CHAPTER 7 Acquired and Developmental Disturbances of the Teeth and Associated Oral Structures
COMMON DISTURBANCES IN CHILDREN
Dental care services have become more readily available to children, and caries prevention programs have become more effective. There has been a steady decline in the incidence and prevalence of dental caries in permanent teeth among U.S. children (see Chapter 10). However, according to the first Surgeon General’s report on oral health in America published in May 2000, dental caries is the single most common chronic childhood disease.1 Periodontal disturbances are also common. Although severe forms of periodontal disease are rare in children, all experience at least mild gingivitis on occasion. Both caries and periodontal disease are, for the most part, acquired and preventable disturbances of the teeth and jaws. Other chapters of this book are devoted to a more in-depth discussion of the cause, prevention, and management of dental caries (see Chapters 10, 17, 18, and 19) and periodontal disturbances (see Chapters 11 and 20). Injuries to the teeth and supporting tissues represent another large category of acquired disturbances (see Chapter 21).
Many children have orthodontic conditions that justify corrective treatment, and for some of them the condition is serious enough to be categorized as deforming or crippling. Approximately 1 in 1000 children in the United States is born with a cleft lip or palate. These conditions are primarily developmental disturbances and are discussed in greater detail in Chapters 6 and 25 to 28 26 27 28.
ALVEOLAR ABSCESS
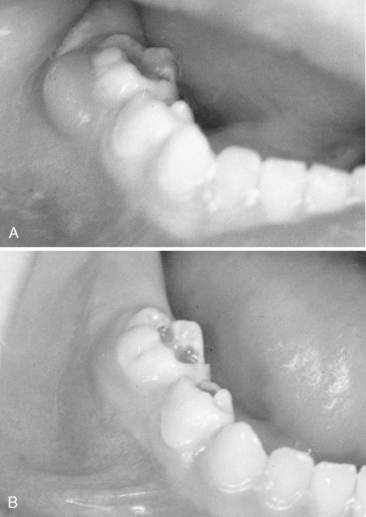
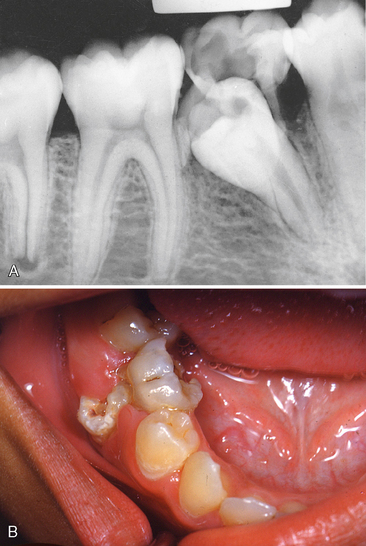
In the early stages, the acute alveolar abscess can be diagnosed based on radiographic evidence of a thickened periodontal membrane. The tooth is sensitive to percussion and movement, and the patient may have a slight fever. The acute symptoms of an alveolar abscess can be relieved by using antibiotic therapy. Relief of the symptoms is more efficient if drainage is also established (Fig. 7-1). Drainage may be established through the pulp chamber of the tooth and/or the associated gingiva or by extraction of the tooth. If extraction is selected as the best choice of treatment at the emergency appointment and the patient has an unremarkable medical history, concomitant antibiotic therapy is not always necessary. During this acute infection phase, however, it may be impossible to establish effective pain control for the extraction procedure with conventional outpatient techniques.
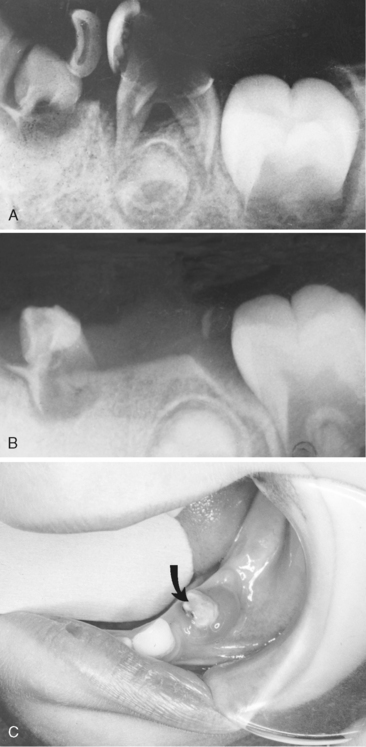
Chronic alveolar abscess, characterized by less soreness, is often a better-defined radiographic lesion. The patient will likely have some lymphadenopathy as well. Draining fistulas are also frequently associated with chronic alveolar abscesses. Usually, antibiotic therapy is unnecessary except in patients with an overriding systemic problem (e.g., patients susceptible to subacute bacterial endocarditis, patients with organ transplants, or those who are immunodeficient). Again, drainage and sterilization of the infected local area are necessary through root canal therapy for the involved tooth or through extraction. If the lesion has only recently passed the acute stage, there may be a pointing soft tissue abscess. In this situation, incising and draining the soft tissue may be indicated in addition to opening the tooth, especially if the tooth is to be treated endodontically (Fig. 7-2). If the lesion is in an advanced chronic stage, drainage may already be established as a natural reaction (Fig. 7-3).
