8
Special Needs Patients
Case 1
Trisomy 21 (Down Syndrome)/New Patient
A. Presenting Patient
- 6-year-, 6-month-old, African-American male
- Diagnosed with Trisomy 21 (Down syndrome) (see Background Information 1)
- New patient visit
- Trisomy 21 consists of a characteristic group of cognitive and physical findings that result from having an extra copy of chromosome 21.
- Most individuals with Trisomy 21 function in the range of mild to moderate intellectual disability.
- Craniofacial characteristics include:
- Hypoplastic midface and maxilla
- Mild microcephaly
- Upslanting palpebral fissures
- Short neck
- Health conditions frequently seen in individuals with Trisomy 21 include:
- Congenital heart disease
- Hypotonia
- Compromised immune function
- Hearing problems
- Thyroid dysfunction
- Skeletal abnormalities
- Eye problems, especially cataracts
- Increased risk for development of leukemia
- Early development of senile dementia
National Institute of Child Health and Human Development (2007)
B. Chief Complaint
- Mother states, “My son has been to other dentists, but they were not able to take care of him”
C. Social History
- Patient attends school; in class for children with special educational needs
- Mother is primary caregiver
- Lower mid-level socio-economic status
- Patient has two sisters, ages 8 and 11
D. Medical History
- Cardiac: Ebstein’s anomaly (congenital defect of tricuspid valve). Patient’s defect is mild and has not required surgical repair. He is not currently on any medications and is followed by pediatric cardiology on an outpatient basis (see Fundamental Point 1).
- History of frequent otitis media and upper respiratory infections.
- Patient was hospitalized at age 3 for myringotomy and placement of tympanostomy tubes. Due to post-operative complications, patient was required to stay in the hospital for three days post-operatively.
- It has been estimated that the frequency of congenital cardiac defects in individuals with Trisomy 21 is 40% to 50%.
- A medical history should include questions on (Freeman et al. 1998):
- History of cardiac problems
- Symptoms of cardiac problems
- Any surgeries for cardiac problems
- Medications for cardiac problems
- Restrictions on activities
- Due to anatomic variations and compromised immune systems, individuals with Trisomy 21 are at increased risk for upper airway infections.
Mitchell, Call, and Kelly (2003)
E. Medical Consult
- Cardiology consult requested. Patient cleared for routine dental treatment. Antibiotic prophylaxis not required.
F. Dental History
- Mother has taken patient to three other dentists, but she was dissatisfied with care provided.
- Patient’s behavior was uncooperative for previous dental examinations.
- Optimal water fluoridation levels
- Patient is not a frequent snack eater, but does drink large amounts of sugary beverages.
- Patient does not brush teeth himself. Allows mother to brush his teeth under duress.
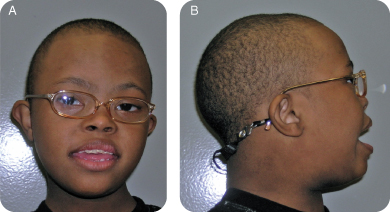
G. Extra-oral Exam (Figures 8.1.1 a–b)
- Patient has characteristic facies of Trisomy 21, as discussed in the background information.
- No other significant findings
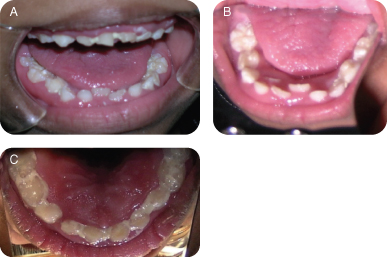
H. Intra-oral Exam (Figures 8.1.2 a–c and Fundamental Point 2)
- Early mixed dentition
- Erupting mandibular central incisors
- Poor oral hygiene
- Generalized marginal gingival inflammation
- Caries-free dentition
- Occlusion: class III skeletal relationship, mesial step primary molars
Figure 8.1.2a–c. Intra-oral photos showing generalized marginal gingival inflammation.
- Individuals with Trisomy 21 may present with a number of oral-facial abnormalities and dental anomalies. These include:
- Class III malocclusion (due to maxillary hypoplasia)
- Relative macroglossia due to the small size of the oral cavity
- Delayed dental eruption
- Hypodontia
- Microdontia and other anatomic anomalies of teeth
- Ectopic eruption and impaction of teeth
- Increased risk for periodontal disease (due to compromised immune response)
Pilcher (1998), Shaw and Saxby (1986), Yavuzyilmaz et al. (1993)
I. Diagnostic Tools
- Radiographs were not obtained for the following reasons:
- Patient was unable to cooperate for radiographic exam
- No caries were noted
- It was determined that the patient would require sedation for radiographic exam; due to absence of caries and the patient’s past history of post-anesthesia complications, the practitioner did not feel sedation presented an appropriate risk/benefit balance for this patient at this time (see Fundamental Point 3).
- Individuals with Trisomy 21 show an increased incidence of the following anatomic variations/medical conditions, which may place them at an increased risk for complications associated with sedation and general anesthesia:
- Congenital heart defects
- Small naso-pharyngeal complex
- Increased incidence of airway anomalies, including laryngomalacia, tracheomalacia, bronchomalacia
- Increased incidence of cervical spine instability
- Obesity
- Hypotonia
- Obstructive apnea
- A careful risk/benefit analysis should be conducted for each child with Trisomy 21 who is being considered for treatment under sedation or general anesthesia.
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List
Diagnosis
- Trisomy 21
- Congenital heart defect (triscuspid valve prolapse)
- Frequent otitis media
- Gingivitis
- Poor oral hygiene
- Malocclusion
Problem List
- High caries risk due to special needs status, high intake of sugared beverages, and poor oral hygiene
- Lack of a dental home
- Increased risk for periodontal disease due to poor oral hygiene and compromised immunity
- Increased risk for ectopic eruption or impaction of teeth, especially in maxillary arch (due to maxillary hypoplasia)
L. Comprehensive Treatment Plan (see Fundamental Point 4)
- Establish a dental home
- Dental prophylaxis and topical fluoride
- Encourage parent to reduce sugared beverage intake
- Encourage improved oral hygiene, (in this case, with parent) focusing on brushing and flossing
- Three-month recall
- Re-evaluate caries risk
- Re-evaluate oral hygiene status
- Monitor eruption of permanent dentition
- Re-evaluate patient’s ability to cooperate for radiographic exam. If cooperative, take radiographs to evaluate for interproximal caries and development of permanent dentition.
- Caries risk: Use the American Academy of Pediatric Dentistry Caries Assessment Tool (CAT) in assigning a patient’s risk category AAPD (2011–2012)
- Periodontal disease: Onset of periodontal disease in individuals with Trisomy 21 is frequently seen by the late teen years. Incidence in some adult populations has been reported to be over 90%. This is probably due to the reduced immune response in these people. Early, aggressive therapy, including frequent cleanings and possible systemic antibiotic therapy, should be considered.
- Malocclusion, ectopic eruption, impactions:
- The class III malocclusion seen in Trisomy 21 involves midface hypoplasia, and would, in most cases, require extensive surgical procedures to correct.
- Patients should be monitored for dental crowding, ectopia, and impactions. These problems may be correctable with orthodontic and minor oral surgical treatment.
Pilcher (1998)
M. Prognosis and Discussion
- There have been reports that individuals with Trisomy 21 have a lower incidence of dental caries than the general population. However, they do experience caries and this patient’s high intake of sugary beverages and poor oral hygiene increases his risk for caries. Dietary modifications and increased recall visits including topical fluoride treatments should reduce this patient’s caries risk.
- This patient is at high risk for development of periodontal disease due to a combination of compromised immune response and poor oral hygiene. Improved oral hygiene and increased recall visits, including prophylaxis and monitoring for periodontal problems, may help improve this patient’s periodontal prognosis.
