CHAPTER 9 Eruption of the Teeth: Local, Systemic, and Congenital Factors That Influence the Process
CHRONOLOGIC DEVELOPMENT AND ERUPTION OF THE TEETH
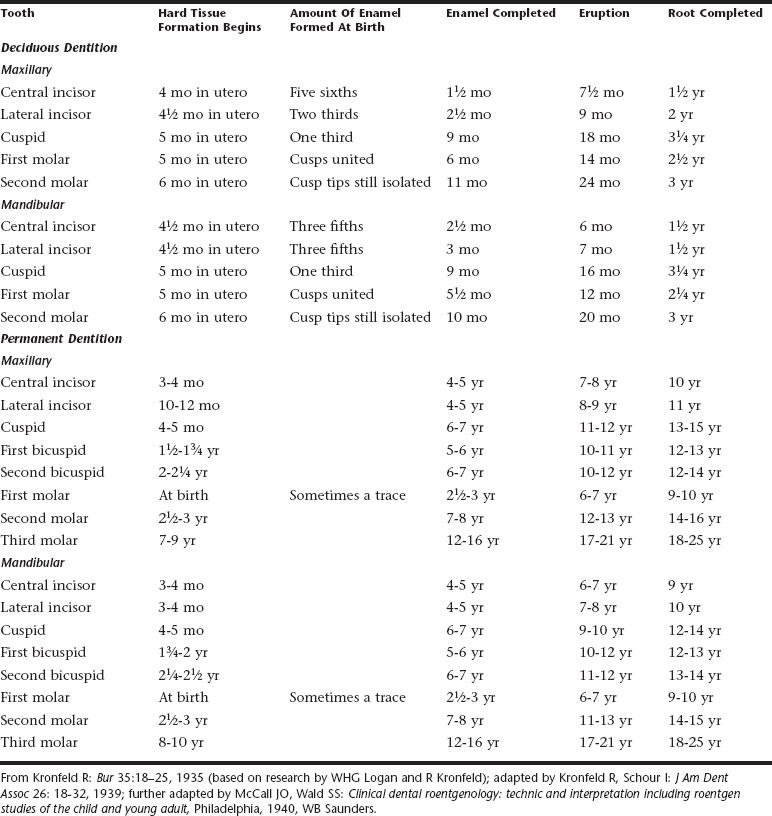
Lunt and Law made a careful review of the literature on the calcification of the primary teeth.1 They compared their findings with the values in Table 9-1 showing Logan and Kronfeld’s chronology of human dentition, which has been an accepted standard for many years.2 They offered a revised table that establishes earlier ages than those previously accepted for initial calcification (Table 9-2). A similar review was carried out for the ages at which the primary teeth erupt.3
Table 9-2 Modification of the Table “Chronology of the Human Dentition” Suggested by Lunt and Law for the Calcification and Eruption of the Primary Dentition
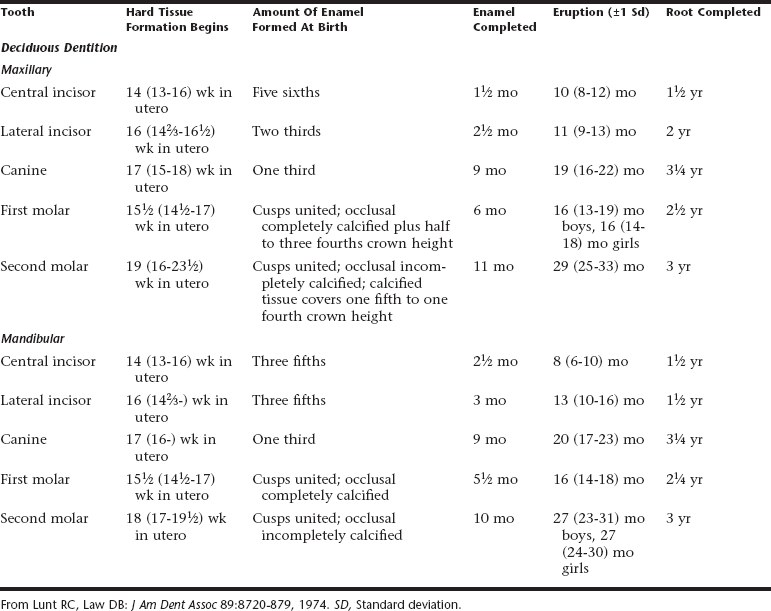
Lunt and Law concluded after reviewing the work of Kraus and Jordan and of Nomata that Table 9-1 should be modified.4,5 The sequence of calcification of the primary teeth should be changed to central incisor, first molar, lateral incisor, canine, and second molar. They determined that the times of initial calcification of the primary teeth are 2 to 6 weeks earlier than those given in Table 9-1. They also concluded that the maxillary teeth are generally ahead of the mandibular teeth in development. Exceptions are the second molars, which generally are advanced in the mandible, and the lateral incisors and canines, which at times may be ahead in the mandible.
