Chapter 8
The Restorability of Broken Down Teeth: the Decision-making Process
Aim
To discuss the factors which must be considered when assessing the restorability and managing the restoration of severely compromised teeth.
Outcome
At the end of this chapter, the reader should be able to make the decision when to restore the compromised tooth, and when to extract and consider options for replacement.
Objectives of Restoring a Severely Compromised Tooth
-
To promote tooth survival.
-
To restore pain-free function.
-
To protect the remaining tooth structure against further carious and non-carious tissue loss.
-
To provide occlusal stability and proximal contacts with adjacent teeth.
-
To provide optimal aesthetics.
-
To promote health in the marginal periodontal tissues.
-
To promote periapical health.
Following completion of the restorative treatment, the tooth should be able to withstand functional loads. The prognosis of the tooth is affected by a number of factors including the quality of the root canal treatment, the quality and quantity of the remaining coronal tooth structure, the avoidance of iatrogenic accidents such as perforation during post-space preparation, and the physical characteristics and fit of the core and the definitive restoration (Fig 8-1).
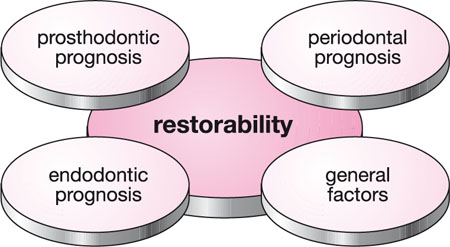
Fig 8-1 Factors affecting the restorability of a root canal treated tooth.
Restoration of Compromised Teeth
Optimal restorative management of the compromised tooth can only be achieved by making a systematic and thorough assessment of the tooth, within the context of the dentition, the supporting structures and the patient as a whole.
By completing a thorough clinical and radiographic examination, the restorability and overall prognosis of the tooth can be determined. These findings can then be presented to the patient, enabling an informed decision on the best way forward, based on the patient’s expectations, motivation, time and financial constraints. The ultimate decision to restore or extract a severely compromised tooth must be dictated by informed patient choice. It is the responsibility of the dental professional to advise the patient of the treatment options, their relative prognosis and cost.
Many of the factors that are important in deciding whether or not to restore a tooth are also important when considering options for replacement if the tooth is lost. In addition, the status of the neighbouring teeth may be a very important consideration in deciding the best option for the patient.
Of course, every patient is different and this must be appreciated when treatment planning decisions are made. There are some patients who may be willing to go to almost any length in the hope of holding on to a tooth, even if the prognosis is acknowledged to be guarded. Alternatively, some patients may be reluctant to embark on any complex work, or wish only to invest in options which they consider to be predictable.
The discussions and the consent to proceed with a particular option should be recorded in the patient’s notes. Written consent may be considered necessary in some instances.
Prognosis
Determining the prognosis of a tooth to be restored necessitates that a number of factors are considered, including the:
-
Prosthodontic prognosis
-
Periodontal prognosis
-
Endodontic prognosis
-
Relevant general factors.
Prosthodontic Prognosis
Key considerations include the:
-
remaining sound coronal tooth structure
-
presence or absence of fractures
-
need to crown the tooth to protect against fracture
-
ability to develop coronal seal
-
ability to obtain ferrule protection
-
occlusal factors
-
ability to obtain satisfactory aesthetics.
Remaining Coronal Tooth Structure
The single most important factor influencing the prosthodontic prognosis is the amount of remaining sound coronal tooth structure. This tooth substance provides retention, resistance and a substrate for adhesion between the tooth and the restoration.
To assess the prognosis of a tooth, all restorations and any residual caries must be removed to allow inspection of the remaining tooth structure. A decision regarding the presence of adequate restorable coronal tooth structure can only be made once all the relevant information has been collected and carefully considered.
Presence of Fractures
The detection of any fractures in the remaining tooth structure is of paramount importance. A fracture may have a massive impact on the prognosis of the tooth. In addition to being a point of weakness in the tooth, fractures are a potential pathway for bacterial ingress into the root canal system and the marginal periodontium. Hence, a fracture can contribute to prosthodontic, periodontal and endodontic failure.
A fracture can be either complete or incomplete. Complete fractures are by definition obvious. Identifying incomplete fractures can be a diagnostic challenge. Fractures can be classified according to their location in the tooth:
-
crown fracture – with or without pulpal involvement
-
combined crown/root fracture
-
isolated root fracture.
Crown Fracture
Crown fractures are seen fairly commonly, and may present in either restored or unrestored teeth. The clinical presentation may be as subtle as some crazing of the enamel, and as obvious as complete fracture and separation of a cusp or tooth wall. Teeth which have been heavily filled or root canal treated are more prone to developing fractures, but catastrophic fractures are occasionally seen in the sound, intact teeth of patients who parafunction. Some teeth may exhibit several fracture lines in different planes, in particular around a large restoration. Fractures can be considered as oblique or vertical in orientation. Vertical fractures usually present in a mesiodistal plane, running from one marginal ridge to another. Oblique fractures tend to occur at the fulcrum point adjacent to the base of a restoration. Vertical fractures may be more likely to result in an unrestorable outcome than other types of fracture.
There is an increased risk of developing tooth fractures with age. This may be related to the cumulative effects of caries, restorative intervention, and continued cyclical loading over years of function. A change in the composition and structure of dentine with age may also play some role in the development of fractures. Impact trauma may be an additional cause in a number of tooth fractures.
The diagnosis of a fractured tooth can, at times, be difficult, as the patient may complain of vague and poorly localised symptoms. The site, depth and completeness of a fracture is probably critical in dictating the type and level of pain. It is important to remember that the symptoms may be very different for fractures between vital and non-vital or root canal treated teeth. The symptoms experienced in fractured vital teeth are related to the effects of hydrodynamic fluid movement in the dentinal tubules and pulp. These pulpal symptoms will obviously not occur in teeth with non-vital pulps. Fractures in root canal treated teeth may only cause symptoms at a late stage, or if the fracture involves the root canal system or periodontal ligament.
Some of the key clinical features of fractured teeth are listed below, together with some clinical investigations which may be used to aid in the diagnosis of a root fracture (Fig 8-2).
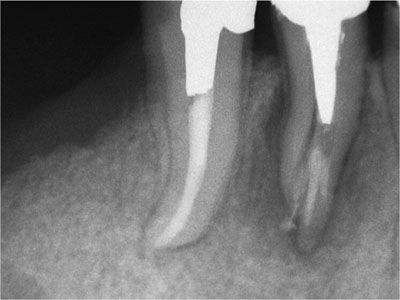
Fig 8-2 A root fracture in a mandibular first premolar restored using a cast post and crown.
Crown Fracture
Symptoms
-
pain may be poorly localised or vague
-
pain on biting, normally short-lived in duration
-
sensitivity to thermal stimuli, usually cold
-
symptoms of pulpitis may develop with time
-
root canal treated teeth may have few or no symptoms.
Clinical features
-
fracture may be oblique or vertical
-
heavily restored teeth may be more susceptible
-
fracture may be more evident in patients who parafunction
-
fracture may not be visible on outer surface of tooth
-
crazing of the enamel
-
clearly demarcated and stained fracture lines
-
tenderness to percussion of individual cusps
-
pain on release after biting on cotton wool or Tooth Slooth/Frac Finder
-
possible increased response to thermal pulp testing, usually cold.
Diagnosis
Clinical
-
direct visualisation – may be aided with magnification
-
removal of restoration to allow clear inspection of cavity
-
transillumination – light will not cross an air-filled gap
-
application of indicator dyes such as methylene blue
-
individual percussion of cusps
-
cotton wool roll, pain may be caused on release after biting
-
symptom reproducers, e.g. Tooth Slooth
-
thermal vitality testing, usually cold, e.g. Endofrost.
Radiographic
-
unlikely to prove conclusive for coronal fractures alone
-
extensive buccolingual fracture may be detected
-
may be more important in excluding other causes of pain.
Management
Probably the two most important considerations when dealing with a fractured tooth are, to what extent the fracture will influence the restorability of the tooth, and whether the fracture extends to involve the pulp.
A supragingival fracture should not affect the prognosis significantly, unless there is a severe lack of coronal tooth structure. Restoration may be as simple as an adhesive cusp replacement restoration. Conversely, a subgingival fracture may render the tooth unrestorable, unless crown lengthening or rapid orthodontic extrusion are possible.
Pulpal involvement of the fracture will necessitate root canal treatment prior to definitive restoration. It is important, however, to establish that the fracture does not extend through the floor of the pulp chamber or into the root canals. Teeth which present with fractures which involve the floor of the pulp chamber or root canals have an uncertain prognosis. It may be impossible to tell whether the fracture is incomplete or complete and, hence, ensuring a bacterial seal with the root canal treatment cannot be achieved predictably. Even in those instances where the root fracture is incomplete on access, there is a very high possibility of propagating the fracture while carrying out the endodontic treatment. As a result, patients should be advised that teeth demonstrating fractures involving the pulp carry a poor or hopeless prognosis.
Root Fracture
Root fracture can occur as a continuation of a coronal fracture or in isolation. Once a fracture involves the periodontal ligament, the nature and severity of the patient’s symptoms may change significantly (see below). The patient is more likely to complain of increased pain on biting, and this will generally be more easily localised and diagnosed. Unfortunately, periodontal ligament involvement of a fracture is an indicator of poor prognosis.
The causes of root fracture are the same as those that cause coronal fracture (i.e. physiological and pathological stresses), and teeth that have been root canal treated and restored with a post are most susceptible to root fracture. Post-restored teeth that are involved in excursive movements are especially at risk of fracture as a result of laterally applied loads. The iatrogenic causes of root fracture include root canal preparation and obturation, post cementation and post removal.
Root Fracture
Symptoms
-
mild to moderate pain
-
pain on mastication
-
increased mobility
-
sinus tract or swelling.
Clinical features
-
typically seen in susceptible teeth, e.g. post-crowned teeth
-
osseous defect adjacent to the fracture
-
periodontal pocketing, classically a localised deep periodontal pocket not consistent with the general periodontal condition. Typically located bucally
-
possible tenderness to percussion. More prolonged than that seen in crown fracture
-
buccal or lingual tenderness to palpation
-
sinus tract formation, soft-tissue swelling or erythema
-
if present, a sinus tract is usually more coronal than typically seen with periapical disease; often coronal to the mucogingival junction
-
increased mobility may be observed.
Clinical diagnosis
-
direct visualisation, may be aided by gently probing and pulling back the gingivae adjacent to the fracture
-
surgical visualisation
-
identification of localised osseous defect
-
direct visualisation of fracture line.
Radiographic diagnosis
-
about 30% of root fractures can be diagnosed radiographically
-
at least two different horizontally angled radiographs should be taken to aid diagnosis.
Key radiographic features include:
-
hair-like fracture lines which may be detected in the dentine body
-
separation of tooth fragments
-
classical “halo” or J-shaped radiolucency, with bone loss around the peri-apex and continuous with the lateral root surface (Fig 8-2)
-
bone loss on the lateral root surface similar to that of a periodontal defect.
Management
-
fractured roots usually require extraction
-
root resection may be possible in certain multi-rooted teeth.
Protection against Fracture
Clinical studies on the restoration of root canal treated teeth have shown that anterior teeth do not necessarily need to be restored with a crown. Even quite extensive loss of proximal tissue in addition to the endodontic access does not necessarily weaken the tooth to the extent to warrant a crown. In fact, there is evidence to suggest that the tissue loss associated with crown preparation in such circumstances may irreversibly weaken the residual tooth substance to a damaging extent, predisposing to failure.
In the case of endodontically treated posterior teeth, the current best evidence indicates significantly longer tooth survival subsequent to the provision of a partial or full coverage cast restoration (Fig 8-3).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