- Behavioral capabilities, both in the dental setting and at home, are always a consideration when treating children with intellectual disabilities. There is a wide range of behaviors in children with Trisomy 21, and many of them are treatable for routine dental care with little or no modifications in care necessary. Diagnostic exams for this particular patient were compromised by the fact that he has, up to now, been uncooperative for radiographs. An oral examination, prophylaxis, and fluoride varnish treatment were made possible with the mother’s assistance, holding her child in the dental chair. Tell-show-do was used with limited effectiveness. As per the mother’s report, the child’s behavior also makes it difficult for her to accomplish adequate oral hygiene at home. An attempt was made to keep the dental visit as atraumatic as possible, and it is possible that, in the future, the child may become more cooperative. As discussed earlier, these children are at an increased risk for complications related to sedation and general anesthesia, and careful consideration must be made for each individual as to whether or not an anesthetic procedure is warranted for routine diagnostic and dental procedures.
N. Complications and Alternative Treatment Plan
- If this patient had clinically detectable caries, would the behavior management techniques previously used be adequate to accomplish needed treatment?
- If this child had cervical spine (atlanto-axial) instability, how might the practitioner need to modify the way in which dental care was delivered?
- Would there be any differences in this child’s orthodontic care at this age if his behavior was cooperative?
Self-study Questions
1. What are some systemic findings in children with Trisomy 21 that could significantly impact longevity and/or quality of life?
2. List four characteristic craniofacial features of individuals with Trisomy 21.
3. Name common intra-oral findings in individuals with Trisomy 21.
4. List features of Trisomy 21 that make these patients poor candidates for outpatient sedation procedures.
5. What is the probable explanation for the increased incidence of early, aggressive periodontal disease in many individuals with Trisomy 21?
Answers are located at the end of the case.
Bibliography
American Academy of Pediatric Dentistry. 2011–2012. Guideline on Caries-risk Assessment and Management for Infants, Children, and Adolescents, Reference Manual. Pediatr Dent 33(6):110–15.
Freeman SB. et al. 1998. Population-based study of congenital heart defects in Down syndrome. Am J of Medical Genetics 16;80(3):213–17.
Mitchell RB, Call E, Kelly J. 2003. Ear, nose and throat disorders in children with Down syndrome. Laryngoscope 113(2):259–63.
National Institute of Child Health and Human Development. www.nichd.nih.gov/health/topics/Down_Syndrome.cfm.
Pilcher, ES. 1998. Dental care for the patient with Down syndrome. Down Syndrome Research and Practice 5(3):111–16.
Shaw L, Saxby MS. 1986. Periodontal destruction in Down’s syndrome and in juvenile periodontitis; how close a similarity? J of Periodontology 57:709–13.
Yavuzyilmaz E. et al. 1993. Neutrophil chemotaxis and periodontal status in Down syndrome patients. J of Nihon University School of Dentistry 35:91–5.
SELF-STUDY ANSWERS
1. Congenital heart defects, cognitive impairment, compromised immune response, thyroid disorders, cervical spine instability, increased risk for development of leukemia, increased incidence of early development of senile dementia
2. Hypoplastic midface, mild microcephaly, upslanted palpebral fissures, short neck
3. Hypodontia, microdontia, delayed dental eruption, ectopic dental eruption, dental impactions, crowding of maxillary dentition, relative macroglossia, class III malocclusion
4. Increased incidence of airway anomalies, small naso-pharyngeal complex, hypotonia, obesity, increased incidence of congenital heart defects, increased incidence of spinal deformities and instability
5. Individuals with Trisomy 21 have a compromised immune response, which places them at increased susceptibility for chronic infectious processes. This is the probable explanation for their relatively high incidence of periodontal disease.
Case 2
Cerebral Palsy, Bronchopulmonary Dysplasia
A. Presenting Patient
- 8-year-, 2-month-old Caucasian male
- Diagnosed with cerebral palsy, bronchopulmonary dysplasia, asthma, and mild intellectual disability
B. Chief Complaint
- Patient presenting for recall appointment; last dental visit was 18 months ago
C. Social History
- Patient attends school; is in a class for children with special educational needs
- Child lives at home with mother, father, and 3 older siblings
- Father works full time; mother is a full-time homemaker
- Socio-economic status is lower middle class
D. Medical History (see Background Information 1)
- Premature birth (child was born at 26 weeks gestational age, birth weight = 978 g) (see Fundamental Point 1)
- Cerebral palsy, mixed type (spastic and dyskinetic)
- Status post bronchopulmonary dysplasia secondary to long neonatal course of positive pressure ventilation
- Hospitalization for aspiration pneumonia at age 2
- Mild/moderate asthma, currently managed with Flovent (fluticasone) and albuterol inhalers used on a daily basis
- Mild intellectual disability
- Cerebral palsy can be described as “A group of disorders of the development of movement and posture causing activity limitations that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disturbances of cerebral palsy are often accompanied by disturbances of sensation, cognition, communication, perception, and/or behavior and/or a seizure disorder.” (Bax et al. 2005)
- Bronchopulmonary dysplasia (BPD) is a common complication of preterm birth. It is seen most frequently in infants born prior to 30 weeks gestational age and weighing <1,200g at birth. It is related to the need for positive-pressure ventilation (PPV) in neonates with poorly developed pulmonary systems. PPV can result in injury to the pulmonary microvasculature and alveolar structures. Neonates with BPD are at increased risk for abnormal pulmonary function into late childhood and possibly adulthood (Blayney et al. 1991, Jobe and Bancalari 2001).
- Children who are born at extremely low birth weights (<1,000 g) are at risk for a number of medical and developmental conditions that can persist past the neonatal period and result in health care issues throughout life. These include:
- Cerebral palsy
- Bronchopulmonary dysplasia (with subsequent higher rates of asthma than children born at full gestational age)
- Patent ductus arteriosis
- Intellectual disability
- Visual impairment (retinopathy of prematurity)
- Hearing impairment
Hack et al. (2005)
E. Medical Consult
- Consulted with primary care physician to ascertain patient’s current respiratory status, which is stable
F. Dental History
- Has been managed at the same dental clinic since 3 years of age
- Attendance at clinic has been sporadic (last visit 18 months ago)
- Positive behavior for brief procedures, but very active in dental chair: Try to keep appointments short
- Not a frequent snacker, eats mostly at meal time
- Optimal water fluoridation levels
- Brushes without supervision (once or twice per day)
G. Extra-oral Exam (Figure 8.2.1)
- No significant findings
Figure 8.2.1. Facial photograph

H. Intra-oral Exam (see Figures 8.2.2a–c and Fundamental Point 2)
- Early mixed dentition (slightly delayed for age)
- Possible intra- and extra-oral concerns in patients with cerebral palsy (CP) (Ortega et al. 2007):
- Hypotonia of the tongue and perioral musculature can result in anterior open bites and constricted palates. (This particular patient does not have a constricted palate).
- Immature swallow pattern, with characteristic tongue thrust, can also contribute to anterior open bite.
- A poor swallow reflex, seen in some patients with CP, can result in persistent drooling, which can irritate skin in the peri-oral region.
- Patients who use inhaled medication for control of asthma may show the following oral findings (McDonald, Avery, and Dean 2011):
- Increased caries risk (due to reduced salivary flow)
- Gingivitis
- Throat irritation
- Candidiasis
Figure 8.2.2a–c. Intra-oral photos showing generalized marginal gingivitis and mandibular crowding

Occlusion
- 9-mm overjet, anterior open bite
- Moderate crowding of the lower arch
- Mesial step primary molars, class I canines
Poor Oral Hygiene
- Generalized marginal gingivitis
- Clinical exam suggests caries-free dentition
I. Diagnostic Tools
- Radiographs (bitewings and a panoramic film) were attempted, but were of poor diagnostic quality due to patient’s difficulty staying still
J. Differential Diagnosis
- N/A
K. Diagnosis and Problem List
Diagnosis
- Cerebral palsy
- Cognitive impairment (mild)
- Status post bronchopulmonary dysplasia with current mild/moderate asthma
Problem List
- Irregular use of a dental home
- Gingival inflammation due to poor oral hygiene
- High caries risk due to poor oral hygiene and asthma medications
- Unknown caries status of interproximal surfaces
- Large overjet increases risk of traumatic dental injury
- Moderate mandibular crowding
- Caries risk: Use the American Academy of Pediatric Dentistry Caries Assessment Tool (CAT) in assigning a patient’s risk category AAPD (2011–2012a)
- Provide dietary counseling to the parent AAPD (2011–2012a and b)
- Gingival inflammation
- Stress to parent the importance of daily oral home care. Instruct the parent to help with child’s oral hygiene.