Lunt and Law also believe that the lateral incisor, first molar, and canine tend to erupt earlier in the maxilla than in the mandible; the Logan and Kronfeld table suggests that eruption in the mandible is generally ahead of that in the maxilla. The ages at which primary teeth erupt are 2 months or more later than suggested in the Logan and Kronfeld table. Finally, Hernandez and colleagues provide confirmation that more recent studies in different white populations have findings similar to these classic studies on eruption chronology.6
The time of eruption of both primary and permanent teeth varies greatly. Variations of 6 months on either side of the usual eruption date may be considered normal for a given child. A study by Parner and colleagues compared the well-known general acceleration of the physical development of children over the past century with their own observations of the emergence of permanent teeth.7 They found that the emergence of permanent teeth has not been subject to a similar acceleration; in fact, the mean age of eruption has increased slightly, but only by a few days per year. They conclude that the age of eruption of the permanent teeth is a much more stable phenomenon than other aspects of physical development of children.
Numerous in vivo animal experiments and human radiographic studies have been done to better understand the process of tooth eruption. Although many theories have been advanced, the factors responsible for the eruption of the teeth are not fully understood. The factors that have been related to the eruption of teeth include elongation of the root, forces exerted by the vascular tissues around and beneath the root, growth of the alveolar bone, growth of dentin, growth and pull of the periodontal membrane, hormonal influences, presence of a viable dental follicle, pressure from the muscular action, and resorption of the alveolar crest.
A series of experiments by Cahill and Marks have established that a viable dental follicle is required for tooth eruption.8 Further studies by Marks and Cahill resulted in the conclusion that “tooth eruption is a series of metabolic events in alveolar bone characterized by bone resorption and formation on opposite sides of the dental follicle and the tooth does not contribute to this process.”9
Grøn observed in her study of 874 Boston children that tooth emergence appeared to be more closely associated with the stage of root formation than with the chronologic or skeletal age of the child.10 By the time of clinical emergence, approximately three fourths of root formation had occurred. Teeth reach occlusion before the root development is complete.
Demirjian and Levesque presented a large sample of 5437 radiographs from a homogeneous (French-Canadian) population.11 They used this sample to investigate the sexual differences in the development of permanent mandibular teeth from the early stages of calcification to closure of the apex. The analysis of the developmental curves of individual teeth shows a common pattern, namely, the similarity in timing between the sexes for the early stages of development. For the first stages of crown formation, which they refer to as A, B, and C, there was no difference between boys and girls in the chronology of the dental calcification in the majority of teeth. For the fourth stage, D, which represents the completion of crown development, girls were more advanced than boys by an average of 0.35 year for four teeth. For the stages of root development the mean difference between the sexes for all teeth was 0.54 year; the largest difference was for the canine (0.90 year). The data from Demirjian and Levesque show the importance of sexual dimorphism during the period of root development rather than during the period of crown development.11
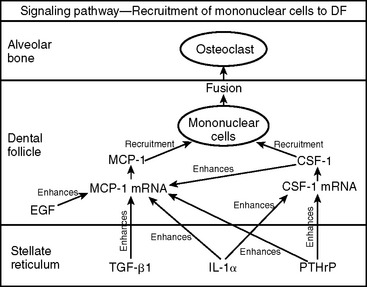
The tooth eruption process is clearly complex, and many different mechanisms are undoubtedly involved. Some of the leading scientists who are contributing to a better understanding of the tooth eruption process have written review articles to help consolidate the facts and theories associated with this process. A review article by Wise and colleagues focuses on the molecular signals that initiate tooth eruption.12 These researchers state that tooth eruption is a complex and tightly regulated process that involves cells of the tooth organ and the surrounding alveolus. Mononuclear cells (osteoclast precursors) must be recruited into the dental follicle before the onset of eruption. These cells, in turn, fuse to form osteoclasts that resorb alveolar bone, creating an eruption pathway for the tooth to exit its bony crypt. In recent years, knowledge of the biology of tooth eruption has greatly increased. What has emerged is the realization that interactions of osteoblasts, osteoclasts, and dental follicles involve a complex interplay of regulatory genes that encode various transcription factors, protooncogenes, and soluble factors. For the clinician faced with treating both simple and complex dental complications arising from abnormal tooth eruption, knowledge of the basic molecular mechanisms involved is essential (Fig. 9-1). A paper by Kardos reviews the evidence for a tooth-eruptive force as well as its direction and source.13 Finally, an extensive review by Marks and Schroeder analyzes experimental data to identify the basic principles of tooth eruption and offers their guiding theories of the process.14 For more information about the details of the tooth eruption process, refer to these review articles.
INFLUENCE OF PREMATURE LOSS OF PRIMARY MOLARS ON ERUPTION TIME OF THEIR SUCCESSORS
Posen, after reviewing the records of children in the Burlington study who had undergone unilateral extraction of primary molars, came to the following conclusions: Eruption of the premolar teeth is delayed in children who lose primary molars at 4 or 5 years of age and before.15 If extraction of the primary molars occurs after the age of 5 years, there is a decrease in the delay of premolar eruption. At 8, 9, and 10 years of age, premolar eruption resulting from premature loss of primary teeth is greatly accelerated. Hartsfield stated that premature loss of teeth associated with systemic disease usually results from some change in the immune system or connective tissue.16 The most common of these conditions appears to be hypophosphatasia and early-onset periodontitis.
VARIATIONS IN SEQUENCE OF ERUPTION
The mandibular first permanent molars are often the first permanent teeth to erupt. They are quickly followed by the mandibular central incisors. Lo and Moyers found little or no clinical significance to the eruption of the incisors before the molars.17
After analyzing serial records of 16,000 children in Newburgh and Kingston, New York, Carlos and Gittelsohn concluded that the average eruption time of the lower central incisors was earlier than that of the first molars by about 1½ months in both boys and girls.18 Of considerable interest was the gender difference in the eruption sequence of permanent teeth. The mandibular canine erupted before the maxillary and mandibular first premolars in girls. In boys the eruption order was reversed—the maxillary and mandibular first premolars erupted before the mandibular canine.
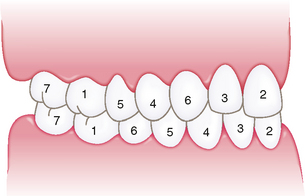
Moyers stated that the most common sequence of eruption of permanent teeth in the mandible is first molar, central incisor, lateral incisor, canine, first premolar, second premolar, and second molar.19 The most common sequence for the eruption of the maxillary permanent teeth is first molar, central incisor, lateral incisor, first premolar, second premolar, canine, and second molar (Fig. 9-2). He identified these common sequences in each arch to be favorable for maintaining the length of the arches during the transitional dentition.
A deficiency in arch length can occur if the mandibular second permanent molar develops and erupts before the second premolar. Eruption of the second permanent molar first encourages mesial migration or tipping of the first permanent molar and encroachment on the space needed for the second premolar. The importance of maintaining the second primary molar until its replacement by the second premolar is discussed in Chapter 27. In the maxillary arch the first premolar ideally should erupt before the second premolar, and they should be followed by the canine. The untimely loss of primary molars in the maxillary arch, which allows the first permanent molar to drift and tip mesially, results in the permanent canine’s being blocked out of the arch, usually to the labial side.
