CHAPTER 27 Managing the Developing Occlusion
It should be the goal of every practitioner providing oral health care for children and adolescents to assess and guide the developing occlusion toward optimal outcomes. The Clinical Guidelines of the American Academy of Pediatric Dentistry1 on “Management of the Developing Dentition and Occlusion in Pediatric Dentistry” illustrates this responsibility with the following statement:
Ngan and colleagues2 illustrate this responsibility regarding contemporary practice in stating “Pediatric dentistry has increasingly shifted from a conservativerestorative approach toward a concept of total pediatric patient care. Thus all aspects of oral health care including diagnosis, prevention, oral medicine, restoration, and correction of malocclusion are increasingly the responsibility of the pediatric dentist.” In the context of these statements, clinical decisions are presented daily that challenge pediatric practitioners in affecting outcomes in management of the developing occlusion. As defined by Moyers,3 space supervision is “when the judgment of the dentist determines that the individual patient’s occlusion will have a better chance of obtaining optimum development through supervised intervention of the transitional dentition than without clinician directed intervention.” Space supervision encompasses procedures such as preventive orthodontics, guidance of eruption, interceptive orthodontics, and phased “early” orthodontic treatment that should be understood in terms of its diagnostic parameters, treatment basis, and clinical applications.
DEVELOPMENT OF OCCLUSION AND TIMING OF INTERVENTIONS
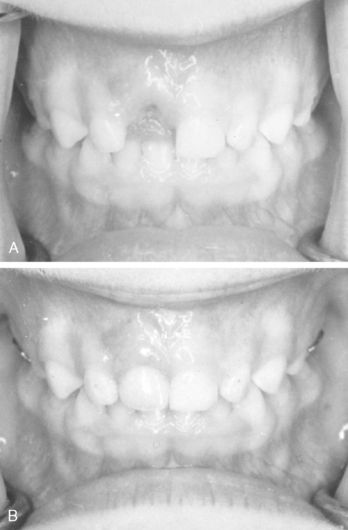
A review of studies by Baume,4 Moorrees,5,6 Bishara and colleagues7 and Moyers and Wainwright8 provides an understanding of the biogenetic course of the primary, transitional, and permanent dentitions that is critical to management of the developing dentition. Evaluating study models of the primary dentitions of 30 children obtained sequentially at various developmental stages, Baume4 reported two consistent morphologic arch forms of the primary dentition: either generalized spaces between the teeth were present (type I) or the teeth were in proximal contact without spacing (type II). The archform in both types appears congenital rather than developmental as the original pattern exhibited upon eruption was maintained from ages 3 to 6 years. Spaced arches frequently exhibit two distinct diastemas, referred to as primate spaces — one between the mandibular canine and first primary molar and the other between the maxillary lateral incisor and primary canine. Baume4 observed that until eruption of the permanent first molars, the sagittal dimension of the primary dental arches remained essentially unchanged with the possible exception of a slight decrease as the result of the development of dental caries on the proximal surfaces of the molar teeth. Only minor changes in the transverse dimension of the primary dental arches occurred during the 3- to 6-year age period unless negatively influenced by deleterious functional patterns. Given these findings, orthodontic intervention during the primary dentition up to 6 years of age is mostly directed toward maintaining inherent arch dimensions and arch integrity with preventive and restorative services. Space maintainers when primary teeth are lost prematurely are the next major consideration in maintaining arch dimensions. Control of functional problems such as elimination of deleterious thumb-sucking habits and correction of functional crossbites may also receive attention during the primary dentition years. While desirable, treatments for these factors are often deferred depending upon cooperation of the child in appliance protocols.
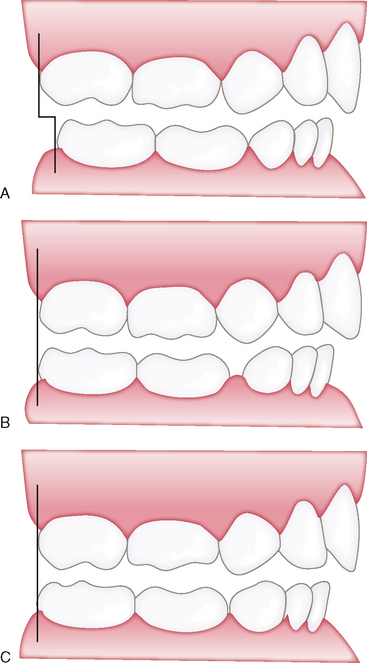
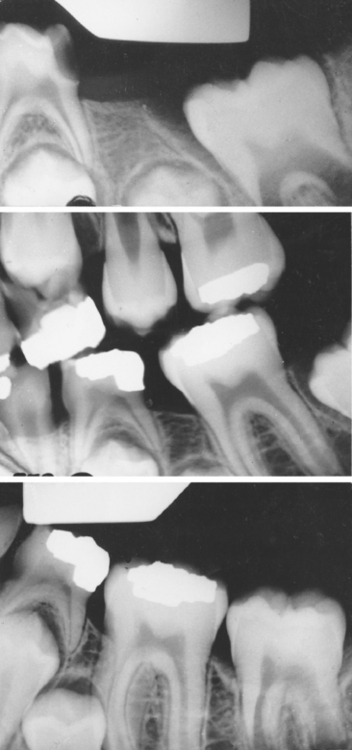
The early mixed dentition (6 to 9 years of age) is a period much more prone to localized factors that may result in severe malocclusion problems if undetected. In addition to a continuation of basic preventive and space maintenance issues, problems encountered in this period include dentoalveolar anterior crossbites, ectopic eruption of permanent incisors and/or first permanent molars, posterior crossbites, open-bite and flared maxillary incisors associated with deleterious oral habits, and developmental anomalies (e.g., ankylosis, supernumerary teeth, missing teeth). Baume,4 comparing models of 60 children before and after eruption of the permanent molars, found three distinct kinds of molar adjustment (Fig. 27-1). “Early” mesial shift during first permanent molar eruption occurs at the expense of any posterior spacing that might have been present to include breakdown spaces resulting from interproximal caries. Moyers,8 agreeing that the pattern of transition involving the straight terminal plane is normal, suggested that the occlusion forming a mesial step (distal surface of the lower second primary molar is mesial to the same surface of the maxillary molar) is most ideal for class I development. A distal step (distal surface of lower second primary molar is distal to the same surface of the maxillary molar) is indicative of a developing class II malocclusion. Proper permanent molar occlusion was achieved from a straight terminal plane by a second mesial shift of the molars as second primary molars are exfoliated. This “late” shift of the mandibular first molar, often under the additional influence of the emerging second permanent molar, occurs at the expense of the leeway space with an attendant arch length decrease of 2 to 3 mm on average.
Further evaluation by Baume indicated a transverse widening of the intercanine width of the upper and lower dental arches occurred during eruption of the permanent incisors. The increase represented a physiologic widening by lateral and frontal alveolar growth to provide space for the erupting permanent incisors and their greater mesiodistal widths. The mean increase in intercanine width was greater in the maxillary arch (3 to 4 mm) than in the mandibular arch (2 to 3 mm). In the mandibular arch, the greatest tendency to increased width was during the eruption of the lower lateral incisors, whereas in the maxillary arch it occurred primarily during eruption of the maxillary central incisors. Whereas the increase was slightly greater in nonspaced primary arches than in spaced arches, the arches with spaces generally resulted in favorable alignment of the permanent incisors. About 40% of the arches without primary dental spacing resulted in crowded anterior segments. Moorrees reported similar dimensional changes concurrent with incisor transitional periods.5
Bishara and colleagues7 also reported arch dimensional changes in their studies of patients from age 6 weeks to 45 years of age, noting that (1) significant maxillary and mandibular arch width increases occurred between 6 weeks and 2 years of age, (2) the mandibular intercanine width was established by 8 years of age (i.e., after eruption of the four incisors), (3) although arch width increased between 3 and 13 years of age, there was a slight decrease in width, more in the intercanine than intermolar area, after complete eruption of the permanent teeth. In sum, incisor alignment patterns and intercanine arch dimensions are essentially established by age 8 years of age. Interceptive procedures receive significantly more emphasis in this period to allow a harmonious transition directed toward achieving alignment of the permanent incisors and 6-year molars with symmetrical arch development and coincident midlines. Additionally, early recognition and elimination of deleterious oral habits or deviant functional patterns should enhance normal patterns of development while diminishing the long-term effects of atypical growth.
In addition to malocclusion factors identifiable during first molar and incisor transition, corrective measures to align and position the erupting buccal segments come into play during the late mixed dentition (9 to 12 years of age) when primary canines and molars are exfoliating in conjunction with eruption of the permanent canines and premolars. Epidemiologic studies demonstrate that crowding and malalignment become significantly more prevalent and exhibit greater severity between the mixed dentition period (6 to 12 years of age) and the adolescent young permanent dentition (12 to 18 years of age). This suggests that normal transitional changes do not compensate for anterior malalignment and crowding in that late mesial shift of the buccal segments upon exfoliation of second primary molars results in decreased arch length and arch circumference. Nance9 observed that in the average patient’s mandibular arch, a leeway size difference of +1.7 mm per side exists with the combined mesiodistal widths of the primary canine, first primary molar, and second primary molar being larger than the mesiodistal widths of the corresponding permanent canine and premolars. The difference between the total width of the corresponding three primary teeth in the maxillary arch compared with the three permanent teeth that succeed them is +0.9 mm per side of leeway space. The control of this leeway space in terms of arch dimensional change through space supervision may offer opportunities to significantly improve tooth size–arch size adjustments for the relief of typical levels of crowding. Gianelly10,11 and others have shown that the control of leeway space will accommodate typical levels of lower incisor crowding in approximately 75% of mixed dentition patients presenting for orthodontic treatment. As applied to the late mixed dentition, a positive excess leeway space to an overall deficiency of less than 2 mm per quadrant may be considered potential situations for space supervision programs. Lower arch length deficiencies of more than 2 to 3 mm per quadrant should be considered a discrepancy beyond simple guidance procedures.
In answering these questions, a thorough clinical examination supported by appropriate diagnostic records should be obtained before initiating treatment interventions. The clinical examination should assess the patient’s overall health status, extraoral facial patterns (profile, facial symmetry, area of discrepancy), occlusion from an esthetic and functional standpoint, temporomandibular joint function, neuromuscular patterns, growth patterns, and nasopharyngeal airway patterns. A form similar to the one depicted in Fig. 27-2 is helpful in composing clinical findings and formulating the patient’s diagnosis, problem list, and treatment plan summary. In terms of diagnostic records beyond clinical findings, necessary records may range from simple photos or study models when treating a functional posterior crossbite to a complete set of orthodontic records for a patient with a skeletal malocclusion or severe crowding. More comprehensive records may include an eight-film series of extra and intraoral photographs, appropriately trimmed orthodontic study models, a full-mouth series or panoramic radiograph, lateral and anteroposterior cephalograms, and when indicated temporomandibular diagnostic views such as corrected axis tomograms or magnetic resonance imaging. Supplemental diagnostic procedures can also include a detailed tooth-size arch-size space analysis (Chapter 25) and a cephalometric analysis (Chapter 26). And finally, cone beam computed tomography should be considered in special cases, such as impacted teeth or craniofacial patients.
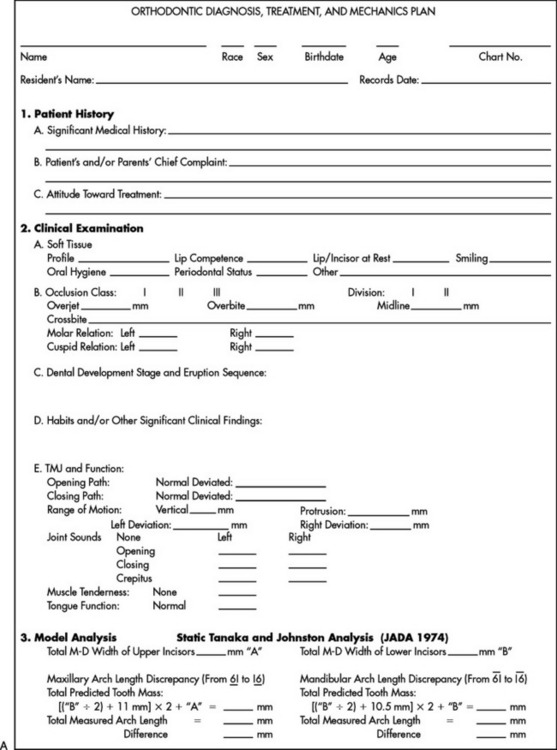

Figure 27-2 “Orthodontic Diagnosis and Treatment Plan” form. A, Front side. B, Back side. IUSD Pediatric Dentistry.
EARLY LOSS OF TEETH AND SPACE MAINTENANCE
If arch integrity is disrupted by early loss of primary teeth, problems may arise that affect the alignment of the permanent dentition. Opposing teeth can supraerupt, more distal teeth can drift and tip mesially, and more forward teeth can drift and tip distally (Figs. 27-3 and 27-4). Altered tooth positions may include a “symptomatic” space deficiency with loss of arch length and circumference, blocked or deflected eruption of permanent teeth, unattractive appearance, food impaction areas, increased caries and periodontal disease, and other negative aspects of malocclusion. The altered occlusal relationships may evidence traumatic interferences and untoward jaw relationships. When early primary tooth loss occurs, corrective measures such as passive space maintenance, active tooth guidance with space regaining, or a combination of both may be needed to optimize the normal process of occlusion development.
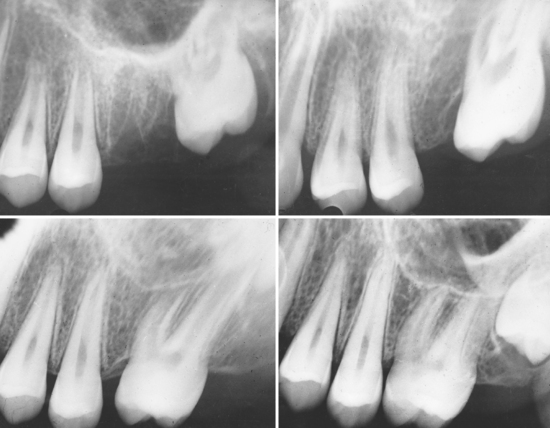
Miyamoto and colleagues12 observed the effects of the early loss of primary teeth by measuring crowding and malalignment in the permanent dentition of 255 schoolchildren aged 11 years or older. Children who had premature loss of one or more primary canines or molars were more likely to receive orthodontic treatment in the permanent dentition with the need more than three times greater in children who had lost one or more primary teeth through 9 years of age than the control group. Premature loss of primary molars was especially associated with major malalignment of permanent teeth. No differences were observed in effects between loss of first and second primary molars. Crowding of anterior teeth was directly affected by the premature loss of primary canines. A review of the clinical literature by Owen13 revealed the following general factors should be considered in assessing the implications of premature loss of primary teeth to arch development, the development of a malocclusion, and the need for a space maintainer.
Individual permanent teeth are often observed to be delayed in their development and consequently in their eruption timing. Impacted permanent teeth or deviations in eruption paths may be reflected with abnormally delayed eruption times. In cases of this type it is generally necessary to extract the primary tooth, construct a space maintainer, and allow the permanent tooth to erupt and assume its normal position (Fig. 27-5). The exact timing of permanent tooth eruption is less important in the overall occlusion development compared with greater significance related to sequencing, site of eruption, and adequate space for subsequent eruption.
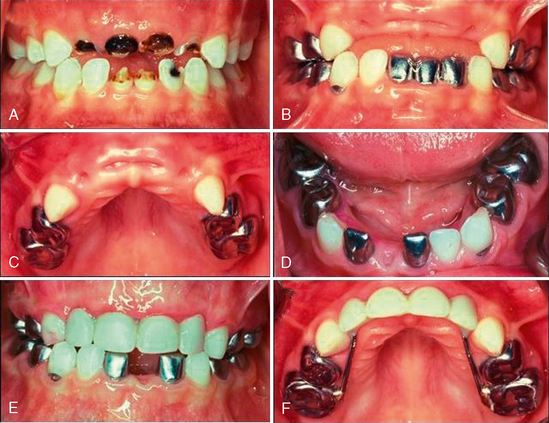
Loss of Primary Incisors
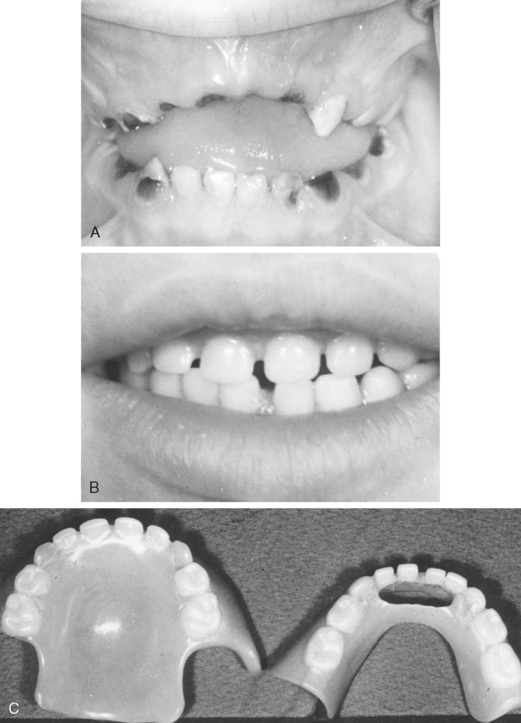
Premature loss of maxillary primary incisors does not generally result in decreased upper intracanine dimensions if the incisor loss occurs after the primary canines have erupted into occlusion at approximately 2 years of age. The support of the mandibular occlusion “holds” the maxillary anterior intracanine width dimensions. Baume type I spaced primary dentitions have significant latitude to resist arch dimensional changes. If the anterior primary teeth were in contact before the loss or there is evidence of an arch-length inadequacy in the anterior region, space adjustments in alignment after the loss of one of the primary incisors is a potential factor in space maintenance (Fig. 27-6). The major consequence of early loss of maxillary primary incisors is most likely delayed eruption timing of the permanent successors as reparative bone and dense connective tissue covers the site. In addition, unattractive appearance and potential development of deleterious habits (e.g., tongue-thrust swallow, forward resting posture of the tongue, improper pronunciation of fricative sounds—“s,” “f”) may be of concern following premature loss of primary maxillary incisors. An anterior appliance incorporating artificial primary teeth may be considered to satisfy esthetic and functional needs. Acrylic partial dentures have been successful in the replacement of single (Fig. 27-7) and multiple (Fig. 27-8) maxillary primary incisors. Given the demands of cooperation in wear and frequent appliance loss or damage, such removable appliances can be problematic in preschool-age children.
A fixed option using primary incisor denture teeth secured from a rigid steel wire (0.036 or 0.040) extended to bands or stainless steel crowns on the primary molars, a so-called “Hollywood” bridge, may be a more predictable option (Fig. 27-9). One can obtain additional stabilization in keeping the wire from flexing by placing an occlusal rest on the first primary molar, using a Nance button, or by covering the ridge with acrylic resin. Use of such an appliance incorporating artificial primary anterior teeth is elective to primarily address esthetic demands rather than specific space management concerns.
Loss of Primary Canines
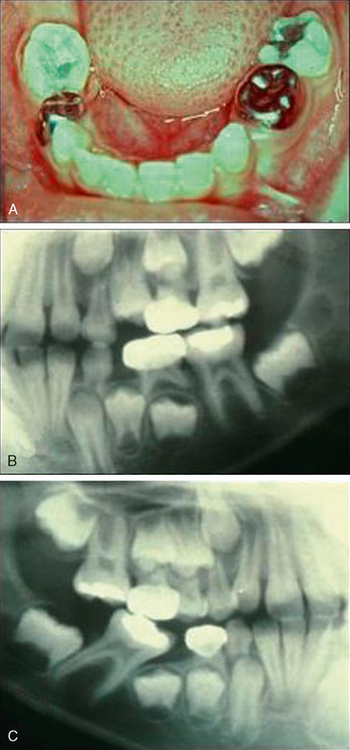
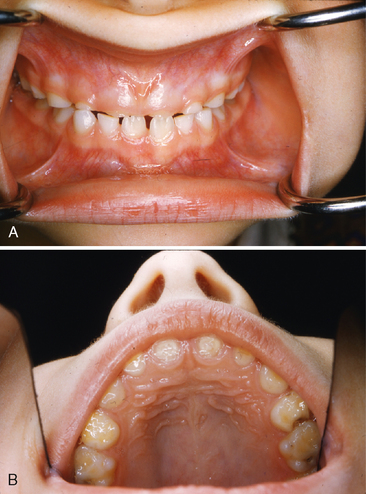
Most often due to ectopic eruption of permanent lateral incisors, early loss of a mandibular primary canine is a significant indicator of a tooth size-arch size discrepancy. Unilateral loss of a lower primary canine is frequently followed by a shift in the dental midline toward the side of loss, lingual collapse of the incisor segment, and possibly deepening of the bite (Fig. 27-10A, B). The asymmetric disruption in arch integrity complicates normal eruption of the permanent canines and premolars toward the affected side. If ectopic eruption involves bilateral loss of both lower primary canines, pronounced lingual inclination and distal drifting of the permanent incisors, deepening of the overbite, increased overjet, and significant loss of arch perimeter is likely to be the alignment result (see Fig. 27-10C, D).
The ectopic loss of maxillary primary canines occurs less frequently than mandibular loss given more favorable space adjustments for incisor liability. When it occurs, ectopic loss of a maxillary primary canine typically reflects a very distal eruptive displacement of the permanent lateral incisor and not necessarily a significant tooth mass problem. Atypical upper anterior alignment may occur with resultant crowding and blockage of the permanent canine because it erupts so late in normal transition. Early loss of maxillary primary canines is an indicator for early orthodontic treatment with an understanding the child is a definite candidate for comprehensive orthodontic intervention.
Loss of First Primary Molars
The effect of premature loss of first primary molars in both arches is mostly dependent on the state of eruption of the first permanent molars. If the primary first molar is lost during the primary dentition from ages 3 to 5 years, there should be little or no space loss associated with mesial movement of the second primary molar. However, as first permanent molars erupt at age 5 to 7 years, a strong force is exerted that pushes the second primary molar forward into the first primary molar space (see Fig. 27-3B). This results in a loss of posterior arch length within the quadrant that can lead to crowding as the canines and premolars erupt in later stages. In addition to posterior effects, mandibular arch length may be further compromised by distal and lingual shifting of anterior teeth toward the side of first primary molar tooth loss. Therefore loss of a first primary molar in either arch approximating eruption of first permanent molars indicates use of a space maintainer is generally desirable to stabilize second primary molar and canine positioning.
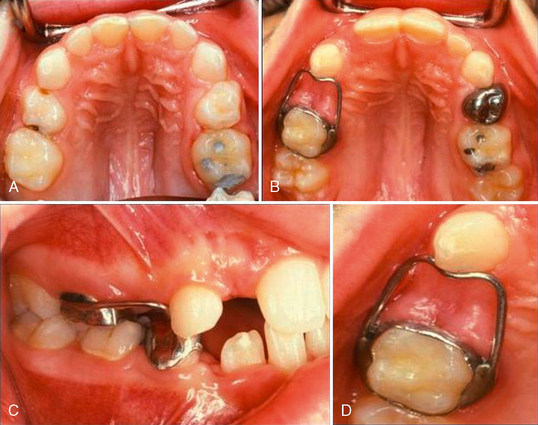
A unilateral fixed space maintainer called a band or crown and loop is usually the appliance of choice for early loss of first primary molars. The appliance incorporates a band or crown on the second primary molar with a soldered wire-loop extension extending forward to contact the distal-cervical surface of the primary canine in the quadrant (Fig. 27-11). The loop uses 0.036 or 0.040 stainless steel wire strong enough to withstand biting forces while ensuring a rigid abutment contact in stopping forward movement of the second primary molar and distal movement of the primary canine. Wire design approximates the gingival contour of the extraction space to avoid occlusal interferences and is wide enough to allow the permanent tooth to erupt. A modification of the design is use of a single-wire extension “arm” rather than a full loop from the posterior abutment to contact the anterior abutment (Fig. 27-12). The single arm of 0.036 or 0.040 wire is rigid enough to hold the space while reducing by half possible interferences to eruption of the underlying tooth. Neither the loop nor the arm design restores chewing function or prevents eruption of opposing teeth, a possible consideration in some cases. In addition, the wire may inhibit primary canine distolateral movement as permanent incisors erupt, particularly in association with lower lateral incisor eruption. For this reason, the status of permanent incisor eruption sequencing, symmetry, and positioning should be monitored and guidance steps taken to optimize normal incisor eruption. The clinician must recognize these limitations and prepare for modifications in the overall space supervision planning.
The use of a band as the abutment attachment makes it easy and economical to construct, takes little chair time, and adjusts readily to accommodate the changing dentition. The use of a stainless steel crown as the abutment base (Fig. 27-13) offers the advantage of increased stability and retention. A crown is used if the second primary molar has extensive caries or if the tooth has had vital pulp therapy. The steel crown should be prepared as described in Chapter 18. An impression is made, the crown removed from the tooth and seated in the impression, and a working model prepared on which to fabricate the loop. Because it is difficult to remove the crown (converted to a band) to make adjustments, adapting a band or one size larger crown over a cemented crown restoration and constructing a conventional band and loop appliance is another alternative to address unilateral space maintenance (Fig. 27-14).
If first primary molars are lost bilaterally within a lower arch and the second primary molars are retained, two separate unilateral loop appliances are generally indicated until first permanent molar and incisor eruption are complete. Bilateral lingual holding arch designs should not be placed before eruption of the permanent incisors as the lingual wire may interfere with incisor positioning during eruption. Additionally, primary incisors as anterior stops do not offer sufficient anchorage to prevent loss of arch length in most cases. Either of the loop or arm designs is relatively effective as long as the clinician realizes the appliances are dependent on abutment teeth that may exfoliate before the need for space maintenance is complete. After the permanent incisors have fully erupted and as the primary canines and molars exfoliate, a second appliance that stabilizes final permanent molar position and arch length may be necessary to prevent subsequent space loss.
Loss of Second Primary Molars
If a second primary molar is lost in a child 2 to 5 years of age, no space loss should occur while the first permanent molar is in basal bone. The options in managing such early loss are very limited due to lack of retention elements for fixed appliances and patient cooperation in the use of appliances at this age. As first permanent molars erupt, however, considerable loss in arch length can occur if no second primary molar is present as an eruptive guide (Fig. 27-15). Space loss of as much as 8 mm in a maxillary quadrant has been documented as the first permanent molar displaces forward through bodily crown-root movement and mesiolingual rotation around the palatal root. Early loss of lower second primary molars in conjunction with first permanent molar eruption timing results in up to 4 to 6 mm of space loss during transition. The lower first molars move forward by pronounced mesial tipping of the crown with more modest bodily tooth movement expressed in molar adjustments. Distal movement and retroclination of teeth anterior to the space is also a likely consequence to early loss in the lower arch. If the loss of the second primary molar occurs after the first permanent molars have fully erupted and normal cuspal interdigitation has been established, the degree of space loss should be less dramatic than earlier during molar transition regardless of arch involved. However, mesial movement of the permanent molar through lack of buttressing support from the missing second primary molar usually results in space loss that may be significant in amount. Quadrant space loss on the order of 2 to 3 mm without the buttressing support of the second primary molar may be realized—easily enough to compromise positioning of the permanent canines and premolars.
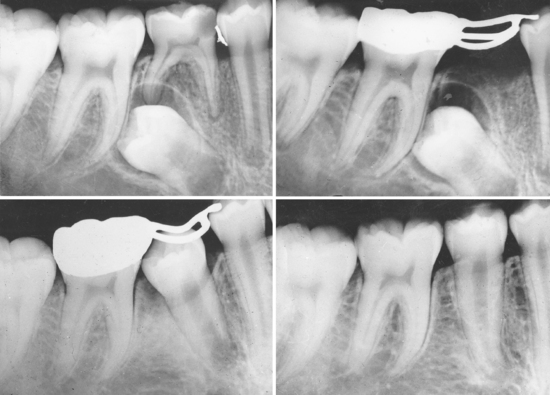
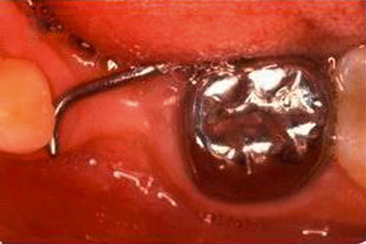
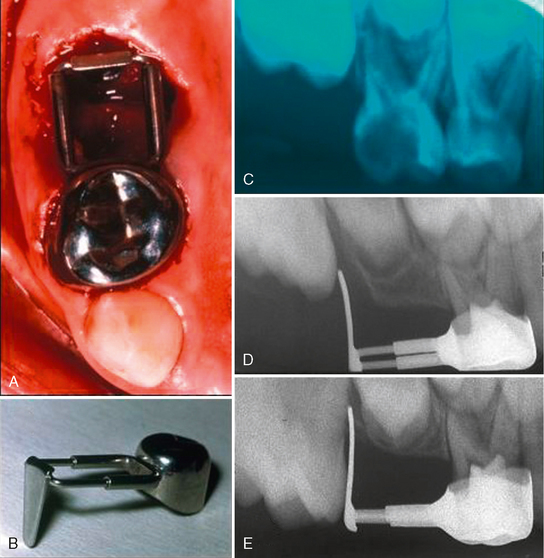
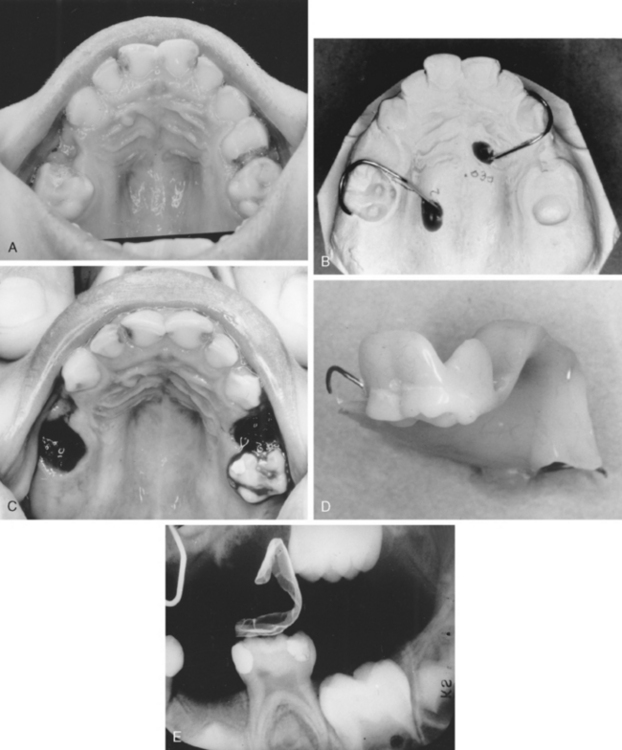
Given the findings regarding space loss with second primary molars, a space maintainer is generally indicated in most patients to control permanent molar positions. If the loss occurs just before eruption of the first permanent molar, that is, when the first molar crown is still covered with oral mucosa and a thin partial covering of bone, a space maintainer to guide the positioning of the first permanent molar into normal occlusion is desirable. The appliance of choice is a distal shoe for both the maxillary (Fig. 27-16) and mandibular arches. The appliance incorporates a posterior wire-loop extension from the first primary molar that supports a vertical tissue blade positioned to contact and guide the erupting permanent molar into normal position. The depth of the intragingival extension should be about 1.0 to 1.5 mm beyond the mesial marginal ridge of the molar to “capture” the surface as the tooth erupts vertically. Gauged in length to represent the missing second molar, accurate placement is critical to insure that the distal shoe does not extend too far distally over the first molar and block its eruption, nor be too short and not maintain the space occupied by the lost second primary molar. It has been observed that the soft tissue tolerates the blade extension well, although a small metallic “tattoo” in the gingiva may result.
The first primary molar is first prepared with a stainless steel crown or well-adapted band that provides a retentive base for the distal shoe. An impression is made to prepare a working model. If the primary second molar has not yet been extracted, it is cut off the model and a hole made with a bur that simulates the position of the distal root of the tooth. If the second primary molar has been removed previously, the positioning of the tissue extension may be determined with measurements on bite-wing or periapical radiographs or by measuring the mesiodistal width of the contralateral second molar. The extension blade is contoured, extended distally into the prepared opening on the model and the loop soldered to the band or crown. An alternative in design is the use of an adjustable Gerber extension employing a trombone-type attachment with the sleeve portion tach-welded or soldered to the band or crown (see Fig. 27-16). The sliding extension can be positioned into the tube sleeve and the posterior length adjusted to the proper spacing with the blade extension positioned directly into the extraction space or a surgical incision made just at the mesial contact area of the erupting first permanent molar. Crimping of the sleeve tube holds the length of the established extension loop. The tach-welded area should ideally be supported with additional solder to reinforce the appliance from occlusion forces. Before final placement, a radiograph of the distal shoe in position should be made to determine whether the extension is in proper relationship with the unerupted first permanent molar. Final adjustments in length and contour may be made to make sure mesial contact of the first permanent molar is provided. Brill,15 in describing chair-side fabrication procedures, presents the distal shoe as an efficient and cost-effective appliance for guiding the unerupted permanent first molar into position with success rates relatively equal to studies looking at the longevity of other space maintainers.
Several conditions contraindicate the use of distal shoe appliances. Given the extent of caries involvement, there may be lack of abutments to support a cemented appliance. Poor oral hygiene or lack of patient and parental cooperation greatly reduces the possibility of a successful clinical result. Histologic studies show that the distal shoe does not become lined with epithelium and is associated with a chronic inflammatory response. Therefore certain medical conditions such as blood dyscrasias, immunosuppression, congenital heart defects, history of rheumatic fever, and diabetes contraindicate the use of the appliance. If the distal shoe is contraindicated, two possibilities for treatment exist: (1) allow the tooth to erupt and regain space later, or (2) use a removable or fixed appliance that does not penetrate the tissue but places pressure on the ridge mesial to the unerupted permanent molar (Fig. 27-17). Carroll and Jones16 reported on a pressure-type appliance successfully used to guide the permanent molar as it erupted. Given the fact that the first permanent molars are guided in their eruption by the distal-cervical aspect of the second primary molar, the acrylic or pressure extension usually serve as an ineffective guide for eruptive positioning. The removable extension is more likely to work in the lower arch if the eruption bulge area of the first permanent molar can be engaged with the acrylic. If several teeth are missing, the removable appliance can serve to restore function and prevent super-eruption of opposing teeth.
After the first permanent molar has been guided into position, a distal shoe is usually indicated for replacement with a different appliance. Continued vertical development will usually result in tipping of the permanent first molar over the top of the blade extension with resulting space loss and tissue complications. One option is to remove the intragingival extension and replace it with a reverse band and loop employing an occlusal directed extension to prevent the molar from tipping over the wire. Exfoliation of the first primary molar as an abutment may also occur before eruption of the second premolars. So a more preferred option to replace a distal shoe once the first permanent molars have erupted adequately to be banded is the use of a bilateral space maintainer such as a mandibular lingual holding arch, maxillary transpalatal bar, or maxillary Nance appliance. These same bilateral space maintainers are the method of choice to provide stability to first permanent molar positions whenever the second primary molars are lost and first permanent molars have erupted into occlusion. Even after first permanent molar occlusion is established, the loss of second primary molars will potentially result in significant amounts of closure without the buttressing effect of the primary second molar.
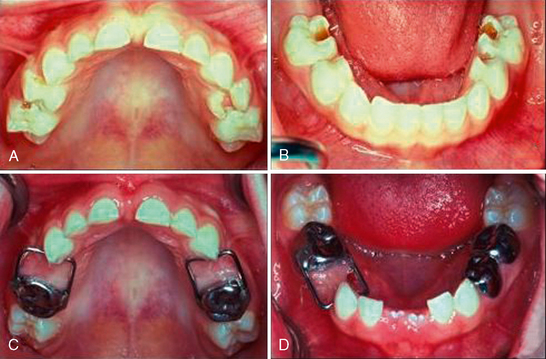
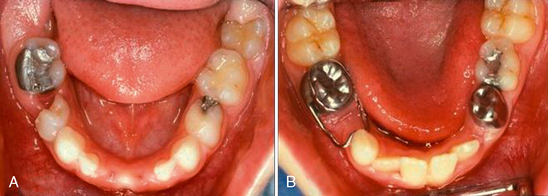
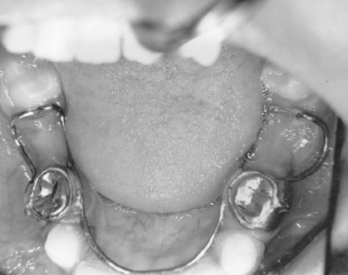
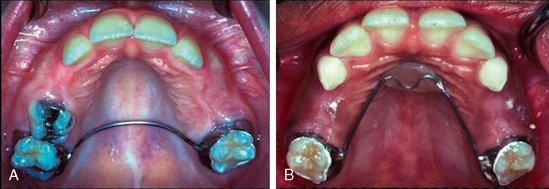
The classic bilateral mixed dentition space maintainer in the mandibular arch is the soldered lingual holding arch (Figs. 27-18). With bands fitted to the first permanent molars, a 0.036- or 0.040-inch steel wire is contoured to the arch and extended forward to make contact with the cingulum area of the incisors (Fig. 27-19). The design stabilizes lower molar positions from moving mesially and incisor relationships from retroclining lingually in sustaining the canine-premolar segment space (i.e., leeway space). The lingual wire must simply be contoured to not interfere with normal eruption paths and provide an anterior arch form so that the incisors have an opportunity for alignment. In the mixed dentition, the soldered lingual holding arch should present minimal problems with breakage, minimal oral hygiene concerns, minimal interference in eruptive movements of permanent canines and premolars, and no concerns about whether the child is wearing the appliance. Importantly, the bilateral design and use of permanent teeth as abutments allows application during the full transitional dentition period of the buccal segments. As stated earlier, lower lingual arches should not be placed before the eruption of the permanent incisors because of their frequent lingual eruption path. The lingual wire may interfere with normal incisor positioning if the appliance is in position before lateral incisor eruption. Additionally, abutting against primary incisors as anterior stops does not offer sufficient anchorage to prevent significant loss of arch length.
Used in the maxillary arch to stabilize molar positions bilaterally, the soldered transpalatal bar incorporates a transverse palatal wire of 0.036 or 0.040 stainless steel wire soldered to molar abutments (Fig. 27-20A). The rigid transverse wire prevents the two main space loss patterns of upper first permanent molars: mesiobuccal rotation and anterior bodily displacement. While the appliance may allow some minor mesial tipping of the upper molars, this is generally considered insignificant as to overall space loss in the maxillary arch. The simple transpalatal contour of the connector wire offers the main argument for this appliance: It is easy to fabricate and offers minimal irritation to the palatal tissue or tongue. The Nance appliance uses a contoured rigid wire with an acrylic “button” contacting the palatal shelf as an anterior stop for bilateral molar stabilization in the maxillary arch (see Fig. 27-20B). Providing the same molar rotation and bodily movement control as transpalatal bars, the added bracing of the acrylic button against the anterior palatal vault offers some additional resistance against forward tipping movements of the molars. Whereas the bilateral stability of the transpalatal appliance appears adequate in most situations, the resistance of the Nance with its acrylic palatal stop is preferred by some clinicians. Tissue irritation beneath the button does not appear to be a clinical problem in most cases if proper hygiene is followed.
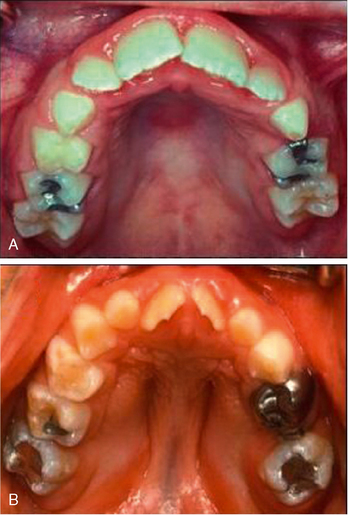
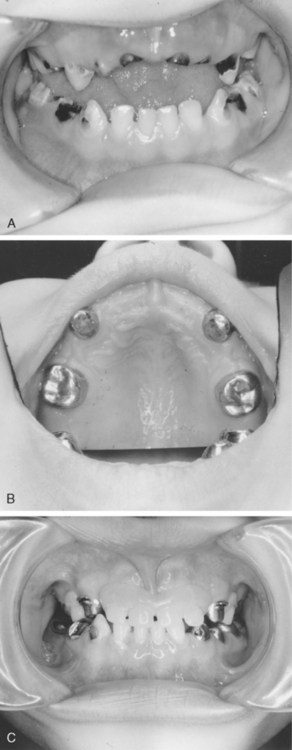
Areas of Multiple Primary Molar Loss
Loss of multiple primary molars may lead to mutilation of the developing dentition unless an appliance is constructed to maintain relationships of remaining teeth and to guide eruption of the developing teeth. In addition to arch dimension concerns, reduced masticatory function is undesirable from a nutritional standpoint. Removable acrylic partial dentures have been used successfully in either arch after the loss of multiple teeth. If artificial teeth are included, an essentially normal degree of function and acceptable esthetics can be restored. The disadvantages lie in their unpredictability outside the clinicians control because the appliances require patient cooperation and can be easily lost or broken during wear. During the transitional stages of exfoliation and eruption, stability of removable appliances is often difficult to sustain with the loss of abutments. The wire clasps and resin contact areas may present “food-traps” for plaque accumulation, with increased potential for soft tissue irritation and dental caries.
If the loss of one or both of the second primary molars occurs a short time before the eruption of the first permanent molars, the acrylic removable appliance may be considered in preference to one of the distal shoe maintainers described previously. An acrylic partial denture with a distal extension to guide first permanent molars into position may be used (Fig. 27-21). The teeth to be extracted are cut away from the stone cast and a depression is cut into the stone model to allow the fabrication of the acrylic extension. The acrylic will extend into the alveolus after removal of the primary teeth. The extension may be removed after eruption of the permanent tooth. It is occasionally necessary to recommend extraction of all the primary teeth in a preschool child. Although this was more common in the prefluoridation era, some children even today must have all of their teeth removed because of widespread oral infection and because the teeth are nonrestorable. Preschool children can wear complete dentures successfully before the eruption of permanent teeth (Fig. 27-22).
Loss of First Permanent Molars
The second molars, even if unerupted, start to drift mesially after the loss of the first permanent molar. A greater degree of forward bodily movement will occur with loss of the first permanent molar in children in the 8- to 12-year age group. In older children, if the loss occurs after eruption of the second permanent molar, more exaggerated mesial tipping of the second molar can be the expected outcome. Although the premolars undergo the greatest amount of distal drifting, all the teeth anterior to the space, including the central and lateral incisors on the side where the loss occurred, may show evidence of movement. Contacts open and the premolars, in particular, rotate as they fall distally. There is a tendency for the maxillary premolars to move distally in unison, whereas those in the lower arch may move separately. When the maxillary first permanent molar loses its opponent, it erupts at a faster rate than the adjacent teeth. The alveolar process is also carried along with the molars and causes problems when prosthetic replacements are needed. The treatment of patients with the loss of first permanent molars must be approached on an individual basis. A superimposed existing malocclusion, abnormal musculature, or the presence of deleterious oral habits can affect the result, as in the case of the premature loss of primary molars.
If the first permanent molars are removed several years before eruption of the second permanent molars, there is an excellent chance that the second molars will erupt in an acceptable position (Fig. 27-23). However, the axial inclination of the second molars, particularly in the lower arch, may be greater than normal.
When the first permanent molar is lost after the eruption of the second permanent molar, orthodontic evaluation is indicated, and the following points should be considered: Is the child in need of corrective treatment other than in the first permanent molar area? Should the space be maintained for a replacement prosthesis? Should the second molar be moved forward into the area formerly occupied by the first molar? The latter choice is often the more satisfactory, even though there will be a difference in the number of molars in the opposing arch. A third molar can often be removed to compensate for the difference. Without treatment the second molar will tip forward within a matter of weeks (Fig. 27-24).
Another option to consider is autotransplantation of a third molar into the first molar position (Fig. 27-25). According to Bauss and colleagues, autotransplantation has become a well-established treatment modality in cases of early tooth loss or aplasia.17 For third molars with partly developed roots, transplantation success rates have been reported in the range of 74% to 100%.
ORAL HABITS IN CHILDREN
Bruxism
Defined as nonfunctional grinding or gnashing of teeth, bruxism has been reported in up to 15% of children and young adults. Usually occurring at night, bruxism can result in significant abrasion of primary and permanent teeth if continued over a prolonged period (Fig. 27-26). A vinyl bite-guard that covers occlusal surfaces of all teeth can be worn at night to prevent continued abrasion. The occlusal surface of the bite-guard should be flat to avoid occlusal interferences. A mouth guard of the type described in Chapter 22 may also help in overcoming the habit. Ramfjord18 believes occlusal interferences may trigger bruxism if combined with nervous tension. Therefore occlusal equilibration can be used to help the problem if obvious interferences are present. Sheppard19 recommends construction of an anterior bite plate that allows for continued eruption of the posterior teeth if they have been abraded by the habit. When bruxism continues into adulthood, periodontal disease and/or temporomandibular joint disturbances can be a resulting factor.
Digit Sucking Habits
Many children suck their thumbs or fingers for short periods during infancy or early childhood with the habit considered normal during the first 2 years of life. If present at such an early age, parents should be advised to periodically observe the nature and intensity of the habit. If the child demonstrates gradually diminishing activity, it is probable the habit will cease without intervention. Traisman and Traisman20 reported the average age at which digit-sucking stopped was 3.8 years, although other studies indicate a persistent incidence of up to 20% at age 4 years. These studies indicate changes in the anterior occlusion caused by digit-sucking are temporary with little likelihood of long-term effects if the habit is discontinued by age of 3 to 4 years.
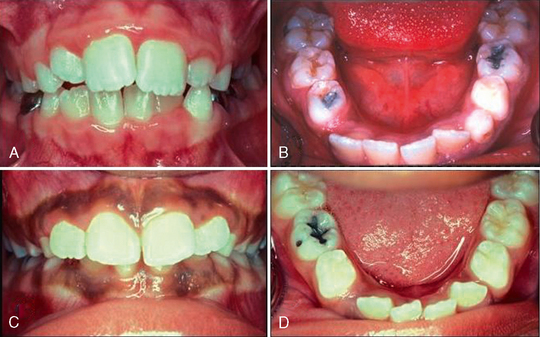
If the intensity of the habit persists or increases and adverse dental and skeletal changes are noted beyond age 4 years, corrective measures may be needed to avoid undesirable occlusion problems (Fig. 27-27). By the age of 6 to 7 years, estimates indicate approximately 10% to 15% of children have a persistent digit-sucking habit that run the gamut from incidental sucking at bedtime to pronounced habits that seems to be almost constant. Almost all authorities recognize persistent digit-sucking habits extending into the incisor transition period can cause a malocclusion or aggravate an already existing one. Pressure generated from the habit can produce changes in the anterior segments of the dental arches with labial flaring and protrusive spacing of maxillary anterior teeth and increased overjet. Remodeling of the maxillary alveolar process and vertical displacement of the maxillary anterior teeth can result in an open-bite relationship. In addition, the digit positioning can interfere with eruption of the lower incisors to exaggerate the open-bite appearance in the incisor segment. Intense patterns may contribute to pronounced lingual inclination of the mandibular incisors that further increases the overjet situation. The increased open-bite and overjet may lead to abnormal muscle activities where the tongue protrudes during swallowing as an adaptation to the anterior space. Subtelny,21,22 in evaluating 34 digit-sucking children using cineradiography, reported that 82% exhibited tongue-thrust activity during swallowing. Dent/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses