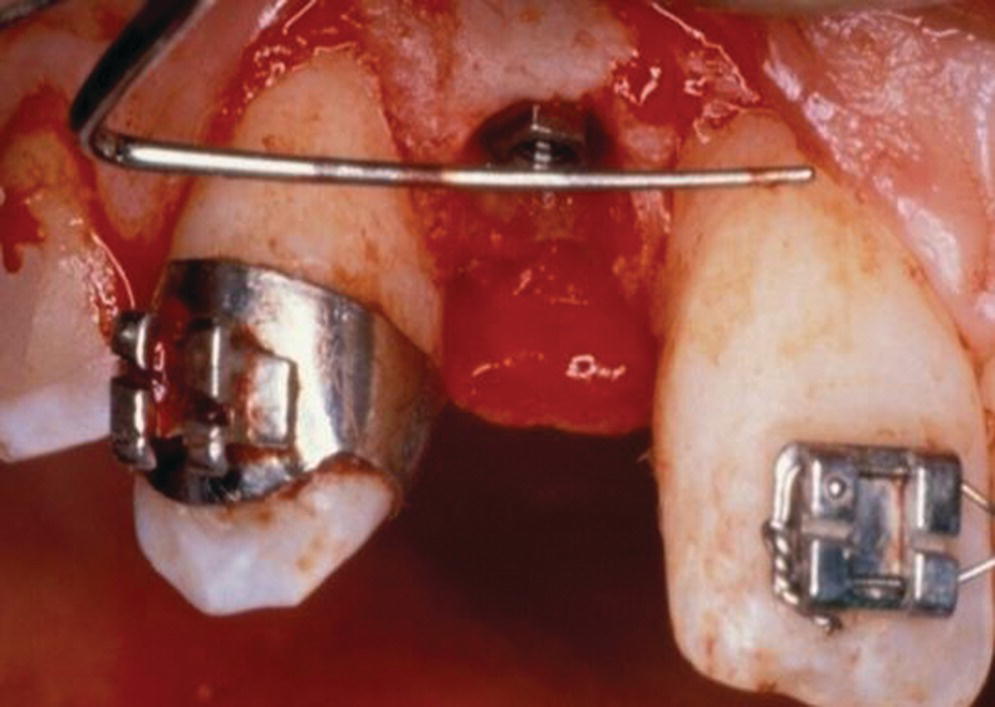
Figure 9.3 Placement of implant in frontal plane 2–3 mm apical to the adjacent teeth cementoenamel junction.
Source: Reproduced with permission from Charles Goodacre.

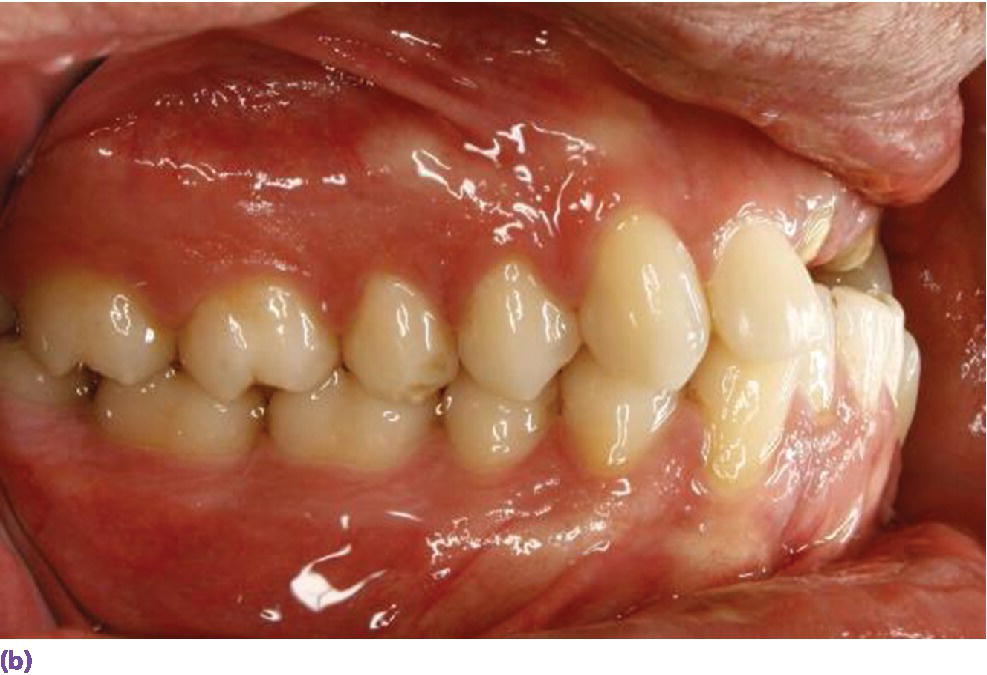

Figure 9.4 (a) Class II, division 2 jaw relation pre‐empting replacement of decoronated roots with a screw‐retained implant fixed dental prosthesis due to the lack of sufficient space for the screw‐access housing. (b) Supraeruption of mandibular incisors encroaching on restorative space for implant prosthesis. (c) Orthodontic intrusion of mandibular incisors to accommodate maxillary anterior restorative requirements and harmonious crown morphologies.





Figure 9.5 (a, b) Minimum of 5 mm interocclusal space is required for screw‐retained restorations. (c) A minimum of 7 mm of interocclusal space is required for a cement‐retained crown allowing at least 5 mm for abutment height. (d) Canine guidance or group function developed when restoring a posterior implant crown. (e) Implant not placed orthogonally with occlusal plane obviating the use of screw‐retained design. However, restricted interarch space has compromised retention of a cement‐retained prosthesis. Auxiliary retention using a lateral screw would be appropriate.
Source for (a–d): Reproduced with permission from Carlos Eduardo Gonzales Espinoza.
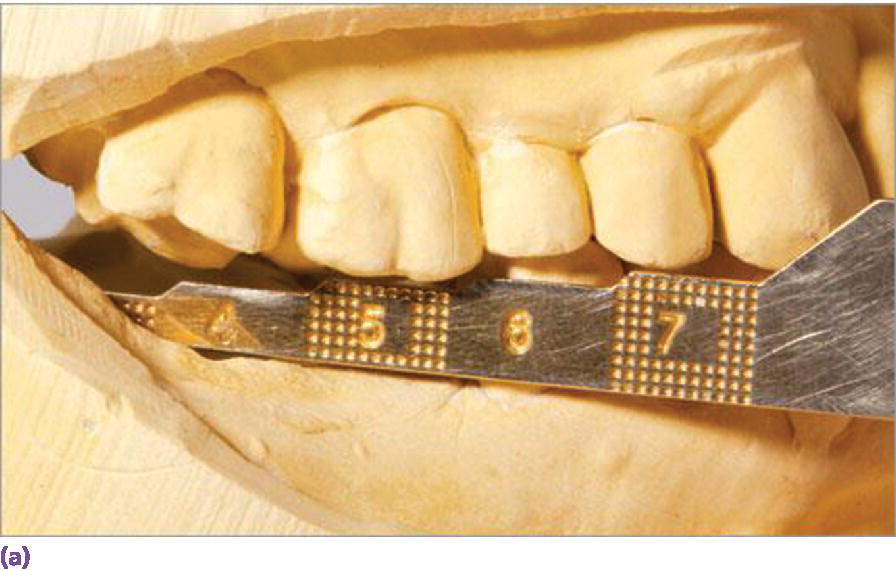


Figure 9.6 (a) Measurement of vertical space to assess interarch accommodation for screw‐ or cement‐retained restorations. Despite the 5 mm allowance for a screw‐retained restoration in this scenario, equilibration or restoration of antagonist teeth would be necessary to eliminate excursive interferences. (b) Supraeruption of maxillary second bicuspid and first molar influencing design of antagonist crown height and occlusal scheme in lateral excursions. (c) Use of buccal and palatal temporary anchorage devices (TADs) for intrusion with expected movement of 0.5–1 mm per month for adults.
Differences in gingival and osseous architecture have been documented widely and have been shown to exhibit a significant influence on restorative outcomes.6,7 Thin gingival biotypes are highly sensitive to trauma and inflammation and have been reported to be associated with three times the marginal recession of thick biotypes after extraction (Figure 9.7).8 The loss can be 1.5–2 mm over the first year, with the most loss occurring in the initial 3 months (Figure 9.8).9 Ridge preservation should be considered for most thin biotypes.10 On the other hand, if immediate placement of implants in thin biotypes is pursued, there may be insufficient thickness in periodontal tissues to minimize alveolar resorption or lack of anchoring bone to ensure predictable stabilization.10 The presence of a papilla between immediate single‐tooth implants and adjacent teeth was significantly correlated with a thick flat biotype.11,12 In fact, a 5‐year prospective clinical study reported that the failure‐free rate was 94% and 78% for maxillary central incisor metal–ceramic crowns with thick and thin biotype, respectively.10 The main cause of failure was an esthetic problem.13 In an effort to improve the esthetic outcome with thin gingival biotypes, subepithelial connective tissue grafting and specific implant and restorative planning have been recommended (Figure 9.9a–g). A change to a more palatal and apical implant placement with a straight‐walled platform, 3–4 mm inter‐implant space, use of concave abutment and crown profile, as well as platform switching may lead to greater success.14,15 Two meta‐analyses assessed the impact of platform switching on peri‐implant bone changes, which revealed significantly less mean marginal bone loss (approximately 0.5 mm) at implants with a platform‐switched compared to platform‐matched implant–abutment configuration (Figure 9.10).16,17 However, because of heterogeneity of the included studies, the results should be interpreted with caution.


Figure 9.7 (a) Thick gingival biotype, square tooth morphology, wide band of attached tissue, short papillae. (b) Thin gingival biotype, trigonal tooth morphology, narrow band of attached tissue, long papillae.
Source: Reproduced with permission from Charles Goodacre.

Figure 9.8 Extraction of central incisor on thin biotype without ridge‐preservation procedure.






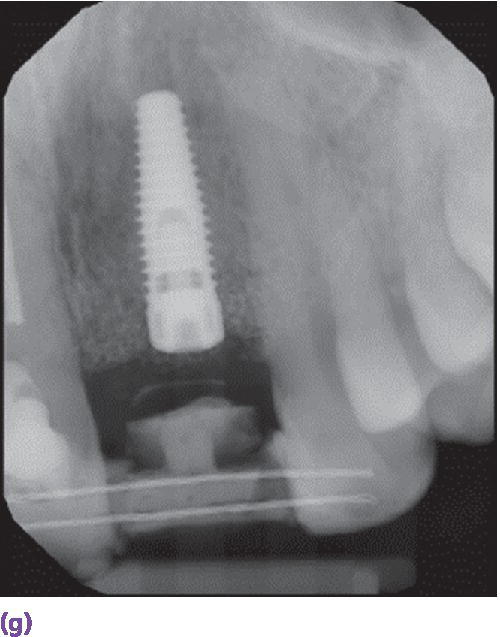

Figure 9.9 (a) Maxillary left central incisor is unrestorable. (b) Periapical radiograph disclosing internal and external resorption. (c) Subepithelial connective tissue graft in conjunction with implant placement. (d) Palatal donor site for graft. (e) Resin‐bonded bridge (facial view). (f) Resin‐bonded bridge reinforced with orthodontic braided wire (palatal view). (g) Periapical radiograph of implant while integrating. (h) Patient with full smile with restoration in place.

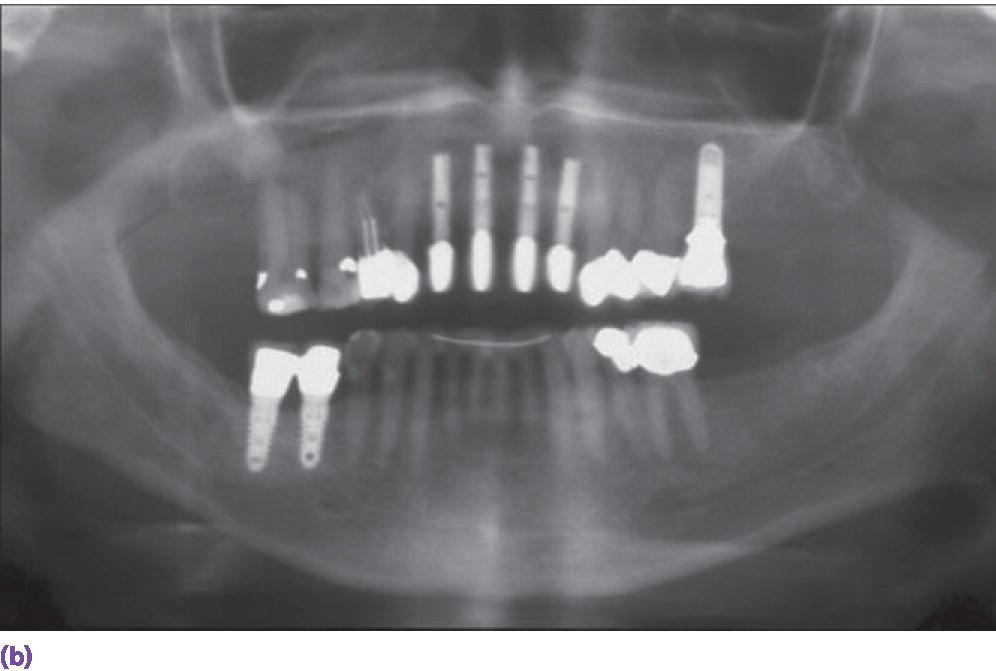
Figure 9.10 (a) Individual porcelain fused to metal crowns on sites #7, 8, 9, 10 implants. (b) Platform‐switched abutment design.
The presence of chronic periodontitis has been implicated in higher incidence of implant marginal bone loss and late failure, especially in cases of aggressive periodontitis without periodontal maintenance.18,19 When patients with a history of periodontitis are well controlled, no link has been shown between their history and implant failure.20 However, when a patient has had a previous implant failure, the risk of another failure increases by an odds ratio of 1.3.21
Finally, all adjunctive interceptive procedures involve additional risk factors that are patient, operator, and technique sensitive. A comprehensive treatment plan optimally weighs the risk, benefit, and cost of each treatment option.
Indications for endodontic versus implant therapy
The decision to endodontically treat or retreat a tooth or extract and place an implant has been addressed in a number of systematic reviews.22–24 Although similar high survival rates have been reported, the implant group has demonstrated almost fivefold higher incidence of postoperative complications.25 However, the survival data vary with specific local factors which affect the prognosis of endodontic treatment. For example, Salehabi and Rotstein26 assessed more than 1.4 million patients during an 8‐year period and found, in the absence of apical periodontitis, the probability that initial endodontic treatment would keep the tooth disease‐free was 92–98%, but the chance that a tooth with apical periodontitis would completely heal after initial treatment was 74–86% (Figure 9.11). Odds of success of treatment were found to decrease by 14% for every 1 mm increase in the diameter of the preoperative lesion.27 Tortuous root anatomy, and presence of calcifications or internal/external resorption also compromise prognosis, but with the aid of cone‐beam computed tomography (CBCT), treatment results have improved (Figure 9.12).28 Regarding orthograde retreatment, success was reduced if there was an alteration of the root canal morphology (47% as opposed to 86.8%, 2‐year follow‐up), presence of apical radiolucency, and adequate previous endodontic therapy (higher likelihood of extraradicular lesions, cystic lesions, and foreign body reactions).29 For surgical retreatment, success reports vary widely (59–93%).28,30,31 The following factors were identified as predictors of healing: absence of preoperative pain or signs, good density of the root canal filling, and a periapical lesion size of 5 mm or less. With regard to treatment‐related factors, teeth treated with the use of an endoscope tended to have higher healed rates than teeth treated without the use of an endoscope.32

Figure 9.11 Approximately 10% reduced chance of complete healing after primary endodontic treatment for #8 compared to #9 because of apical radiolucency.

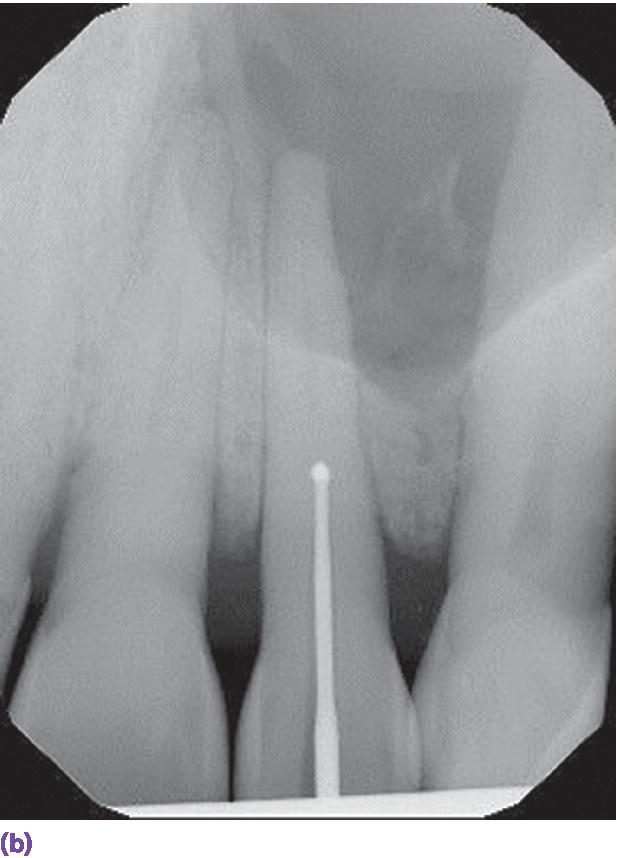

Figure 9.12 (a) Accuitomo scan of calcified canal of #10. (b) Gates‐Glidden drill (Dentsply Tulsa Dental Specialties, Tulsa OK) accessing calcified blockage. (c) Completed obturation of #10.
Source: Reproduced with permission from Ray Scott.
When deciding on endodontic treatment or replacement with an implant, the prosthetic restorability, periodontal support, caries index, strategic importance of the tooth, esthetic demands, cost/benefit/risk analysis, operator expertise, and patient preferences will weigh heavily. For example, the remaining coronal structure should allow for a 1.5–2 mm ferrule with at least 1 mm of dentinal thickness, otherwise forced eruption or crown lengthening (barring gingival scallop disharmony) is needed. 33
An elongated epithelial attachment, which can be disclosed through sounding the midfacial bone, often does not create an esthetic blemish in the gingival contour. However, if the tooth is extracted without the preparation of orthodontic forced eruption, a soft/hard tissue dehiscence is likely. Therefore, this scenario would place a high premium on salvaging the natural tooth through endodontic (re)treatment.
The periodontal status of teeth considered for preservation has been stratified. Treatment of molars with class I furcation invasion with nonsurgical periodontal therapy was more cost effective than treatment with implant‐supported crowns.34 Samet et al.35 have identified teeth with 6–8 mm pocket depth, 50% attachment loss, or class II furcation as questionable for retention. In a long‐term study of up to 27 years with a mean of 11.5 years of follow‐up, lack of compliance, smoking, and residual 6 mm post‐periodontal treatment pocketing were risk factors for progression of tooth loss.36 However, it is important to keep in mind when adequate periodontal treatment and maintenance are performed, a 10‐year study tracking natural teeth with chronic or aggressive periodontitis (with an initial 50–70% attachment level) reported 88% survival of teeth.37 As a consequence, the decision of tooth extraction, for periodontal reasons in favor of a dental implant, should be carefully considered in partially edentulous patients.
The use of adenosine triphosphate‐driven bioluminescence has been demonstrated to be an effective innovative tool in enumerating the total bacteria count and oral Streptococcus mutans.38 This enables the practitioner to assess a baseline reading and patient’s commitment to oral hygiene to forecast long‐term restorability of natural teeth. There may be a premium on endodontically (re)treating a tooth adjacent to an implant to preserve the interproximal bone (Figure 9.13), or an abutment which is part of a long‐span fixed dental prosthesis. Additionally, esthetic demands may predicate salvaging a natural tooth. In these strategic scenarios, the patient should be apprised of the advantages of preservation and the importance of home‐care maintenance for success.
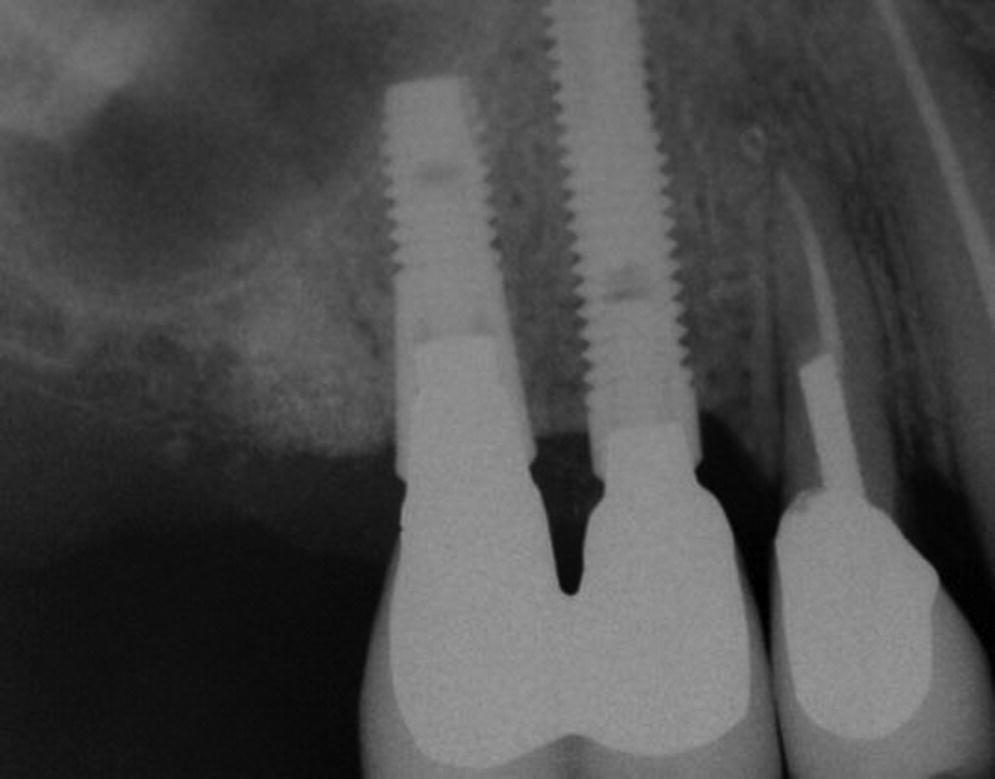
Figure 9.13 Interproximal bone preserved with natural tooth (#5) proximal to implant restoration, placing premium on retreatment of this tooth.
Source: Reproduced with permission from Charles Goodacre.
When generalists perform endodontic therapy or implant surgery, there is a lower survival rate reported compared to specialists, with a greater discrepancy in implant outcomes.39–41 Specifically, survival of implants placed by inexperienced clinicians was 73.0% as opposed to 95.5% by implant specialists.42 A comparison of tooth survival rates after endodontic treatment by endodontic specialists vs. general practitioners, in a multicenter study consisting of 350 teeth that met the inclusion criteria, showed a difference of 98.1% vs. 89.7%.43 Informed consents should include operator experience,44 maintenance projections, esthetic and functional expectations, treatment cost/time comparisons, and impact of no treatment. An average treatment time estimate of an implant restoration on the maxillary arch is up to 250 days vs. 67 days for endodontic therapy.
In summary, when orthograde or surgical endodontic retreatment is indicated, the advent of dental operating microscopes, newer ultrasonic armamentaria, nickel–titanium rotary instrumentation, advanced electronic apex locators, thermoplastic gutta‐percha delivery, mineral trioxide aggregate, and CBCT diagnostic tools have made this strategy the second line of defense before extraction and implant replacement.45–48
Indications for tooth‐supported fixed dental prostheses versus single implant crowns
When comparing 10‐year survival rates (approximately 89%) of tooth‐supported fixed dental prostheses (FDPs) (Figure 9.14) and single implant crowns (SICs) (Figure 9.15), virtually no differences have been reported when metal–ceramic restorations were evaluated.49 When the same investigators compared 5‐year complication rates, conventional FDPs represented more biologic sequelae, such as loss of vitality, caries, and recurrent periodontitis, while SIC recorded more technical problems, such as loose abutment screws, veneer fracture, and loss of retention.

Figure 9.14 Three‐unit fixed dental prosthesis replacing #8.
Source: Reproduced with permission from Nicola Zitzmann, Basel, Switzerland.


Figure 9.15 (a) Healing abutment in #8 site. (b) Single implant crown replacing #8.
Source: Reproduced with permission from Charles Goodacre.
Despite high survival rates of metal–ceramic restorations, there has been a growing emphasis on evolving all‐ceramic systems, driven by the debatable need for metal‐free restorations. It is of note that 5‐year follow‐up studies have demonstrated lower survival rates of glass ceramic FDPs (e.g. lithium disilicate system), glass‐infiltrated alumina FDPs (e.g. In‐Ceram system), and densely sintered zirconia FDPs in comparison with metal–ceramic restorations.50 The incidence of framework fractures was significantly higher for reinforced glass ceramic and infiltrated glass ceramic FDPs, while the incidence for loss of retention and ceramic fractures was significantly higher for densely sintered zirconia FDPs compared to metal–ceramic FDPs. On the other hand, the performance of all‐ceramic implant restorations supported by zirconium abutments versus metal–ceramic crowns on titanium abutments demonstrated no biologic or technical differences in complications with a 5‐year follow‐up (Figure 9.16).51 One caveat in assessing the data on single implant crowns is that esthetic problems may be under‐reported in as many as 60% of studies.52,53 However, Zitzmann et al. focused in on the cost effectiveness of a three‐unit tooth‐borne FDP compared with a SIC in the anterior sextant. Their investigation revealed fewer complications and higher patient satisfaction for the implant restoration.54 In addition, Walton,55 in a 15‐year study on over 300 patients, compared these two modalities and reported the estimated cumulative survival for SICs was significantly better than for three‐unit FDPs when replacing anterior teeth. The complication rates of the FDPs and SICs were similar, but the economic burden for the FDPs was greater.



Figure 9.16 (a) Zirconia abutment affixed to implant in #8 site. (b) All‐ceramic crown restoring #8. (c) Periapical radiograph.
Source: Reproduced with permission from Carlos Eduardo Gonzales Espinoza.
Given the aforementioned data, the optimal restorative design will be predicated on systemic,56,57 local,58 and patient‐mediated factors.59 Local factors to consider include caries index, periodontal condition of the teeth, the restorability or need for restoration of teeth bounding the edentulous span, the quality/quantity of bone of the prospective implant site, the indication for interdisciplinary care required to optimize the implant site, as well as the esthetic predictability of the conventional/implant regimens.60,61 Patient‐related factors include desire for either individual units or/and maintaining unrestored teeth, morbidity concerns especially with additional adjunctive care, and projected treatment time/cost differences. Single tooth implants have been projected to be financially commensurate with three‐unit fixed dental prostheses, but 75–90% more costly than a similarly endodontically treated tooth, and require up to four times the number of days for treatment.62
Indications for implant‐fixed dental prostheses and cantilevered fixed dental prostheses
When comparing studies before and after the year 2000, there has been a positive learning curve in the survival rate of not only single implant crowns but also multiple‐unit implant‐supported fixed dental prostheses (IFDPs).63 The 5‐year survival rate of IFDPs (Figure 9.17) has increased from 93.5% to 96.4%, but the incidence of complications is still high. For example, biologic problems, reported as peri‐implant disease, soft tissue complications, marginal bone loss, fistula, or gingivitis, have slightly increased from 7.4% to 9.4% in newer studies.63,64 These results may be in part due to better reporting. However, esthetic outcomes have improved in more recent investigations. The advent of wider application of zirconia‐based ceramics and appreciation of biologic principles integral to a healthy and harmonious result appear to be responsible.65–67 On the other hand, when assessing technical problems, IFDPs have about twice the incidence of veneer fracture (7.7%) than SICs in more recent studies. The risk of fracture of veneering material has been shown to increase with the size of the reconstruction, in addition to veneering ceramics for zirconia‐based IFDP frameworks exhibiting higher chipping.63 However, the use of slow cooling, more anatomically designed zirconia copings, sufficient thickness of veneer porcelain and minimum connector height of 3 mm may rectify this higher incidence of fracture. Occlusal guidelines have attempted to address the absence of proprioception recorded in implant‐ versus tooth‐supported restorations by recommending light centric contacts and either the absence of or shared excursive contacts, although this is strictly empirical.68 Abutment or screw loosening (4.0%) has been observed less in IFDPs than in SICs,69 and has also shown a reduction of incidence in later investigations, perhaps due to the increasing use of internal connection implants70 and the adoption of proper preload. It has been demonstrated in vitro that tightening the screw a second time within 10 seconds of initial recommended torque level has overcome 40% of the preload loss due to torsional relaxation of the screw shaft, embedment relaxation, and plastic deformation.71,72


Figure 9.17 (a) Titanium abutments to support a fixed dental prosthesis. (b) Porcelain‐fused‐to‐metal implant fixed dental prosthesis.
Controversy has persisted regarding the decision to place one implant per crown instead of planning for an IFDP. Yi et al.73 conducted a comparative retrospective study on three‐unit IFDPs supported by two or three implants in posterior maxillary or mandibular partially edentulous patients (Figure 9.18). Results revealed 100% implant survival and no significant differences in complications with 63 patients observed with up to a 5‐year follow‐up. Salvi and Bragger74 corroborated the absence of a link between complications and number of implants supporting the prosthesis. These clinical results address concerns of mechanical complications that have grown out of Rangert et al.’s work
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