The eruption of the maxillary canine is often delayed because of an abnormal position or devious eruption path. This delayed eruption should be considered along with its possible effect on the alignment of the maxillary teeth. The significance of the sequence of the eruption of permanent teeth is considered further in Chapter 27.
LINGUAL ERUPTION OF MANDIBULAR PERMANENT INCISORS
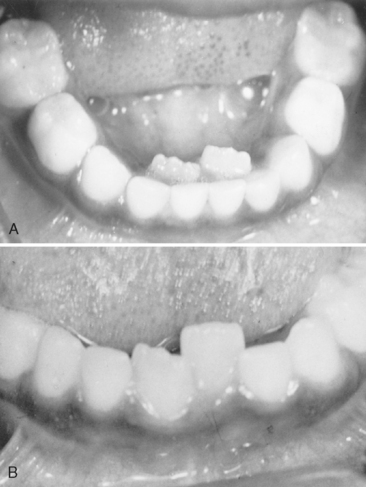
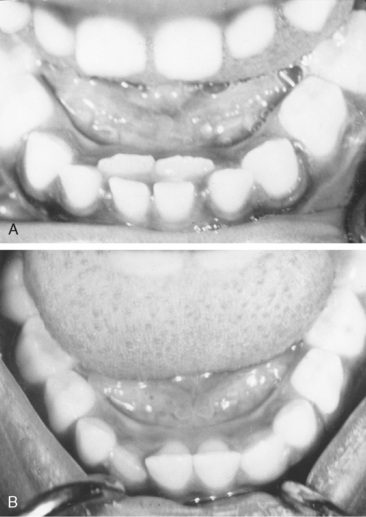
The eruption of mandibular permanent incisors lingual to retained primary incisors is often a source of concern for parents. The primary teeth may have undergone extensive root resorption and may be held only by soft tissues. In other instances the roots may not have undergone normal resorption and the teeth remain solidly in place. It is common for mandibular permanent incisors to erupt lingually, and this pattern should be considered essentially normal. It is seen both in patients with an obvious arch length inadequacy (Fig. 9-3) and in those with a desirable amount of spacing of the primary incisors (Fig. 9-4). In either case the tongue and continued alveolar growth seem to play an important role in influencing the permanent incisors into a more normal position with time. Although there may be insufficient room in the arch for the newly erupted permanent tooth, its position will improve over several months. In some cases there is justification for removal of the corresponding primary tooth. Extraction of other primary teeth in the area is not recommended, however, because it will only temporarily relieve the crowding and may even contribute to the development of a more severe arch length inadequacy.
Gellin has emphasized the anxiety created when the parents discover a double row of teeth. He suggested that if the condition is identified before 7½ years of age it is unnecessary to subject the child to the trauma of removing the primary teeth because the problem is almost always self-correcting within a few months.20 However, he warned that when lingually erupted permanent mandibular incisors are seen in an older child and the radiograph shows no root resorption of the primary teeth, selfcorrection has not been achieved and the corresponding primary teeth should be removed.
Gellin and Haley conducted a clinical study to determine whether removal of the corresponding primary tooth is necessary when the lingual eruption pattern of the mandibular permanent incisor is identified.21 They monitored 57 lingually positioned mandibular permanent central or lateral incisors in 44 children. The children were selected for the study if they had one or more permanent mandibular incisors erupting immediately lingual to the corresponding primary incisor. Other criteria required for entry into the study included the presence of both primary mandibular canines, the absence of any other anomalies of the mandibular primary or permanent incisors, and the absence of severe crowding of the permanent mandibular incisors characterized by eruption of the lateral incisors directly behind the central incisors. The mean age of the children at their first observation was 6 years, 4 months, and the ages ranged from 4 years, 10 months to 8 years, 8 months. There were 22 boys and 22 girls in the study. Of the permanent teeth studied, 47 were central incisors and 10 were lateral incisors.
In all cases, labial migration occurred naturally, and extraction of the corresponding primary incisor was unnecessary. Gellin and Haley reported that spontaneous correction of lingually erupted mandibular permanent central incisors occurred by age 8 years, 2 months in 95% of the cases that met the criteria of their study.21 They also observed that spontaneous correction of lingually erupted lateral incisors occurred by at least 8 years, 4 months of age. Although the sample of the lateral incisors was too small to draw specific conclusions, correction occurred in all cases, and central incisors migrated labially at an earlier age. Gellin and Haley recommended a conservative approach of waiting and periodic observation to spare the child a surgical procedure. They suggested that if labial migration of the permanent incisor had not occurred by 8.2 years for central incisors and 8.4 years for lateral incisors, overretention of the primary incisor should be suspected and removal of the primary tooth considered. However, they recommended removal only if the primary incisor remained firm and the root had failed to resorb.
TEETHING AND DIFFICULT ERUPTION
Some young children become restless and fretful during the time of eruption of the primary teeth. Many conditions, including croup, diarrhea, fever, convulsions, primary herpetic gingivostomatitis, and even death have been incorrectly attributed to eruption. In the nineteenth century, complications from teething were believed to be a frequent cause of infant mortality. Both King and Dally have reported that 5016 deaths in England and Wales were attributed to teething in 1839.22,23
Illingworth made a thorough search of the world literature and failed to produce evidence that teething causes fever, convulsions, bronchitis, or diarrhea.24 His findings are supported by Tasanen’s unique study of teething, in which 192 tooth eruptions were observed in 126 infants and 107 controls.25 All the babies were seen on the day of the eruption of the tooth, and records were kept of the temperature, incidence of infection, erythrocyte sedimentation rate, white blood cell count, behavior (including sleep), color of the mucosa, sensitivity of the tissue covering the erupting tooth, and pain resulting from pressure on the tooth. Tasanen concluded that teething does not increase the incidence of infection, does not cause any rise in temperature, erythrocyte sedimentation rate, or white blood cell count, and does not cause diarrhea, cough, sleep disturbance, or rubbing of the ear or cheek, but that it does cause daytime restlessness, an increase in the amount of finger sucking or rubbing of the gum, an increase in drooling, and possibly some loss of appetite. In one third of the children, there was no change in the color of the mucosa in the area of the erupting tooth, in one third of the children the change was slight, and in the remaining one third of the children there was a pronounced change in the mucosa, often with small hemorrhages.
A later study of 46 healthy infants conducted by Jaber and colleagues demonstrated a small increase in body temperature in 20 (43%) of the infants on the day of emergence of their first tooth.26 However, the authors emphasized a danger in attributing fever to teething. Macknin and colleagues have confirmed these results.27 Leung has reported that serious mistakes have been made in the care of infants and toddlers when their symptoms were ascribed to teething without completion of a thorough diagnostic evaluation and resulted in the overlooking of significant systemic disturbances.28 Swann observed 50 children who were hospitalized after their symptoms were initially attributed to teething by parents or physicians.29 After a careful medical evaluation, an organic cause of illness was identified in 48 of the 50 patients.
ERUPTION HEMATOMA (ERUPTION CYST)
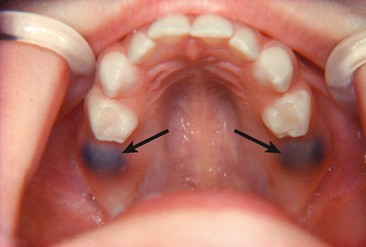
A bluish purple, elevated area of tissue, commonly called an eruption hematoma, occasionally develops a few weeks before the eruption of a primary or permanent tooth. The blood-filled cyst is most frequently seen in the primary second molar or the first permanent molar regions. This fact substantiates the belief that the condition develops as a result of trauma to the soft tissue during function (Fig. 9-5). Usually within a few days the tooth breaks through the tissue, and the hematoma subsides. Because the condition is almost always self-limited, treatment of an eruption hematoma is rarely necessary. However, surgically uncovering the crown may occasionally be justified.
ERUPTION SEQUESTRUM
The eruption sequestrum is seen occasionally in children at the time of the eruption of the first permanent molar (Figs. 9-6 and 9-7). Starkey and Shafer have described the sequestrum as a tiny spicule of nonviable bone overlying the crown of an erupting permanent molar just before or immediately after the emergence of the tips of the cusps through the oral mucosa.30 Wat/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses