Chapter 8
Treatment of a Patient with an Edentulous Mandible with an Immediate Occlusal Loading Protocol (DIEM® 2)
LITERATURE REVIEW
Introduction
Dentistry has moved through a number of evolutions over the last several decades. For many years, treatment of the edentulous mandible using conventional complete dentures was the standard of care for dentistry, even though the term standard of care can have multiple definitions (Feine et al. 2002; Fitzpatrick 2006). Conventional mandibular complete dentures still are frequently made for edentulous patients but often can be frustrating for clinicians and patients due to severe resorption and the resultant instability of mandibular complete dentures (Figures 8.1–8.3).
Rehabilitation of edentulous patients can be accomplished with conventional complete dentures or with implant-supported prostheses (Meijer et al. 2003). Per Carlsson (2010), despite the significant improvements reported by patients regarding retention and stability with implant-supported prostheses, conventional complete dentures remain the most prescribed treatment for such rehabilitation due to economic factors. Even with complete dentures, which partially restore masticatory function compared with implant-supported prostheses, edentulous patients have been reported to expect a better quality of life after treatment completion (Yoshida et al. 2001; Ellis et al. 2007). On the other hand, although the vast majority of the patients using conventional complete dentures have been satisfied with their prostheses, about 10%–20% of these patients have reported that they have not been satisfied, even when the dentures have been clinically acceptable (Carlsson 2006).
Figure 8.1 Preoperative clinical anterior view of a severely resorbed edentulous mandible. Note that the soft tissues of the floor of the mouth are actually superior to the residual ridge.

Figure 8.2 Panoramic radiograph of an edentulous mandible with moderate resorption. Note the density of the edentulous mandible as indicated by the radiopacity of the mandible.

Figure 8.3 Panoramic radiograph of an edentulous mandible with severe resorption. Note that the mental foramen was located very close to the crest of the edentulous jaw. This patient was unable to wear her mandibular denture due to pain with chewing.
In a recent paper (Bekiroglu et al. 2012), the populations of two nursing homes were studied regarding oral complaints of patients 55 years of age or older and their satisfaction with complete or partial dentures. There were a total of 210 potential subjects; 130 (61.9%) took part in the surveys. One hundred five (80%) subjects wore complete dentures; more than one-half of the subjects were older than 75 years of age. Sixty percent of the subjects reported problems for all the variables in the questionnaires. Bekiroglu et al. (2012) concluded that elderly people with dentures, particularly complete dentures, frequently complained of a wide range of problems that included eating, social interaction, and communication. They also concluded that these problems had a detrimental influence on the subjects’ quality of life. In a separate publication, Ribeiro et al. (2012) reported on the effects that Alzheimer’s disease (AD) had on an elderly population and concluded that elderly subjects with AD had poorer oral health than elderly patients without the disease. Despite the positive self-perception of their oral health, the oral health of subjects with AD tended to decline as their disease progressed.
As mentioned earlier, patient expectations may interfere with patient-reported levels of satisfaction regarding prosthetic treatment (Baracat et al. 2011). Clinicians also must take into consideration that important differences among patient expectations and dentist expectations exist (Marachlioglou et al. 2010). This may negatively affect patient/dentist relationships. Appropriate, respectful relationships between patient and dentist have been proven to be important regarding successful responses to treatment (Carlsson 2006; Baracat et al. 2011). Dentists’ understanding of patient expectations prior to treatment regarding the likelihood of success as perceived by patients as well as the potential for success dentally is also important. If the prognosis for successful treatment is verbalized by both parties, both parties will more likely avoid frustrations regarding unrealistic expectations (Marachlioglou et al. 2010).
The Preosseointegration Era
The preosseointegration era was defined by Philip Worthington (2005) as the period where preprosthetic surgical procedures were accomplished to facilitate prosthetic treatment in patients with significant anatomic compromises. The surgical procedures developed in this era were directed towards two goals:
The most durable contribution made during this time related to orthognathic and preprosthetic surgical techniques that eliminated osseous asymmetries that corrected clinical situations prior to denture construction. Conventional prosthodontic treatment resulted in accurately fitting prostheses. However, there were numerous patients who still could not manage their dentures (Carlsson and Omar 2010).
Prior to the advent of osseointegration, patients elected to undergo significant surgical procedures regarding endosseous and/or subperiosteal implants (Figures 8.4–8.6). Many of the surgical procedures (mandibular staple implants; mandibular subperiosteal implant frameworks) included the need for hospitalizations and general anesthesia. It is interesting to note that these surgical procedures were planned for elderly patients who were the least able to undergo such anesthetic procedures.
Figure 8.4 Clinical intraoral image of a patient restored with a cast metal framework that splinted the two oral posts associated with a mandibular staple implant. Note the lack of keratinized tissues on the facial surfaces of the posts.

Figure 8.5 Panoramic radiograph of the patient in Figure 8.5. The implant framework was placed with a submental approach with the patient in a hospital operating room, under general anesthesia.
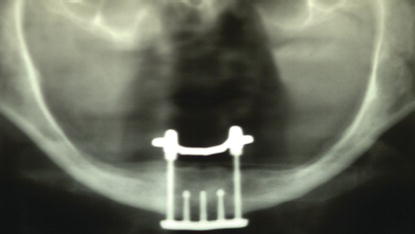
Figure 8.6 Panoramic radiograph of a patient treated with a mandibular subperiosteal implant framework. This implant framework was placed with an intraoral approach with the patient in a hospital operating room, under general anesthesia.

The Osseointegration Era
This era expanded knowledge of bone biology relative to osseous wound healing and its interactions with dental implants and their surfaces. Roughened surfaces and the requirement for minimal micromotion fostered stable implant/bone connections and allowed the creation of fixed implant-retained prostheses. Albrektsson et al. (1986) described the osseointegration era as halfway biotechnology.
Implantology struggled during this period of time with failures and successes. In 1982 at a conference organized in Toronto, Canada, by Dr. George Zarb, dental professionals realized that their interaction and understanding of bone biology was, in fact, progressing and many solid partnerships were being formed.
However, as quoted by Worthington (2005), the Scottish poet, Robert Burns (1971), reminded us it is not always easy to see ourselves as others see us and what perhaps was evolving was that the surgeons looking at themselves might see someone who was innovative, resourceful, and dexterous, whereas their prosthodontic colleagues might see someone who was overconfident, unrealistic, and perhaps ineffective. On the other hand, the prosthodontist might look at himself/herself and see a true artist with the hardest job of all – satisfying patients. His or her surgical colleagues might see prosthodontists as someone who was not only very demanding but also grudging in acknowledgment of the surgical contribution (Worthington 2005) (Figures 8.7 and 8.8).
Figure 8.7 Preoperative clinical image of mandibular anterior teeth with poor long-term prognoses.

Figure 8.8 Immediate postoperative clinical anterior view of the patient in Figure 8.7 after the mandibular teeth were extracted, multiple implants were placed with high insertion torques, and a full-arch, immediate prosthesis was screwed into place.

Brånemark’s protocol (Brånemark et al. 1977) for dental implants included the following:
This strict protocol led to high cumulative survival rates (CSRs) at up to 36 months post implant placement of 90.7% for implants with diameters less than 4 mm, 94.6% for implants with diameters of 4–5 mm, 66.7% for 7 mm long implants, and 96.4% for 16 mm long implants (Winkler et al. 2000).
Brånemark et al. (1983a) divided osseointegration into three phases: primary fixation; callus formation; and remodeling into mature, lamellar bone. Nonintegration of dental implants occurred when this sequence of events was disturbed (Adell et al. 1986). The potential etiologies for nonintegration of dental implants included preparation trauma, infection, premature occlusal loading, and postinsertion occlusal overload of fixed prostheses. However, scientific evidence for premature occlusal loading has been disputed (Testori et al. 2001, 2002; Romanos et al. 2013).
Immediate Occlusal Loading in the Edentulous Mandible
Immediate occlusal loading (IOL) in the edentulous mandible has taken on several different names: DIEM® (Biomet 3i, Palm Beach Gardens, FL, USA) and Teeth in a Day® (Prosthodontics Intermedica, Fort Washington, PA, USA). IOL of multiple, splinted implants with fixed, implant-retained prostheses in the maxillae has also been reported with long-term, high CSRs.
Ostman et al. (2012) reported on the results of a study involving IOL with 112 maxillary and 27 mandibular implants. Forty-two patients were included in the study and were consecutively enrolled. Surgical implant placement requirements consisted of final insertion torques of a least 30 N cm and an implant stability quotient (ISQ) above 55. All of the implants were placed by one investigator, and the majority of these implants (n = 77/55%) were placed in posterior regions and in soft bone (n = 90/65%). A total of 57 prosthetic constructions were evaluated consisting of 20 single-tooth restorations, 30 fixed partial dentures (FPDs), and 7 complete, fixed maxillary restorations. Radiographs were taken at baseline and 12 months postoperatively. Ostman and others reported that of the 139 study implants, one implant failed. The overall CSR at 1 year was 99.4%. Mean marginal bone resorption was 1.01 mm (SD 0.85) during the first year of function. Ostman and others concluded that the study was limited to a short follow-up period; immediate loading with this specific implant type seemed to be a viable option in implant rehabilitation, when insertion torques of at least 30 N cm were achieved. They also concluded that further studies were needed to authenticate the findings of this study.
IOL in the edentulous mandible has been defined as implant placement with adequate primary stability and a fully functional occlusion at the time of implant placement (Schnitman et al. 1997). This definition was specific regarding time and function of the implants (Figure 8.9).
Figure 8.9 Patient with IOL™ Abutments (Biomet 3i, Palm Beach Gardens, FL, USA) in place immediate post implant placement, prior to transfer to the author’s office.
IOL has proven to be predictable when implants were placed with insertional torque values of at least 30 N cm or greater (Testori et al. 2001; Lazzara et al. 2003). This torque value is a quantitative measurement of the force required to place implants into their osteotomies and correlates well with primary stability. Micromotion has been defined as the movement of an implant within an osteotomy. Tarnow et al. (1997) quoted Brunski (1997) as stating micromotion can be deleterious at the bone/implant interface especially if the micromotion occurred soon after implantation. Brunski further stated that micromotion of more than 100 µm should be avoided as motion greater than this level would likely cause the wound to undergo fibrous repair rather than the desired osseous regeneration. Brunski described movement in the range of 50–100 µm as clinically acceptable and would be tolerated by implants and allow osseointegration.
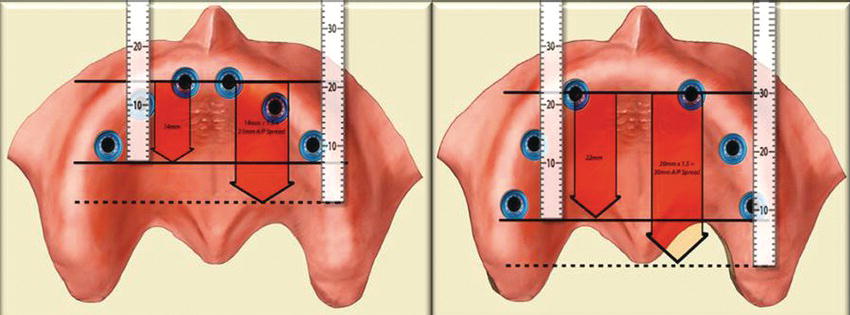
Cross-arch stabilization is accomplished when implants are splinted from one side of the arch to the other. This bilateral arrangement provides biomechanical advantages when connected by rigid prostheses. Cross-arch stabilization is also a function of the anterior/posterior (A/P) spread of implants in a given arch (McAlarney and Stavropoulos 1996). A/P spread is measured by drawing a horizontal line across the most anterior implant and a second horizontal line through the middle of the most posterior implants (Figure 8.10). In a definitive implant-retained prosthesis with a metal framework, the development of a cantilever distal to the last implants may range from 1.5 times the distance to one-half of this distance (English 1992).
Early investigators of IOL of dental implants included Schnitman, Tarnow, and Testori. Schnitman (1997) reported the results of a 10-year study that included sixty-three 3.75 mm diameter machined, cp titanium implants placed in 10 patients followed for 10 years. The 10-year CSR of all implants was 93.4%. The immediately loaded implants had a CSR of 84.7%; the nonloaded implants had a CSR of 100%. Tarnow et al. (1997) completed a 5-year study and reported on the immediate loading of threaded implants in edentulous arches. Six of the patients had edentulous mandibles; four had edentulous maxillae. Fifty-nine implants were immediately loaded; 38 were nonloaded and healed without occlusal function. Fifty-seven of the 59 immediately loaded implants integrated, and 37 of the 38 submerged nonloaded implants integrated. Tarnow and others’ conclusion was that immediate loading of multiple implants rigidly splinted, with cross-arch stabilization, can be a viable treatment option for edentulous patients.
Figure 8.10 Diagrammatic representation of A/P spreads. The image on the left demonstrates an A/P spread of approximately 15 mm; the image on the right demonstrates an A/P spread of approximately 22 mm.
Testori et al. (2001) evaluated the healing of OSSEOTITE® implants with a submerged, traditional unloaded protocol and an immediate loading protocol in a single patient. It was a case report that quantified bone/implant contact surface area for two immediately loaded and one nonloaded implant 8 weeks post implant placement. The case report described the treatment for one patient with 11 implants: 5 were allowed to heal with the traditional protocol and 6 were immediately loaded. Eight weeks post implant placement and IOL, three implants were removed and analyzed for bone implant contact. The two immediately loaded implants had significantly greater bone/implant contact (68%) than the nonloaded implants (34%). IOL of implants did not impede osseointegration and bone remodeling on the OSSEOTITE® surface.
Testori et al. (2003) followed the aforementioned clinical report with a study where six patients received definitive prosthesis in occlusal function within 36 hours of implant placement surgery. All of the implants were clinically successful. Testori et al. (2003) concluded that the treatment of patients with edentulous mandibles with this IOL protocol supported by OSSEOTITE® implants seemed to be a viable option to the traditional nonloading healing protocol. High implant clinical survival rates and minimal bone loss were obtained with the immediate loading protocol immediately or up to a 36-hour period post implant placement. Drago and Lazzara (2006) reported similar findings with IOL of edentulous mandibles 12 months post implant placement. The CSR for the implants was 96.8%; the CSR for the prostheses was 100%.
More recently, Pieri et al. (2009) reported a CSR of 98.6% for 144 mandibular implants placed in 23 patients. The implants were restored with full-arch prostheses (9 maxillary, 15 mandibular) within 48–72 hours post implant placement. All implants were placed into occlusal function immediately post implant placement. Pieri and others concluded that IOL of multiple mandibular implants rigidly splinted together was a viable treatment option when the implants achieved high levels of insertion torque (≥30 N cm).
Immediate Occlusal Loading in Edentulous Maxillae
Edentulous maxillae are different from edentulous mandibles at the microscopic and macroscopic levels. This is particularly true when comparing anterior maxillary jaws with anterior mandibular jaws; maxillary bone is more trabecular and less dense than mandibular bone (Jaffin and Berman 1991; Esposito et al. 1998). In some cases, it is much more difficult to achieve high insertion torque levels at the time of maxillary implant placement. High insertion torque levels are considered to be one of the primary criteria for successful osseointegration of dental implants (Esposito et al. 1998). Implant insertion torques of at least 40 N cm have been recommended as the minimal value acceptable for IOL, although this issue is still being researched (Adrianssens and Hermann 2001).
DIEM® Protocol
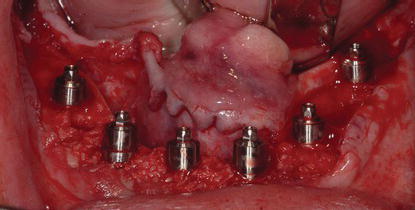
Testori et al. (2003) initiated procedures that became known as the DIEM® protocol (Biomet 3i, Palm Beach Gardens, FL, USA). The protocol included placement of at least four implants into edentulous mandibles, with insertional torque values of at least 30 N cm. The implants would be restored with a screw-retained prosthesis on the same day. Implant restorative components were developed to facilitate fabrication of this type of prosthesis. The protocol provided patients with fixed, screw-retained implant prostheses, with fully functional occlusions on the day of implant placement. The protocol could be adapted for dentulous patients with hopeless dentitions, where the teeth were extracted on the day of implant placement (Figures 8.11–8.13), as well as edentulous patients who were unable to manage complete dentures (Figures 8.14–8.16).
This type of treatment clearly requires a team concept for restorative dentists, implant surgeons, and laboratory technicians. This protocol was restoratively driven but surgically determined in that all of the criteria for IOL have to be satisfied prior to loading the implants with full-arch prostheses on the day of implant placement. If one or more of the criteria were not satisfied, implants would be placed and not loaded, or grafting may be required prior to implant placement at a later date. Restorative dentists had the role of coordinating treatment logistics. Extensive preoperative treatment planning was necessary to determine such details as to whether the patient will be treated at the surgical and restorative offices on the same day or whether the procedures will be extended to occur over a 36-hour period and patients would be treated in the surgical office and then, the next day, in the restorative office.
Figure 8.11 Preoperative clinical image of a patient with a hopeless dentition secondary to dental caries.

Figure 8.12 Postoperative clinical image of the patient in Figure 8.11 one week after extraction of the remaining teeth, multiple implant placement with high primary stability, and insertion of maxillary and mandibular full-arch prostheses.

Figure 8.13 Postoperative clinical image of the patient in Figures 8.11 one week after the aforementioned procedures were accomplished.

Figure 8.14 Preoperative clinical image of a patient with a maxillary complete denture that she was no longer capable of managing without significant amounts of denture adhesive on a daily basis.

Figure 8.15 Postoperative clinical image of the patient in Figure 8.14 one week after multiple implants were placed with high primary stability. The implants were restored with a full-arch, immediately occlusal loaded, screw-retained prosthesis.

Figure 8.16 Postoperative clinical image of the patient in Figure 8.14 one week after the aforementioned procedures were accomplished.

DIEM®2 Protocol
Over the past several years, numerous reports have been published regarding treatment of patients with edentulous maxillae with dental implants, IOL, and full-arch, fixed prostheses (Balshi et al. 2005; Calandriello and Tomatis 2005; Malo et al. 2005; Capelli et al. 2007; Testori et al. 2008). The studies reported using straight, vertical, and tilted implants. Tilted maxillary implants have one distinct advantage over using multiple vertical implants in the posterior maxillary segments – grafting of maxillary sinuses are generally avoided. This nongrafted solution typically saves patients surgical procedures, surgical morbidity, and costs.
Romanos and Nentwig (2009) reported the results of a 5-year clinical study regarding maxillary implants and full-arch, immediately loaded prostheses. Ninety implants were placed (6 in each arch) for 15 patients. The implants were immediately loaded with full-arch, acrylic resin prostheses. The implants were loaded for a mean of 42.4 months; Romanos and Nentwig reported three implant failures. The CSR was 96.7%. The authors concluded that with this protocol, IOL for maxillary edentulous jaws can be used successfully when implant primary stability, cross-arch stabilization, and soft diets are used during initial healing.
The DIEM®2 protocol calls for the placement of a sufficient number of implants to satisfactorily retain full-arch, fixed prostheses immediately after implant placement. Four, six, or more implants may be used to retain the fixed prostheses. Implant number will depend on the quality of the bone, the A/P spread, the insertion torque, the opposing dentition, and the presence or absence of parafunctional habits.
Prosthetic and clinical factors involved in treatment planning include:
- Vertical dimension of occlusion (VDO)
- Lip support, incisal display at rest, speaking, smiling, lip mobility, and the resulting transition zone
- Interarch distance
- Condition of the preexisting dentures
- Skeletal/dental malocclusion
- Temporomandibular joint health/disease
Treatment indications for immediate, full-arch prostheses include:
- Adequate bone quality equal to or greater than Type III
- Adequate bone volume for implant placement
- Adequate restorative volume that will provide adequate space for implant restorative components and prostheses
- Adequate A/P spread for optimal implant positions and decreased cantilevers (Figure 8.17)
Contraindications for IOL include:
- Systemic, uncontrolled diseases
- Uncontrolled, parafunctional habits (bruxism)
- Poor bone quality (Type IV)
- Lack of bone quantity
- Limited A/P spread (Figure 8.18)
Figure 8.17 Laboratory occlusal image that demonstrates a satisfactory A/P spread with 4 maxillary implants. The large A/P spread resulted in minimal posterior cantilevered segments.

Figure 8.18 Clinical occlusal image of a patient that demonstrates a poor A/P spread with 4 mandibular implants. This short A/P spread would likely result in either longer cantilevered posterior segments on a fixed prosthesis, or the patient could elect to be treated with a bar splinting the implants and a mandibular overdenture.

CLINICAL CASE PRESENTATION
Appointment 1: Initial Examination
Dr. Carpentieri performed both the surgical and prosthodontic procedures for this patient.
This patient was self-referred. The receptionist at the front desk sent this patient a personal letter welcoming her to the practice prior to the initial examination appointment. This letter introduced the entire staff to the patient and also discussed the philosophy of the practice. Once the patient arrived at the office, the receptionists introduced themselves in person and again welcomed the patient to the practice.
The implant treatment coordinator re-explained what would be accomplished at this visit; the initial visit would last approximately 60 minutes, and this visit was one of potentially two diagnostic visits in the treatment process. The patient was also asked to bring a family member or individual to accompany them at any future appointments.
Chief Complaint
A 68-year-old female presented for evaluation. The patient’s chief complaint was, “I can’t wear my upper denture anymore. My lower teeth hurt, are loose and some of them are broken. I don’t want to wear a lower denture.” The medical and dental histories with all medications were recorded.
Radiographs
Conventional digital panoramic and periapical radiographs were taken at this time (Figures 8.19 and 8.20).
Figure 8.19 Preoperative panoramic radiograph that demonstrated moderate to advanced bone loss throughout the mandibular dentition.

Figure 8.20 Preoperative periapical series of radiographs that demonstrated moderate to advanced bone loss throughout the mandibular dentition.
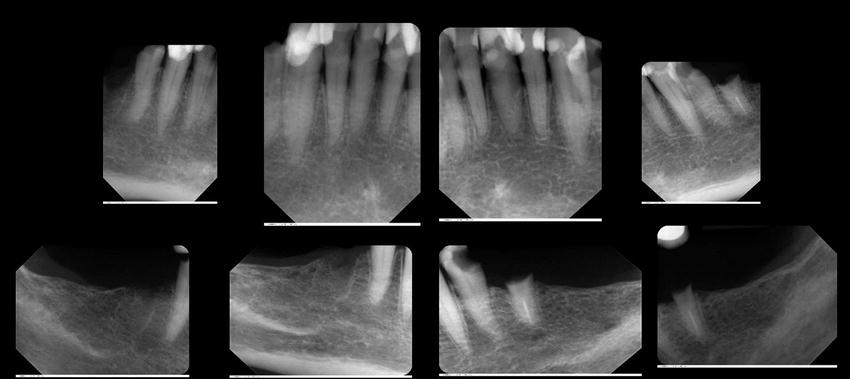
Figure 8.21 Preoperative clinical anterior image of the patient in an approximate vertical dimension of rest position. There was a skeletal Class I relationship between the edentulous maxillae and partially edentulous mandible.

Physical Examination
Extra- and intraoral physical examinations were completed including periodontal pocket measurements and tooth mobility (Figures 8.21–8.25). Measurement of the patient’s ability to open to allow access with the drills at potential implant sites was recorded with a long Castroviejo caliper (Ace Surgical Supply Co., Inc., Brockton, MA, USA) (Figure 8.26). The bone and tissue thicknesses were approximated and recorded with Boley gauge calipers (Boley Gauge, Ace Surgical Co., Brockton, MA, USA) at the same sites (Figure 8.27).
Figure 8.22 Preoperative clinical anterior image of the patient with the maxillary denture in place, in centric occlusion.

The maxillary denture was not retentive and unstable right to left and anterior to posterior. It lacked satisfactory distal buccal seals. The edentulous ridge was broad and U-shaped. The ridge was covered with pink, fixed, keratinized soft tissues. The edentulous ridge height was satisfactory. She had a normal palatal vault without any tori. There were no soft tissue lesions; she had adequate and apparently normal saliva.
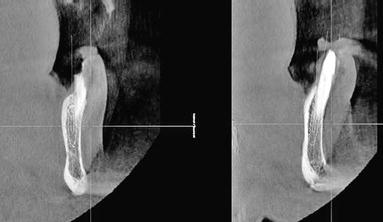
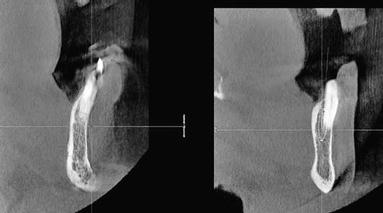
The patient proceeded with the complete, definitive examination, which included three-dimensional (3D), computed tomography (CT) (Figures 8.28 and 8.29). Conventional and CT radiography demonstrated at least 50% horizontal bone loss around the mandibular teeth. There were multiple instances of recurrent caries and large, preexisting restorations. The mandibular left second premolar (#20) was missing most of its clinical crown.
Figure 8.23 Close-up, preoperative clinical anterior image of the mandibular anterior teeth. The incisal edges demonstrated moderate incisal wear; there were multiple restorations and gingival recession.

Figure 8.24 Preoperative clinical, occlusal anterior image of the remaining mandibular teeth.

Figure 8.25 Preoperative clinical image of the patient in rest position.

Figure 8.26 Castroviejo caliper used to measure the amountof interocclusal distance available for osteotomy andimplant placement.
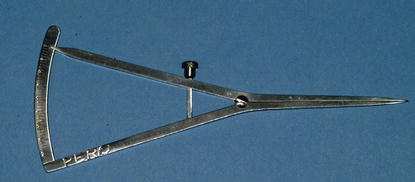
Figure 8.27 Boley gauge used to measure the preoperative width of the alveolus.

Figure 8.28 Cross-sectional oblique CT images; these images demonstrated horizontal bone loss and adequate implant bone volume for placement of implants immediately post extraction without the need for bone grafting procedures.
Diagnoses
Figure 8.29 Cross-sectional oblique CT images; these images demonstrated horizontal bone loss and adequate implant bone volume for placement of implants immediately post extraction without the need for bone grafting procedures.
Prognosis
Deterioration of the dentition was projected to continue, and the patient agreed that the dentition would require a significant effort to restore. Multiple treatment plans were discussed including periodontal surgery, endodontics, crowns, FPDs and removable partial dentures (RPDs), complete dentures, overdentures, and dental implants with and without IOL. The patient’s lack of commitment to maintain reasonable oral hygiene, the cost to replace and restore the remaining teeth, and the potential for recurrent caries and periodontal disease were beyond her means and desires. Maintenance of the natural dentition would likely require additional costly treatment in the future; the prognosis considering her care and retention of the restored dentition was extremely poor. The patient was still faced with continuing to wear a mandibular RPD.
She was interested in the concept of extraction, implant placement, and IOL. She was pleased that this would include elimination of a mandibular removable prosthesis. The prognoses for extractions, alveolectomy, implant placement, and IOL for a mandibular fixed implant-retained prosthesis and a complete maxillary denture were favorable, and she accepted it as her treatment option. The costs over the long term were figured to be less than the treatment option that included maintenance of her natural dentition. The implant treatment plan would likely provide better function, aesthetics, and phonetics on a long-term basis. The interest and commitment to proceed expressed by the patient resulted in completion of the radiographic examinations, which included a CT of the mandible. The patient was discharged to return for the definitive consultation and presentation of written treatment plan options.
Appointment 2: Consultation with Patient (1 Hour)
Treatment Options
The first treatment option included a new maxillary complete denture, extraction of the mandibular teeth, alveolectomy to provide the requisite restorative volume, implant placement with insertion torque values of at least 50 N cm, and then an immediate, full-arch prosthesis per an IOL protocol. The patient did not have enough bone volume posteriorly to consider vertical implant placement; she also did not have enough space between the mental foramen for five vertical implants. The author (JC) decided to use a tilted implant protocol for the posterior implants and a vertical implant protocol for the two anterior implants. Angled abutments were to be used to facilitate the prosthetic procedures for the posterior tilted implants. It was expected that the implants would achieve insertion torques of at least 50 N cm in the anterior mandible. This was the author’s baseline to consider immediate loading for the mandibular full-arch prosthesis. After osseointegration occurred, a definitive mandibular prosthesis would be fabricated with a computer-aided design and computer-aided manufacturing (CADCAM) framework (Table 8.1).
The second treatment option described the extraction of the remaining teeth and replacement with a mandibular, immediate complete denture and a new maxillary complete denture. If the denture experience was unsatisfactory, implants could be considered at a later date for increased retention and stability of one or both dentures (Chao et al. 1995; Awad et al. 2003) (Table 8.2).
The third treatment option deferred any or all prosthetic treatments at this time (Table 8.3).
Benefits and limitations of each treatment option were described in detail on the written treatment plans. The surgical and prosthodontic fees or ranges of fees for each procedure were also listed on each treatment plan. Those fees will not be listed here. The patient was given copies of the treatment plans, and after some consideration, the patient agreed to proceed with the first treatment plan including implant placement and insertion of a fixed implant-retained prosthesis on the same da/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