CELLULITIS
Cellulitis is a very serious infection. It can be life threatening and is a potential complication of all acute dental infections. It is usually a result of severe untreated caries in patients who do not receive regular dental care or who may have had dental care only for treatment of dental emergencies. It is not unusual for the parents to take the child with dental cellulitis to the hospital emergency department. The child appears acutely ill and may have an alarmingly high temperature with malaise and lethargy.
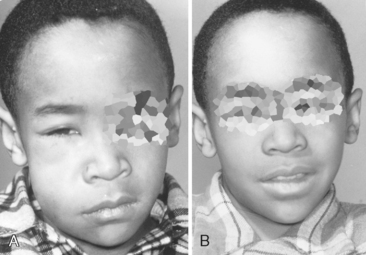
If a maxillary tooth is the problem, the swelling and redness may involve the eye (Fig. 7-4A). If cellulitis is treated too late, serious complications, such as involvement of the central nervous system or a cavernous sinus thrombosis, could occur. If cellulitis results from an infected mandibular tooth, the diffuse swelling and infection will spread to the floor of the mouth along fascial planes, nerves, and vessels. If the infection involves the submandibular, sublingual, and submental spaces, it is called Ludwig angina. In this condition the tongue and floor of the mouth become elevated to the extent that the patient’s airway is obstructed and swallowing is impossible.
The offending organisms in cellulitis from dental infections are usually capable of producing hyaluronidase and fibrinolysins. These agents break down the intercellular cementing substance (hyaluronic acid) and fibrin, which permits the rapid spread of the infection. One of the broad-spectrum antibiotics should be prescribed early to reduce the possibility of the infection localizing and draining on the outer surface of the face (see Fig. 7-4B). It should be emphasized to the parents or patient that antibiotics will not heal the condition completely and that follow-up treatment of the tooth is essential.
If the infection is already severe when the parent or patient seeks treatment, a blood culture or a culture of exudate may be performed to identify the infecting organisms. Then, if the infection does not respond to the initial antibiotic therapy, a second, more appropriate antibiotic may be selected after the causative organisms have been identified. Molinari has emphasized the continuing emergence of antibiotic-resistant bacterial strains that render many common antimicrobial agents ineffective.2
The child with cellulitis should be hospitalized if the clinical signs or symptoms warrant very close monitoring or if there is any question as to whether the parents or patient will follow through with the prescribed treatment. Hospitalization is recommended especially in the case of Ludwig angina, because maintenance of a patent airway may require the assistance of medical personnel. In these severe cases, parenteral administration of antibiotics is also recommended, at least initially.
DEVELOPMENTAL ANOMALIES OF THE TEETH
ODONTOMA
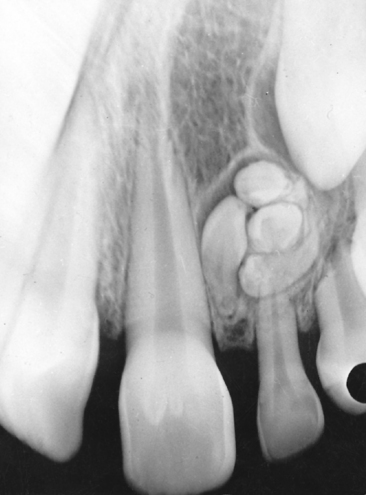
The abnormal proliferation of cells of the enamel organ may result in an odontogenic tumor, commonly referred to as an odontoma. An odontoma may form as a result of continued budding of the primary or permanent tooth germ or as a result of an abnormal proliferation of the cells of the tooth germ, in which case an odontoma replaces the normal tooth (Figs. 7-5 and 7-6). The anomaly is discussed in detail in Chapter 8. An odontoma should be surgically removed before it can interfere with eruption of teeth in the area. The presence of an odontoma should alert the practitioner to inquire about the concurrent presence of dysphagia or a family history of dysphagia that is perhaps due to hypertrophy of the smooth muscles of the esophagus as a part of the rare autosomal dominant odontoma-dysphagia syndrome.3
FUSION OF THE TEETH
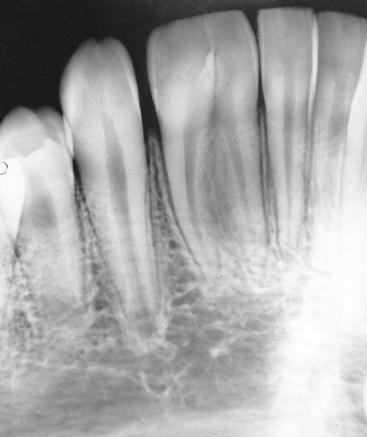
The radiograph may show that the fusion is limited to the crowns and roots. Fused teeth will have separate pulp chambers and separate pulp canals (Fig. 7-7). Dental caries may develop in the line of fusion of the crowns, necessitating the placement of a restoration. A frequent finding in fusion of primary teeth is the congenital absence of one of the corresponding permanent teeth.