- Schedule recall visits at more regular intervals to assess home care, perform prophylaxis, and monitor gingival inflammation (AAPD 2011–2012c)
- Malocclusion: Conduct orthodontic evaluation in early mixed dentition
- Assess tooth size, shape, position
- Conduct space analysis (AAPD 2011–2012d)
L. Comprehensive Treatment Plan
- Dental prophylaxis (sedation may be necessary)
- Fluoride treatment
- Review of oral hygiene and diet (with parent and child)
- Orthodontic consultation
- Space analysis to evaluate arch length
- Evaluate patient’s behavior regarding his ability to cooperate for orthodontic treatment (if treatment is indicated at this time).
- Three-month recall
- Re-evaluate caries risk
- Re-evaluate oral hygiene and soft tissue status
M. Intra-Oral and Post-operative Images
- N/A
N. Prognosis and Discussion
- Although the patient is in a high risk category for dental caries due to poor oral hygiene, he has never had a carious lesion. The prognosis for continued periodontal pathology is high due to poor hygiene, but could improve with better daily oral hygiene. Even performing a thorough prophylaxis may be difficult and sedation may be considered (see Fundamental Point 4).
- The prognosis for malocclusion is poor. Although the patient is fairly cooperative for oral examinations and prophylaxis, it is not clear what his level of cooperation would be for lengthier or more complicated treatments. This must be evaluated and taken into consideration before a decision is made to begin orthodontic treatment.
- This patient’s history of bronchopulmonary dysplasia, aspiration pneumonia, and mild/moderate asthma puts him at risk for respiratory complications during sedation. According to the American Society of Anesthesiologists (ASA) physical status classification system, the patient would be ASA class II (mild systemic disease). If the patient required dental procedures that could not be completed without sedation and/or general anesthesia, his respiratory history should be taken into consideration when deciding the most appropriate setting (i.e., outpatient clinic or hospital OR) and type of anesthesia. (AAPD 2011–2012e)
O. Complications and Alternative Treatment Plan
- If the patient had dental caries present, would the behavior management techniques previously used be adequate to accomplish the needed treatment?
- Is this child an appropriate candidate for in-office sedation, or would he be better managed in a hospital operating room setting, if treatment needs dictated?
- Would there be any difference in this child’s orthodontic treatment at this age, if behavior was not a consideration?
Self-study Questions
1. What are some common complications of extreme low birth weight that can have long-term sequelae?
2. Name three oral/perioral complications sometimes seen in patients with cerebral palsy.
3. What is the etiology for the complications mentioned in question 2?
4. True or False: Cerebral palsy is a progressive neurologic disorder.
5. In what category of neonates does bronchopulmonary dysplasia most frequently develop?
Answers are located at the end of the case.
Bibliography
American Academy of Pediatric Dentistry. 2011–2012a. Guideline on Caries-risk Assessment and Management for Infants, Children, and Adolescents, Reference Manual. Pediatr Dent 33(6):110–15.
American Academy of Pediatric Dentistry. 2011–2012b. Policy on Dietary Recommendations, Reference Manual. Pediatr Dent 33(6):53–4.
American Academy of Pediatric Dentistry. 2011–2012c. Periodicity of Examination, Reference Manual. Pediatr Dent 33(6):102–9.
American Academy of Pediatric Dentistry. 2011–2012d. Management of the Developing Dentition, Reference Manual. Pediatr Dent 33(6):229–41.
American Academy of Pediatric Dentistry. 2011–2012e. Guideline for Monitoring and Management of Pediatric Patients During and After Sedation for Diagnostic and Therapeutic Procedures, Reference Manual. Pediatr Dent 33(6):185–201.
Bax M, Goldstein M, Rosenbaum P, et al. 2005. Proposed definition and classification of cerebral palsy. Dev Med Child Neurol Aug; 47(8):571–6.
Blayney M, Kerem E, Why/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses