Chapter 6
Understanding the Failure of Adhesive Restorations in Root Canal Treated Teeth
Aim
To describe the causes of failure of adhesive restorations in root canal treated teeth.
Outcome
At the end of this chapter, the reader should be able to understand the reasons why adhesive restorations fail in root canal treated teeth, and know how to predictably re-restore them.
Failures
Post-core Decementation
-
Decementation is the primary cause of restoration failure in teeth restored with fibre posts, composite cores and metal-ceramic crowns. This is caused mainly by the degradation of the dentine-composite bond under the influence of function and components of the oral environment. When fibre posts make any contact with oral fluids, their flexural strength is greatly reduced, and this combined with cyclic loading plays an important part in causing the post-core decementation. Post-core decementation is often associated with secondary caries (Fig 6-1).
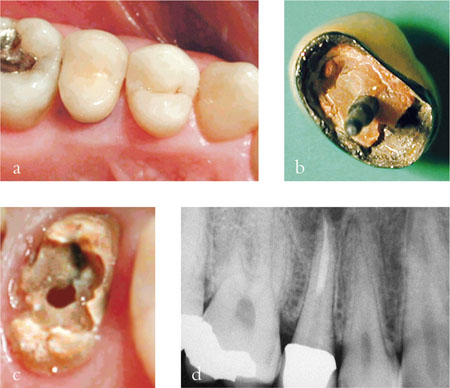
Fig 6-1 Post-core decementation associated with secondary caries (b–c) and a periapical radiolucency (d).
How to minimise the risks of post-core decementation
-
Carefully evaluate the amount of tooth structure available, considering also the amount of tooth structure that will be lost as a result of any subsequent crown preparation. A lack of coronal tooth structure available for bonding is one of the main causes of decementation.
-
Carefully consider if a crown is indicated or not. Research has shown that in anterior teeth, crowning may not increase the likelihood of tooth survival (see Chapter 3). Research has also shown that decementation of the post is highly unlikely to happen if the tooth has not been prepared for a crown. In short, in anterior teeth, post placement and crowning is indicated only if a complete loss of crown tooth structure is present, or if the aesthetic requirements of the patient cannot be met otherwise.
-
The presence of bruxism or other parafunctions may cause failure of post-core restorations. Night guards may be of some help, but the patient needs to be aware that all restorations are at risk of failure when subjected to parafunctions.
-
Preserve as much coronal tooth tissue as possible.
-
Ensure that a proper ferrule has been developed.
-
Ensure that the maximum possible length of the post-space preparation has been created, without risking root perforation or compromising the seal of the root canal filling.
-
Choose the appropriate post size.
-
Isolate the tooth with a rubber dam for moisture control and optimal bonding to dentine.
-
Remove all the remnants of gutta-percha and sealer from the root canal space using an endodontic explorer, under magnification, to optimise the dentinal surface available for the bonding.
-
Rinse the canal with absolute alcohol to sequester any residual eugenol if eugenol-containing materials have been employed.
-
Use a customised post-core if a significant discrepancy exists between the morphology of the root canals and that of the post (see Chapter 5).
Procedure for the management of post-core decementations
Carefully evaluate if the tooth is re-restorable – see Chapter 8 for the decision-making process on the restorability of root canal treated teeth. If the tooth is re-restorable, the best option would normally be to make a new fibre post and composite core before constructing a new crown. If it is agreed with the patient not to start again, it may be possible to simply recement the post-core and crown as follows:
-
Working with magnification and ultrasound, carefully remove all remnants of composite and bonding agent from the root canal.
-
Attempt to reposition the post-crown, checking its marginal adaptation and occlusal relationships.
-
If the post-crown appears satisfactory, isolate the tooth.
-
Etch the root canal for 40 s.
-
Introduce a dual curing, self-etching priming composite cement into the root canal and onto the post (Fig 6-2).
-
Introduce the post-crown into the root canal.
-
Carefully remove any excess composite cement before it is fully cured.
-
Carefully adjust the occlusion.

Fig 6-2 (a) A resin cement capsule featuring a special tip for the insertion of the composite cement into the root canal. The capsule needs to be activated (b), mixed for 15–20 s (c) and inserted into the gun (d). The cement is then applied into the root canal.
Detachment of the Composite Core-crown
Detachment of the composite core-crown from the post is a very rare complication. This may happen when no coronal tooth structure is/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