Delany and Goldblatt reported an interesting case that illustrates the multidisciplinary approach that may be indicated in the clinical management of certain problems associated with fused teeth.4 The disciplines of pediatric dentistry, endodontics, surgery, restorative dentistry, and orthodontics were represented in the initial management of the case, and a post and core and a crown restoration were anticipated for the future. Yet excellent results were obtained in only 6 months with an organized approach to a complex problem that involved the fusion of a supernumerary tooth to a maxillary central incisor, severe crowding, and a palatally displaced lateral incisor. One root of the fused teeth was treated endodontically. The fused teeth were then hemisectioned, and the endodontically treated tooth was restored while the separated tooth was sacrificed. Orthodontic repositioning of the palatally displaced lateral incisor and alignment of the anterior segment concluded the management of the problem. A case of bilateral fusion of primary incisors has also been reported by Eidelman.5
The presence of a single primary and permanent maxillary central incisor may at first appear to be a product of fusion. However, if the single tooth is in the midline, and symmetric with normal crown and root shape and size, then it may be an isolated finding or may be part of the solitary median maxillary central incisor syndrome. This is a heterogeneous condition that may include other midline developmental abnormalities of the brain and other structures that can be due to mutation in the sonic hedgehog (SHH) gene, SIX3 gene, or other genetic abnormality.6 The development of only one maxillary central incisor is an indication for further evaluation for other anomalies.
GEMINATION
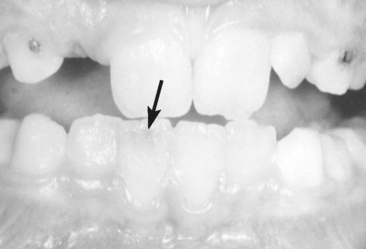
A geminated tooth represents an attempted division of a single tooth germ by invagination occurring during the proliferation stage of the growth cycle of the tooth. The geminated tooth appears clinically as a bifid crown on a single root (Fig. 7-8). The crown is usually wider than normal, with a shallow groove extending from the incisal edge to the cervical region. The anomaly, which may follow a hereditary pattern of occurrence, is seen in both primary and permanent teeth, although it probably appears more frequently in primary teeth.
DENS IN DENTE (DENS INVAGINATUS)
The diagnosis of dens in dente (tooth within a tooth) can be verified by a radiograph. The developmental anomaly has been described as a lingual invagination of the enamel. This condition can occur in primary and permanent teeth. Unusual cases of dens invaginatus have been reported in a mandibular primary canine,7 a maxillary primary central incisor,8 and a mandibular second primary molar.9 Dens in dente is most often seen in the permanent maxillary lateral incisors. The condition should be suspected whenever deep lingual pits are observed in maxillary permanent lateral incisors. Grahnen and colleagues found in a study of 58 families that a similar anomaly was present in more than one third of the parents of children with dens in dente.10 Within the same family, some had dens in dente and others had deep lingual pits, indicating that the condition may be inherited as an autosomal dominant trait with variable expressivity and possibly incomplete penetrance (see Chapter 6 for definitions).
Anterior teeth with dens in dente are usually of normal shape and size. In other areas of the mouth, however, the tooth can have an anomalous appearance. A dens in dente is characterized by an invagination lined with enamel and the presence of a foramen cecum with the probability of a communication between the cavity of the invagination and the pulp chamber (Fig. 7-9).
The advisability of performing endodontic procedures on such a tooth with pulpal degeneration depends on its pulp morphology and the restorability of the crown (Fig. 7-10).
EARLY EXFOLIATION OF TEETH
The early exfoliation of primary teeth resulting from periodontitis has been observed occasionally in young children (see Chapters 6 and 20). Along with hypophosphatasia, prepubertal periodontitis appears to be the most common cause of premature exfoliation of the primary teeth, especially in girls.
HYPOPHOSPHATASIA
Ongoing study into the etiology of hypophosphatasia indicates that the usually lethal autosomal recessive infantile type (I), as well as the usually autosomal recessive milder juvenile type (II) and the autosomal dominant adult type (III), are due to different mutations and heterozygosity versus homozygosity in the tissue-nonspecific alkaline phosphatase (TNSALP or ALPL) gene. Hu and colleagues state that, as a general rule, the earlier the appearance of the disease, the greater the severity.11 Early exfoliation of the primary teeth is usually associated with the juvenile type (II), although such a history may also be present in the adult type (III).11 Diagnostic tests should include the determination of serum alkaline phosphatase levels for parents and siblings.
Pseudohypophosphatasia, first described by Scriver and Cameron, is a rare disorder in which the child has the phenotype of juvenile hypophosphatasia and elevated levels of urinary phosphoethanolamine but plasma alkaline phosphatase activity is normal.12 However, the clinical findings are similar to those of juvenile hypophosphatasia.
CHERUBISM (FAMILIAL FIBROUS DYSPLASIA)
Cherubism is a rare childhood disease affecting jaw development. Cherubism is usually inherited as an autosomal dominant trait with somewhat reduced penetrance in females. The expression may be so variable that a clinically normal-appearing parent may have a history of prominent facial swellings or radiographic evidence of abnormal bone pattern in the mandible. Although disease progression is expected to stabilize or even regress after puberty, a few very aggressive cases, sometimes producing morbid results, have been reported.13–16 At least four cases of nonfamilial cherubism have been reported, which suggests occasional sporadic occurrences from spontaneous mutations.17–19
Two independent groups of investigators20,21 have demonstrated that the gene for cherubism maps to chromosome 4p16. Follow-up work by Ueki and colleagues found that mutations in the gene encoding c-Abl-binding protein SH3BP2 on chromosome 4p16.3 causes cherubism.22 They found several different SH3BP2 gene mutations in patients with cherubism, which probably resulted in a gain of function or dominant-negative effect, although some other gene(s) may also cause cherubism in other patients. They postulated that the onset of cherubism and its anatomically circumscribed characteristics may be related to dental developmental processes in children, when signals unique to the mandible and maxilla are transmitted through the extracellular matrix, triggered by the eruption of secondary teeth.
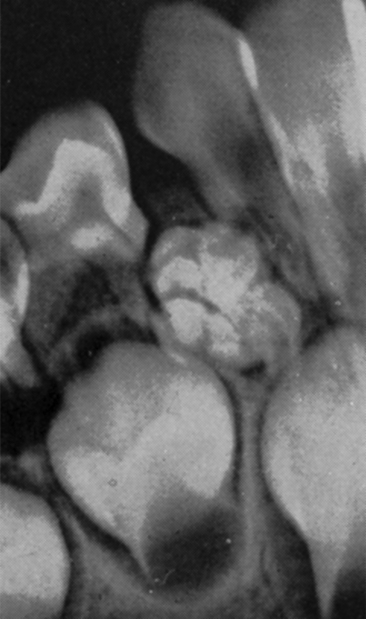
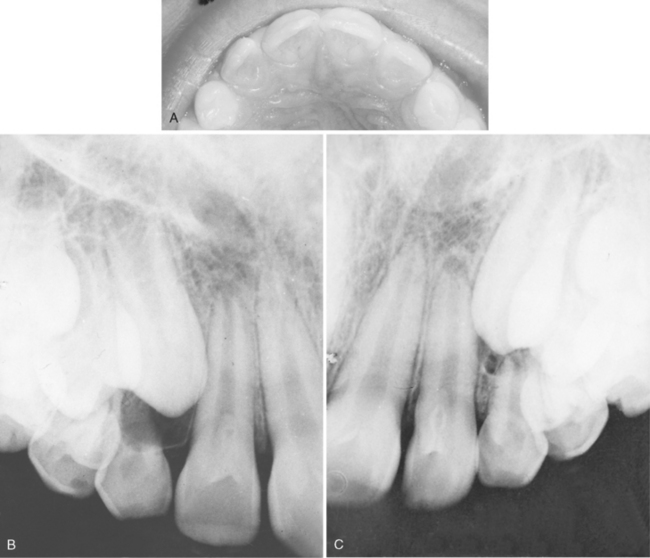
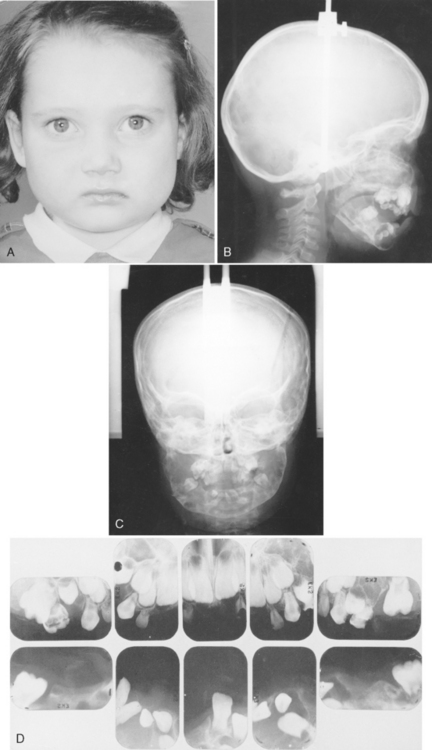
A symmetric or asymmetric enlargement of the jaws may be noted at an early age. Numerous sharp, well-defined multilocular areas of bone destruction and thinning of the cortical plate are evident in the radiograph (Fig. 7-11). Teeth in the involved area are frequently exfoliated prematurely as a result of the loss of support or root resorption or, in permanent teeth, as a result of an interference in the development of roots. Spontaneous loss of the teeth may occur, or the child may pick the teeth out of the soft tissue.
McDonald and Shafer reported a case in which the mandible and maxilla of a 5-year-old girl were symmetrically enlarged.23 Radiographs showed multilocular cystic involvement of both mandible and maxilla. A complete skeletal survey failed to reveal similar lesions in other bones. Microscopic examination of a segment of bone showed a large number of multinucleated giant cells scattered diffusely throughout a cellular stroma. The giant cells were large and irregular in shape and contained 30 to 40 nuclei. During a 10-year observation period, the bony lesions had not progressed appreciably.
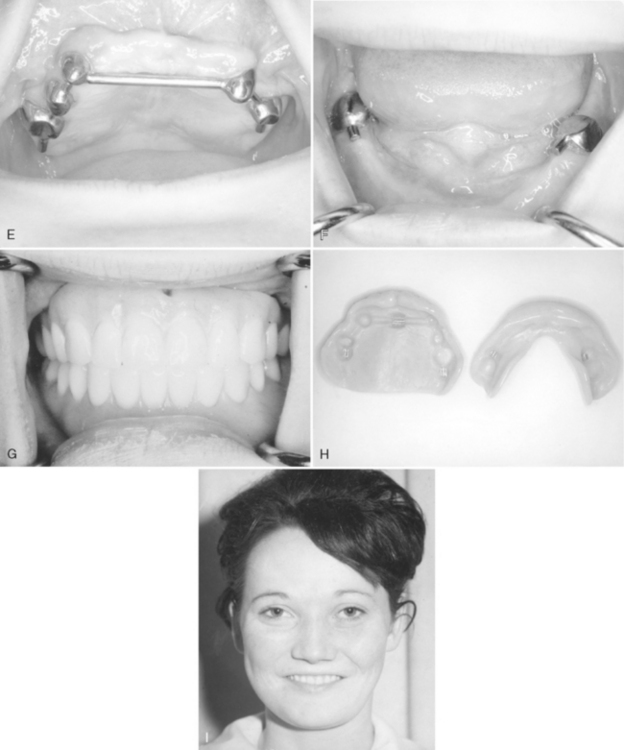
The patient illustrated in Fig. 7-11 was followed into adulthood, and her mouth was restored in a very satisfactory manner. A comparison of the full-face photographs in Fig. 7-11 (A and I) illustrates that, as the face increases in height, the “cherubic” appearance caused by the bilateral bulging of the bone of the mandible is less apparent. Seven permanent teeth in the upper and lower arches were retained and prepared for Baker attachments. Complete dentures were constructed to restore function and improve appearance.
Pierce and colleagues have reported their dental management of a mother and two daughters with inherited craniofacial fibrous dysplasia over a 15-year period.24 The daughters exhibited clinical and radiographic appearances similar to that of the patient just described, but the authors consider fibrous dysplasia and cherubism to be separate entities. Their treatment of the daughters, though more aggressive, resulted in nearly complete dentitions. Treatment included surgical autotransplantation of several teeth and bony recontouring. Orthodontic therapy was also provided for one child. Orthodontics was recommended for the other child but was declined; her dental alignment was acceptable 3 years after surgery.
Peters has reported a study of 20 cases of cherubism in one family that confirmed an autosomal dominant pattern of inheritance.25 The author preferred a conservative approach in managing the giant cell lesions, because they tend to resolve with maturity. Von Wowern published an extensive review of the literature and a 36-year follow-up of families with cherubism.26
ACRODYNIA
The exposure of young children to minute amounts of mercury is responsible for a condition referred to as acrodynia or pink disease. Ointments and medications are the usual sources of the mercury. Weinstein and Bernstein recently reported on 20-month-old twin girls who presented to a hospital with the classic signs and symptoms of acrodynia.27 Further investigation revealed that the girls had been receiving once- or twice-weekly doses of a mercury-containing teething powder during the preceding 4 months. Apparently such preparations are still available in some countries. Horowitz and colleagues reported on two young brothers who received a diagnosis of acrodynia after playing repeatedly with a broken sphygmomanometer.28 Dental amalgam restorations do not cause acrodynia.
HYPOPHOSPHATEMIA (FAMILIAL OR X-LINKED HYPOPHOSPHATEMIC RICKETS OR VITAMIN D-RESISTANT RICKETS)
As reported by Hartsfield, hypophosphatemia is the most common inherited abnormality of renal tubular transport.29 Clinical features become evident in the second year of life. They include short stature and bowing of the lower extremities in affected boys. Premature tooth exfoliation is sometimes also a feature. The inheritance pattern of the disease is usually X-linked dominant, and the disorder is twice as common in females as in males. The HYP Consortium of investigators found mutations in the PHEX (also called PEX) gene on the X chromosome in patients with this condition.30
McWhorter and Seale found that 25% of their patients with vitamin D-resistant rickets (VDRR) were affected with abscesses in primary teeth.31 The results of their study indicated that the presence of one abscess is a predictor of future abscesses in the same patient. The authors suggested that early prophylactic treatment of all posterior primary teeth with pulpotomies and crown placement may be the most conservative therapy for a patient with VDRR who develops a spontaneous abscess. However, a follow-up retrospective study by Shroff and colleagues found the success rate for prophylactic pulpotomies in these patients to be only 44%.32 They concluded that prophylactic pulpotomy therapy cannot be recommended for patients with VDRR based on the currently available data. They also suggested that a more aggressive approach using prophylactic pulpectomy as previously advocated by Rakocz and colleagues may be indicated in these patients and encouraged further investigation in this area.33
CYCLIC NEUTROPENIA (CYCLIC HEMATOPOIESIS)
Cyclic neutropenia is an autosomal dominant condition in which affected individuals are at risk for opportunistic infection during intervals of neutropenia that occur in a 21-day cycle concomitant with oscillation in bone marrow blood cell production. Levels of monocytes, platelets, lymphocytes, and reticulocytes also cycle with the same frequency. Horwitz and colleagues found several different single-base substitutions in the ELA2 gene encoding neutrophil elastase (also known as leukocyte elastase, elastase 2, and medullasin) in affected individuals, and hypothesized that a perturbed interaction between neutrophil elastase and serpins or other substrates may regulate mechanisms governing the clocklike timing of hematopoiesis.34
The condition occurs at any age. Numerous cases in children have been reported. The patients manifest a fever, malaise, sore throat, stomatitis, and regional lymphadenopathy, as well as headache, cutaneous infection, and conjunctivitis. Children exhibit a severe gingivitis with ulceration. With a return of the neutrophil count to normal, the gingiva may return to a nearly normal clinical appearance. Children experiencing repeated insults from the condition have a considerable loss of supporting bone around the teeth. A case report by da Fonseca and Fontes describes a young woman who had suffered from poor oral health throughout her lifetime, and as she approached 21 years of age, all her remaining permanent teeth were finally removed.35 Soon after the extractions, the patient’s blood counts improved to a level not previously seen by her hematologist.
OTHER DISORDERS
Premature exfoliation or marked mobility of teeth in childhood or adolescence has been associated in some cases with other systemic disorders, including acatalasia, Chédiak-Higashi syndrome, Coffin-Lowry syndrome, Down syndrome, Ehlers-Danlos syndrome types IV and VIII, Hajdu-Cheney syndrome, hyperpituitarism, hyperthyroidism, juvenile diabetes, Papillon-Lefèvre syndrome, progeria, Singleton-Merten syndrome, and some malignant diseases such as the histiocytosis X groups (see Chapter 8) and the leukemias (see Chapter 24).
ENAMEL HYPOPLASIA
Postnatal hypoplasia of the primary teeth is probably as common as hypoplasia of the permanent teeth, although the former usually does not occur in as severe a form. Hypoplasia of the primary enamel that forms before birth is rare, however (Fig. 7-12). In its mildest form, a prenatal disturbance is reflected as an accentuated neonatal ring in the primary tooth. In the severe type of neonatal disturbance, enamel formation is sometimes arrested at birth or during the neonatal period (Fig. 7-13). Postnatal amelogenesis is confined to the portion of the crown located cervically from the enamel area present at birth (Fig. 7-14).
Seow and colleagues have observed that enamel hypoplasia of the primary teeth is common in prematurely born, very-low-birth-weight children; its pathogenesis is not understood clearly.36 One likely mechanism is related to mineral deficiency, which may be diagnosed radiologically as demineralization of long bones. These authors believe that both local and systemic factors are involved. An important local factor is trauma from laryngoscopy and endotracheal intubation, which usually results in localized enamel hypoplasia involving only the left maxillary anterior teeth. Slayton and colleagues examined 698 well-nourished and healthy children 4 to 5 years of age and found that 6% had at least one primary tooth with enamel hypoplasia.37
HYPOPLASIA RESULTING FROM NUTRITIONAL DEFICIENCIES
Sarnat and Schour observed that, in a group of 60 children who had adequate medical histories, two thirds of the hypoplastic disturbances occurred during infancy (birth to the end of the first year)38 (Fig. 7-15). Approximately one third of enamel hypoplasia was found in the portion of teeth formed during early childhood (13 to 34 months) (Fig. 7-16). Less than 2% of enamel defects found originated in late childhood (35 to 80 months).
Sheldon and colleagues sought to determine whether defects in enamel were related to the occurrence of systemic ailments.39 They examined ground sections of 95 teeth from 34 patients for whom detailed medical histories were available. In more than 70% of the individuals, a positive correlation was established between the time of formation of a band of defective enamel and the existence of some systemic disability. However, defects in enamel occurred in 23% of patients who had no history of systemic conditions that might have produced enamel defects. No enamel changes occurred in 6% of patients who had histories of disabilities that had produced enamel changes in other patients. Deficiencies of vitamins A, C, and D, calcium, and phosphorus were the most common causes of defective enamel formation.
Purvis and colleagues, in a study of 112 infants with neonatal tetany in Edinburgh, observed that 63 (56%) later showed severe enamel hypoplasia of the primary teeth.40 Histologic examinations revealed a prolonged disturbance of enamel formation in the 3 months before birth. An inverse relationship was demonstrated between the mean daily hours of bright sunshine in each calendar month and the incidence of neonatal tetany 3 months later. This observation suggested that enamel hypoplasia and neonatal tetany can be manifestations of vitamin D deficiency during pregnancy and are most likely the result of secondary hyperparathyroidism in the mother. A significantly higher mean maternal age and a preponderance of lower social class was also seen in the mothers of those in the tetany group. Another study in Edinburgh indicated that only 1% of pregnant mothers took vitamin D supplements.
HYPOPLASIA RELATED TO BRAIN INJURY AND NEUROLOGIC DEFECTS
Herman and McDonald studied 120 children with cerebral palsy between 2½ and 10½ years of age (for whom complete medical records were available) to determine the prevalence of dental hypoplasia.41 The researchers compared them with 117 healthy children in the same age group and observed enamel hypoplasia in 36% of the group with cerebral palsy and in 6% of the group without the disorder. A definite relationship between the time of occurrence of the possible factors that could have caused brain damage and the apparent time of origination of the enamel defect (based on its location in the enamel on the crown of the tooth) was established for 70% of the affected teeth of children with cerebral palsy (see Fig. 7-12). Evidence of enamel hypoplasia is an aid to the clinician and the research worker in determining when brain injury occurred in patients in whom the cause is not clearly defined.
Cohen and Diner observed that enamel defects occurred with greatest frequency in children with low intelligence quotients and a high incidence of neurologic defects.42 They found that chronologically distributed enamel defects were a valuable aid in neurologic diagnosis, because they occur commonly in brain-damaged children. In addition, the defects indicate the time of insult to the developing fetus or infant even when the history is reportedly negative. Martinez and colleagues examined 170 children between 4 and 17 years of age (mean age, 12.03 years) with mental retardation and no history of dental trauma.43 They found that 37% of these children had dental enamel defects.
HYPOPLASIA ASSOCIATED WITH NEPHROTIC SYNDROME
Oliver and Owings observed enamel hypoplasia in permanent teeth in a high percentage of children with nephrotic syndrome and found a correlation between the time of severe renal disease and the estimated time at which the defective enamel formation occurred.44 Similarly, Koch and colleagues found a high incidence of enamel defects in the primary teeth of children were diagnosed with chronic renal failure early in infancy.45
HYPOPLASIA ASSOCIATED WITH ALLERGIES
Rattner and Myers discovered a correlation between enamel defects of the primary dentition and the presence of severe allergic reactions.46 Enamel defects were present in 26 of 45 children with congenital allergies. The enamel lesions were localized in the occlusal third of the primary canines and first molars.
HYPOPLASIA ASSOCIATED WITH LEAD POISONING (PLUMBISM)
Lawson and Stout observed that in areas of Charleston, South Carolina, where there were very old frame buildings, the incidence of pitting hypoplasia was approximately 100% greater than published standards or the incidence in their control group of children.47 They suggested that dentists treating children with unexplained pitting hypoplasia should consider previous exposure to lead as a part of their health evaluation, particularly if the child is from a family in a low economic stratum.
Pearl and Roland have pointed out that the fetus of a lead-poisoned mother can be affected because lead readily crosses the placenta during pregnancy.48 They observed significant delays in development and eruption of the primary teeth in the child of a lead-poisoned mother. They also listed pica (ingestion of unusual objects to satisfy an abnormal craving) as a common sign of plumbism in children 1 to 6 years old, as well as in their mothers. One mother admitted eating plaster from her apartment walls during several months of pregnancy.
HYPOPLASIA CAUSED BY LOCAL INFECTION AND TRAUMA
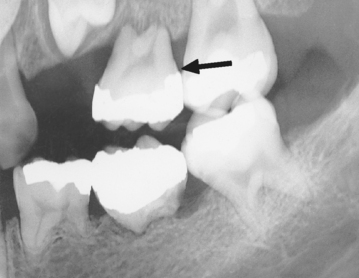
Enamel hypoplasia resulting from a deficiency state or a systemic condition will be evident on all the teeth that were undergoing matrix formation and calcification at the time of the insult. The hypoplasia will follow a definite pattern. Individual permanent teeth often have hypoplastic or hypocalcified areas on the crown that result from infection or trauma (Figs. 7-17 and 7-18).
Turner first described this localized type of hypoplasia.49 He noted defects in the enamel of two premolars and traced the defects to apical infection of the nearest primary molar. Enamel hypoplasia resulting from local infection is called Turner tooth.
Bauer concluded from a study of autopsy material that the periapical inflammatory processes of primary teeth extend toward the buds of the pertinent permanent teeth and affect them during their prefunctional stage of eruption.50 The infection fails to stimulate the development of a fibrous wall that would localize the lesion. Instead, the infection spreads diffusely through the bone around the buds of the successors and thereby affects the important protective layer of the young enamel, the united enamel epithelium.
Bauer found that in some cases the united enamel epithelium was destroyed and the enamel was exposed to inflammatory edema and to granulation tissue.50 The granulation tissue later eroded the enamel and deposited a well-calcified, metaplastic, cementum-like substance on the surface of the deep excavation.
A traumatic blow to an anterior primary tooth that causes its displacement apically can interfere with matrix formation or calcification of the underlying permanent tooth. The trauma or subsequent periapical infection frequently produces defects on the labial surface of the permanent incisor (Fig. 7-19). The retention of infected primary teeth, even if they are asymptomatic, is unjustifiable. The development of hypoplastic defects on the permanent tooth, its deflection from the normal path of eruption, and even death of the developing tooth may result.
HYPOPLASIA ASSOCIATED WITH CLEFT LIP AND PALATE
Mink studied the incidence of enamel hypoplasia of the maxillary anterior teeth in 98 patients with repaired bilateral and unilateral complete cleft lip and palate; the individuals ranged in age from 1½ 18 years.51 Among patients in the repaired unilateral and bilateral complete cleft lip and palate group, 66% of those with maxillary anterior primary teeth had one or more primary teeth affected with enamel hypoplasia; 92% of those with erupted maxillary anterior permanent teeth had one or more permanent teeth affected with enamel hypoplasia. Mink concluded that the permanent teeth are in earlier stages of development at the time of the surgical procedure and are more subject to damage.51 Dixon also attributed many of the defects of tooth structure and formation observed in patients with cleft palate to the reparative surgery.52 Vichi and Franchi, however, suggested that dental anomalies, including hypoplasia, probably result from multiple causes.53 They emphasized the difficulty in understanding the role played by genetic factors, postnatal environment, nutrition, and surgical influences in the development of the dental anomalies.
HYPOPLASIA CAUSED BY X-RADIATION AND CHEMOTHERAPY
Numerous dental abnormalities may result in surviving children who receive high-dose radiotherapy and chemotherapy during the time their teeth are forming. Kaste and colleagues reviewed clinical and radiographic records of 423 survivors of acute lymphoblastic leukemia.54 Among these patients, they observed root stunting in 24.4%, microdontia in 18.9%, hypodontia in 8.5%, taurodontia in 5.9%, and overretention of primary teeth in 4%. The patients who were younger than 8 years old at diagnosis or who received cranial irradiation (in addition to chemotherapy) developed more dental abnormalities than those older than 8 years at diagnosis and those who did not receive cranial irradiation. They also noted that the resulting dental defects may affect the survivors’ quality of life.
Maguire and Welbury point out that, as survival rates for children with cancer improve, the emphasis in therapy has moved from saving children at all costs to saving children at the least cost to the child, and therapy protocols are continually reviewed with this goal in mind.55
Children who receive high-dose x-radiation in the treatment of a malignancy are at risk for developing rampant caries in the irradiated area. The cause is generally believed to be associated with changes in salivary gland function and is discussed in Chapter 10.
Ameloblasts are somewhat resistant to x-radiation. However, a line of hypoplastic enamel that corresponds to the stage of development at the time of therapy may be seen (Fig. 7-20). Radiotherapy will have a more severe effect on the development of the dentin, and root formation will be stunted. Occasionally, development of the permanent teeth will be arrested (Fig. 7-21).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses