3
Complex Pulp Therapy
Case 1
Indirect Pulp Treatment
Figure 3.1.1a–b. Facial photographs
A. Presenting Patient
- 6-year-, 6-month-old Hispanic female
- Recall visit two years after last appointment
B. Chief Complaint and History of Present Injury
- Patient’s father stated that his daughter “complained of toothache the last few days in the lower back right side, and I can see she has several cavities. She has not been to the dentist for a long time.”
- Describe the pain. Does it linger or subside after stimulus is removed? Is the pain spontaneous?
- What are the frequency, severity, duration, triggering agents of the pain (thermal, food, sleeping)?
- What are the symptoms (fever, swelling)?
- What has been the analgesic use?
C. Social History
- Middle class
- Patient is in 1st grade
D. Medical History
- No significant findings, no known drug or food allergies, no medications, vaccinations are up to date
E. Medical Consult
- N/A
F. Dental History
- Dental home was established at the age 16 months when initial signs of early childhood caries were observed on the maxillary primary incisors. Fluoride varnish applications were recommended every three months at that time
- Despite recommendation for routine six-month recalls, two years have passed since last visit
- Cariogenic diet
- Poor oral hygiene, brushes once daily, unsupervised
- Uses toothpaste containing fluoride
- Lives in an optimally fluoridated area
- No history of dental/oral trauma
- Cooperative behavior for all past dental care
G. Extra-oral Exam
- No significant findings
H. Intra-oral Exam
Soft Tissues
- No significant findings
Hard Tissues
- No significant findings
Occlusal Evaluation of Primary Dentition
- Mesial step molars, class III right canines, class I left canines
Other
- Moderate plaque accumulation
- Several teeth with moderate to extensive carious lesions
- Mandibular right primary second molar with an extensive carious lesion
I. Diagnostic Tools
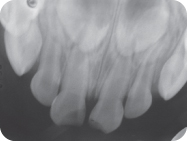
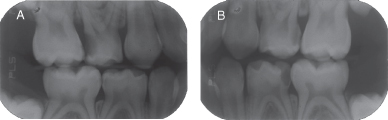
- Periapical radiograph of the mandibular right primary second molar at the time of the initial appointment (Figure 3.1.2) shows a large occlusal carious lesion. It was treated with a pulpectomy as an emergency
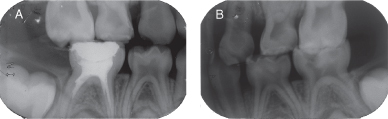
- Right and left bitewing radiographs were taken after the initial visit, which focused on emergency treatment of the mandibular right primary second molar (Figures 3.1.3 a, b)
- The bitewing radiographs showed deep carious lesions on the maxillary right primary second molar and on the mandibular left primary second molar (Figure 3.1.3.)
Figure 3.1.2. Pre-op periapical radiograph of the mandibular right primary second molar
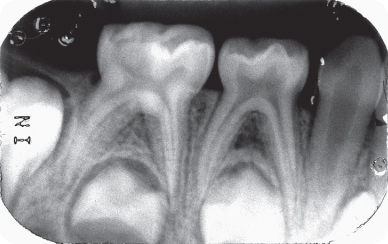
Figure 3.1.3a–b. Bitewing radiographs after pulpectomy and prior to IPT treatments. A. Right bitewing radiograph, B. left bitewing radiograph
J. Differential Diagnosis
For the Maxillary Right and the Mandibular Left Primary Second Molars:
- Deep carious lesions with possible pulp involvement
- Deep carious lesions with partial necrosis
- Deep carious lesions with total necrosis
K. Diagnosis and Problem List
Diagnosis
- Extensive carious lesions in several primary molars
- Deep carious lesion on the right mandibular second primary molar (treated with a pulpectomy in the initial appointment as an emergency)
- Maxillary right and mandibular left primary second molars with deep carious lesions without signs or symptoms of irreversible pulpits and no soft tissue pathology
- No radiographic signs of pulpal nor peri-radicular pathology
Problem List
- High caries risk due to several factors: cariogenic diet, poor oral hygiene, moderate plaque accumulation, unsupervised brushing, no regular dental visits
- Several untreated carious lesions with possible reversible and/or irreversible pulp involvement
L. Comprehensive Treatment Plan
- Emergency treatment of the right mandibular primary second molar
- Explanation to the father of the importance of maintaining a primary second molar, particularly prior to the eruption of the first permanent molar
- Indirect pulp treatment (IPT) technique was chosen for the deep lesions of the maxillary right and mandibular left primary second molars, considering that they were asymptomatic and amenable to be properly sealed with leakage-free restorations
- Comprehensive treatment of other carious lesions: Consider using nitrous oxide analgesia given the length of the procedures
- Follow up care including:
- Immediate post-op and home care instructions
- Prevention plan
- Recall visits every three months, including fluoride varnish application and caries risk re-evaluation
- Follow up radiographs after six months
- Indirect pulp treatment (IPT) is recommended for teeth that have deep, carious lesions approximating the pulp but without signs or symptoms of pulp degeneration.
- In this procedure, the deepest layer of the remaining carious dentin is covered with a biocompatible material to prevent pulp exposure and additional trauma to the tooth. This results in the deposition of tertiary dentin, which increases the distance between the affected dentin and the pulp, and in the deposition of peritubular (sclerotic) dentin, decreasing dentin permeability. It is important to remove the carious tissue completely from the dentino-enamel junction (DEJ) and from the lateral walls of the cavity to achieve optimal interfacial seal between the tooth and the restorative material, thus preventing microleakage.
- The dilemma that clinicians face lies in the assessment of how much caries to leave on the pulpal or axial floor. The carious tissue that should remain on the floor of the cavity preparation is a quantity that, if removed, would result in overt exposure. It is difficult to determine whether an area is an infected carious lesion or a bacteria-free demineralized zone. The best clinical marker is the quality of the dentin: soft, mushy dentin should be removed, and hard, discolored dentin can be indirectly capped.
- The ultimate objective of this treatment is to maintain pulp vitality by:
- Arresting the carious process
- Promoting dentin sclerosis (reducing permeability)
- Stimulating the formation of tertiary dentin
- Remineralizing the carious dentin.
- Two materials have been most commonly used in IPT: Ca(OH)2 and zinc oxide–eugenol paste. Lately, glass ionomer cements have also been successfully used in this procedure. Massara, Alves, and Brandao (2002) demonstrated that glass ionomer creates conditions that lead to remineralization and recommended it as a good base for IPT.
IPT Technique
- Local anesthesia and rubber dam
- Caries removal leaving affected dentin over the pulpal floor
- Coverage of the affected dentin with glass ionomer cement. This material was chosen due to its biocompatible properties, ability to promote remineralization of the demineralized dentin, and fluoride release capacity
- Both teeth received a Class I restoration using a composite resin material followed by a fissure sealant
M. Clinical and Radiographic Follow-up
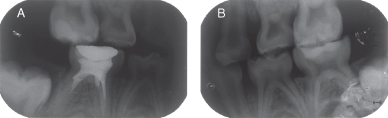
- Ten months after IPT on the maxillary right primary second molar (Figure 3.1.4a) and on the mandibular left primary second molar (Figure 3.1.4b). Notice the retraction of the distal pulp horn due to the formation of reactionary dentin on both teeth
Figure 3.1.4a–b. Post-IPT bitewing radiographs. A. Post-op right bitewing radiograph, B. Post-op left bitewing radiograph
N. Prognosis and Discussion
- Prognosis for caries: The recommended protocol for decreasing caries risk depends on the parents’ understanding and compliance in reducing the identified risk factors and in attending regular recall exams. In the present case, the parent brought the child for a recall visit 10 months after the completion of the initial comprehensive dental treatment, instead of the recommended six months. At that time, new lesions were identified
- Prognosis for IPT: The prognosis for IPT is usually good. Partial caries removal in asymptomatic primary or permanent teeth reduces the risk of pulp exposure. Success rates of IPT have been reported to be higher than 90% in primary teeth; thus, its use is recommended in patients in whom a pre-operative diagnosis suggests no signs of pulp degeneration. The value of taking a good history complemented by a careful clinical and radiographic examination cannot be overestimated. Studies investigating the long-term outcome of partial caries removal have used either composite resins or stainless steel crowns as the restorative material. A recent systematic review of the literature (Ricketts et al. 2006) reported no difference in the incidence of pulp exposure, in the progression of the decay and on the longevity of restorations, irrespective of whether the removal of decay had been minimal (ultraconservative) or complete. In the present case, the longevity of the composite restoration also depends on a periodic clinical follow-up to check the integrity of the margins of the restoration to rule out microleakage. In addition, the presence of a new proximal lesion might jeopardize the success of the IPT by contamination of bacteria and/or their toxins. Therefore, in children with high caries risk, using a stainless steel crown over an IPT is suggested. The most relevant factor noted in the present case that can contribute to a poor prognosis is the patient’s lack of compliance with dental appointments
O. Common Complications and Alternative Treatment Plans
- The most common complications of a failing IPT are pulp necrosis and/or a periapical lesion. These may be the result of an initial misdiagnosis of an irreversibly inflamed or necrotic pulp or due to a poor restoration leading to microleakage.
- Alternative treatments include pulpotomy or pulpectomy
Self-study Questions
1. What could have prevented the amount and severity of the carious lesions in the present case?
2. Could a sealant have prevented these lesions?
3. Has the adopted approach to prevent pulp exposure (IPT) been evaluated and supported by the literature?
4. When is an IPT contraindicated for primary molars?
5. Should poor compliance and high caries risk influence the choice of treatment?
Answers are located at the end of the case.
Bibliography and Additional Reading
Fuks AB. 2005. Pulp therapy for the primary dentition. In: Pediatric Dentistry, Infancy through Adolescence 4th Edition. Pinkham JR, Casamassimo PS, Fields HW Jr., McTigue DJ, Nowak AJ (eds). Elsevier Saunders: St. Louis. pp. 375–93.
Massara MLA, Alves JB, Brandão PRG. 2002. Atraumatic restorative treatment: Clinical, ultrastructural and chemical analysis. Caries Res 36:430.
Ricketts DNJ, Kidd EAM, Innes N, Clarkson J. 2006. Complete or ultraconservative removal of decayed tissue in unfilled teeth. Cochrane Database of Systematic Reviews. Jul 19; 3:CD003808.
SELF-STUDY ANSWERS
1. If the child’s parents would have had a better compliance and followed the six-month recall protocol, at least the severity of the lesions could be controlled and new lesions prevented
2. Probably yes. Sealants are indicated for primary and permanent teeth with pits and fissures that are predisposed to plaque retention. If the sealant covering the susceptible fissure is intact, it can definitely prevent the development of caries
3. Yes. A systematic review of the literature (Ricketts et al. 2006) reported no difference in the incidence of pulp exposure, in the progression of the decay and on the longevity of restorations, irrespective of whether the removal of decay had been minimal (ultraconservative) or complete
4. IPT is contraindicated for primary molars when there is a history of spontaneous pain or any clinical and/or radiographic pathological signs. The tooth must be vital to be treated with IPT
5. Yes. In patients with high caries risk and poor compliance, it is preferable to use radical treatment approaches, such as stainless steel crowns, instead of multi-surface restorations
Case 2
Partial Pulpotomy in Traumatized Primary Incisors
Figure 3.2.1. Facial photograph

A. Presenting Patient
- 4-year-, 2-month-old Caucasian female
- New patient presenting as an emergency
B. Chief Complaint
- Mother stated, “My daughter fell while playing with other children in the kindergarten yard and fractured her two upper front teeth”
C. Social History
- Second of three children
- Both parents are well educated
- Middle class, mother works part time
D. Medical History
- No significant findings, no known food or drug allergies, no medications, vaccinations are up to date
E. Medical Consult
- N/A
F. Dental History
- Has dental home
- Eating habits include a balanced diet rich in proteins and low in carbohydrates. The child eats regular meals and the parents demand that their children limit the ingestion of sweets to after meals
- Fair oral hygiene habits, brushes twice daily with parental supervision
- Uses toothpaste containing fluoride
- Optimal water fluoridation levels
- No history of previous trauma
G. Extra-oral Exam
- Mild swelling of the upper lip
H. Intra-oral Exam
Soft Tissues
- Bruises on labial mucosa, gingival laceration on maxillary anterior area, and laceration of the labial frenum
Hard Tissues
- No significant findings
Occlusion Evaluation of Primary Dentition
- Mesial step molars, class I canines
Other
- Moderate plaque accumulation over the fractured teeth
- Caries-free primary dentition
- Maxillary central incisors with complicated crown fractures
- Mild sensitivity to percussion on both maxillary central incisors
- Physiologic mobility on both traumatized incisors
- Extremely apprehensive
I. Diagnostic Tools
- Anterior maxillary periapical radiograph (Figure 3.2.2). Bitewing radiographs were not taken because the patient has periodical examinations at her family dentist
Figure 3.2.2. Anterior maxillary periapical radiograph showing crown fractures with pulp involvement
J. Differential Diagnosis
- Complicated crown fractures of maxillary primary central incisors
- Complicated crown–root fractures
- Complicated crown fractures associated with subluxation
K. Diagnosis and Problem List
Diagnosis
- Based on the history of pain, clinical examination, and radiographic findings, the most probable diagnosis is complicated crown fractures of maxillary primary central incisors
Problem List
- Maxillary primary central incisors with exposed pulps and pulp polyps needing emergency treatment
- Child has never had a local anesthetic
- Definition: Enamel-dentin fracture with pulp exposure
- Diagnosis: Clinical and radiographic findings reveal a loss of tooth structure with pulp exposure
- Treatment objectives: Maintain pulp vitality and restore normal esthetics and function. Injured lips, tongue, and gingiva should be examined for tooth fragments.
- Pulpal treatment alternatives are pulpotomy, pulpectomy, and extraction
- Keep treatment as simple as possible, taking into consideration the child’s behavior and the life span of the tooth. Decisions often are based on life expectancy of the traumatized primary tooth and vitality of the pulpal tissue
- Risk of treatment and possible sequelae to the permanent tooth should be assessed versus the functional benefit resulting from treatment to the primary tooth
L. Comprehensive Treatment Plan
- Emergency treatment of the exposed pulps
- Explanation to the mother of the importance of maintaining the vitality of both teeth
- Behavioral management considerations (consider using nitrous oxide analgesia)
- Follow-up care including:
- Post-op and home care instructions
- Recall plan
- Radiographs should be taken after 3, 6, 12, 18, and 24 months and thereafter at yearly intervals until physiologic exfoliation of the teeth
- Preserves cell-rich coronal pulp
- Increases healing potential due to preserved pulp
- Physiologic apposition of cervical dentin
- Obviates need for root canal therapy
- Preserves natural color and translucency
- Maintains pulp test responses
- Initially performed only in permanent teeth. Presently, there is enough evidence that this procedure can also be applied in primary teeth
- After the diagnosis is completed, the tooth is anesthetized.
- If possible, pulpal procedures should always be performed under rubber dam isolation and aseptic conditions to prevent further introduction of microorganisms into the pulp tissues (Figure 3.2.3). Care must be taken when placing the rubber dam on a traumatized tooth. If any loosening of the tooth has occurred, the rubber dam clamps must be applied to adjacent uninjured teeth
- In traumatically exposed pulps, only tissue judged to be inflamed is removed. Cvek (1994) showed that with pulp exposures resulting from traumatic injuries, regardless of the size of the exposure or the amount of lapsed time, pulpal changes are characterized by a proliferative response with inflammation extending only a few millimeters into the pulp. When this hyperplastic, inflamed tissue is removed (about 2 mm), healthy pulp tissue is encountered. In teeth with carious exposure of the pulp, it may be necessary to remove pulp tissue to a greater depth to reach uninflamed tissue.
- The instrument of choice for tissue removal in the pulpotomy procedure is an abrasive diamond bur, using high speed with adequate water cooling. This technique has been shown to create the least damage to the underlying tissue.
- Care must be exercised to ensure removal of all filaments of the pulp tissue coronal to the amputation site; otherwise, hemorrhage will be impossible to control.
- After pulpal amputation, the preparation is thoroughly washed with physiologic saline or sterile water to remove all debris; the water is removed by vacuum and cotton pellets (Figure 3.2.4). Air should not be blown on the exposed pulp, because it will cause desiccation and tissue damage.
- Hemorrhage is controlled by cotton pellets slightly moistened with saline (i.e., wetted and blotted almost dry) placed against the stumps of the pulp. Completely dry cotton pellets should not be used because fibers of the dry cotton will be incorporated into the clot and, when removed, will cause hemorrhage. Dry cotton pellets are placed over the moist pellets, and slight pressure is exerted on the mass to control the hemorrhage.
- Hemorrhage should be controlled in this manner within several minutes. It may be necessary to change the pellets to control all hemorrhage. If hemorrhage continues, the clinician must carefully check to be sure that all filaments of the pulp coronal to the amputation site were removed and that the site is clean.
- Sodium hypochlorite (2.5% NaOCl) can be placed on the exposure site to cause hemostasis before pulp capping. It also has the beneficial effect of killing bacteria. It was reported that when used as a hemostatic agent there was no damage to pulpal cells and it did not inhibit pulpal healing, odontoblastic cell formation, or dentinal bridging.
- If hemorrhage cannot be controlled, pulpal amputation should be performed at a more apical level. Once the hemorrhage is controlled, Ca(OH)2 or mineral trioxide aggregate (MTA) is placed in the canal against the pulp stump. A thin layer of intermediate restorative material or flowable composite resin is placed over the Ca(OH)2 or MTA and light cured (Figure 3.2.5); otherwise, the material would be washed out during the acid etching procedure. The tooth is then sealed with an etched bonded composite strip crown restoration (Figure 3.2.6).
Figure 3.2.3. Placement of rubber dam after administration of a local anesthetic
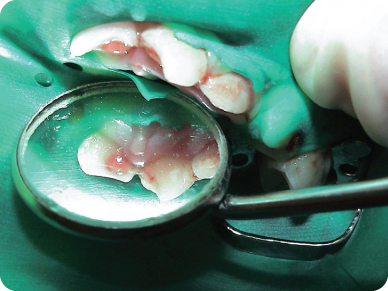
Figure 3.2.4. After pulp amputation, the area is rinsed with saline, and hemostasis is achieved with cotton pellet pressure
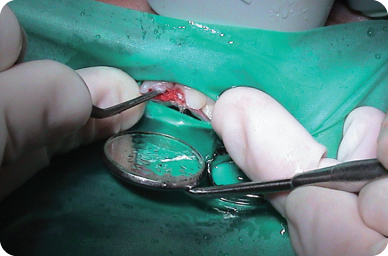
Figure 3.2.5. After hemostasis, the amputated areas are covered with calcium hydroxide or mineral trioxide aggregate, followed by intermediate restorative material
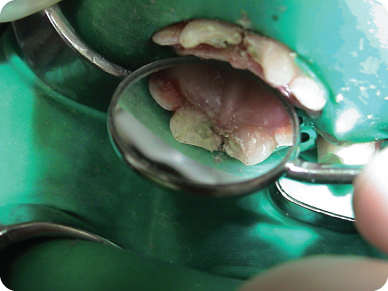
Figure 3.2.6. Completed restorations showing good esthetic results. The pulps remained vital

M. Prognosis and Discussion
- Long-term studies have shown very high success rates of pulp capping and partial pulpotomy with respect to pulp survival. Radiographic evidence of hard tissue closure of the perforation can be seen three months after pulp capping. Most of the studies were done in permanent teeth
- The primary factor to pulp survival after crown fracture is compromised pulp circulation due to luxation injuries. Crown fracture with concomitant luxation injury has been shown to have an increased incidence of pulpal necrosis. Cvek (1994) reported 96% success with partial pulpotomy using Ca(OH)2 on traumatically exposed permanent pulps. Size of the exposure or time between injury and treatment was not critical as long as the superficially inflamed pulp tissue was removed before capping. These studies included both mature teeth and teeth with immature roots. Subsequent investigations have verified these findings. In a long-term follow-up study of partial pulpotomy in permanent teeth, those judged to be healed at three years remained healed 10 to 15 years later.
- Only in the last few years did partial pulpotomy with Ca(OH)2 or mineral trioxide aggregate (MTA) start to be used as treatment modalities for traumatized primary incisors with pulp exposure. This was probably due to the traditional belief that pulpotomy with Ca(OH)2 results in internal root resorption. Today we know that most pulp dressing agents can lead to this pathologic complication, and may be due to the condition of the exposed pulp. Because the pulp is normal in traumatized exposures (except for the exposure area), removing the affected tissue brings about a good prognosis.
- The recommended treatment for traumatized primary teeth with pulp exposure is pulpectomy and full coverage, stainless steel crown [SSC] or composite strip crown (see Chapter 4, Flowchart C). Most root canal filling pastes cause discoloration of the tooth that can be seen through the composite crown. In addition, the tooth becomes brittle and more prone to fracture.
N. Complications and Alternative Treatment Plans
- Unsuccessful partial pulpotomy can result in pulp necrosis and/or a periapical abscess with or without a fistula. These complications can be the result of chronic irritation due to microleakage from an improperly adapted SSC or defective strip crown. Another reason for failure can be related to recurrent trauma, a relatively common finding in young children. These complications can also occur if the initial treatment was a pulpectomy and SSC.
- Extraction is an alternative, but less desirable in a young child
Self-study Questions
1. What are the treatment objectives for a complicated crown fracture?
2. What is the treatment recommended by the American Academy of Pediatric Dentistry for a complicated crown fracture in a traumatized primary incisor?
3. According to Cvek, what are the pulpal changes resulting from a traumatic pulp exposure?
4. What are the advantages of using sodium hydrochloride (NaOCl) to control pulpal hemorrhage during a pulpotomy procedure?
5. What are the advantages of a partial pulpotomy over a pulpectomy for treatment of a complicated crown fracture?
6. What are the most commonly used pulp dressing materials in partial pulpotomy, and what are their properties?
Answers are located at the end of the case.
Bibliography and Additional Reading
Casas M, Fuk AB. 2011. Pulp therapy in primary and young permanent teeth. In: The Handbook of Pediatric Dentistry, 4th Edition. Nowak AJ, Casamassimo PS (eds). American Academy of Pediatric Dentistry, pp. 91–8.
Camp JH, Fuks AB. 2006. Pediatric endodontics: Endodontic treatment for the primary and young permanent dentition. In: Pathways of the Pulp, 9th Edition. Cohen S, Hargreaves KM (eds). Mosby Elsevier: St. Louis. Chapter 22.
Cvek M. 1994. Endodontic management of traumatized teeth. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 3rd Edition. In: Andreasen JO, Andreasen FM (eds). Munksgaard: Copenhagen.
Kupietzky A, Holan G. 2003. Treatment of crown fractures with pulp exposure in primary incisors. Pediatr Dent 25:241–48.
Fuks AB, Heling I. Pulp therapy for the young permanent dentition. In: Pediatric Dentistry Infancy through Adolescence, 4th Edition. Pinkham JR, Casamassimo PS, Fields HW Jr., McTigue DJ, Nowak AJ (eds). Elsevier Saunders: St. Louis. Chapter 33.
SELF-STUDY ANSWERS
1. To maintain pulp vitality and restore normal esthetics and function
2. Pulpectomy followed by a SSC or a composite strip crown
3. Cvek has shown that with pulp exposures resulting from traumatic injuries, regardless of the size of the exposure or the amount of lapsed time, pulpal changes are characterized by a proliferative response with inflammation extending only a few millimeters into the pulp (Cvek, 1994)
4. NaOCl, when placed on the exposure site, causes hemostasis, has a beneficial effect of killing bacteria, and does not damage the pulpal cells
5. Partial pulpotomy allows for the preservation of cell-rich coronal pulp, increases the healing potential due to preservation of the pulp, allows the physiologic apposition of cervical dentin, obviates the need for root canal therapy, and preserves the natural color and translucency
6. Calcium hydroxide and MTA. Both stimulate the healing of the pulp and the formation of a dentin bridge
Case 3
Cervical Pulpotomy in Cariously Exposed Primary Molars
Figure 3.3.1a–b. Facial photographs
A. Presenting Patient
- 5-year-, 6-month-old Hispanic female
- New patient presenting as an emergency
B. Chief Complaint
- Mother confirmed the patient’s complaint of pain in the lower left quadrant while eating; it subsides after a few minutes without taking analgesics
C. Social History
- Fourth of nine children
- Lower socio-economic status
D. Medical History
- Review of medical history revealed no significant findings, no known drug or food allergies, no medications, vaccinations are up to date
E. Medical Consult
- N/A
F. Dental History
- No dental home
- Eating habits include a low-protein, high-carbohydrate diet
- Poor oral hygiene, brushes without supervision
- Uses toothpaste containing fluoride
- Optimal water fluoridation levels
- No history of trauma
- Seven-day history of pain without history of swelling or fever
G. Extra-oral Exam
- No significant findings
H. Intra-oral Exam
Soft Tissues
- Generalized gingivitis
Hard Tissues
- No significant findings
Occlusal Evaluation of Primary Dentition
- Mesial step molars and class I canines
Other
- Extensive plaque accumulation
- Several teeth with extensive carious lesions: maxillary first primary molars, mandibular left first primary molars, maxillary lateral and central incisors
I. Diagnostic Tools
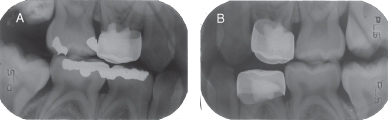
- Periapical radiograph of the maxillary incisors (Figure 3.3.2.)
- Two bitewings (Figure 3.3.3.)
- Unable to obtain posterior periapical radiographs (uncooperative behavior for the periapical radiographs)
- Radiographic lesions on maxillary first and second primary molars, maxillary lateral and central incisors, left mandibular first primary molar, mandibular primary canines, and mandibular right first and second primary molars
Figure 3.3.2. Periapical radiograph of the maxillary incisor

Figure 3.3.3a–b. Bitewing radiographs. A. Right bitewing radiograph, B. Left bitewing radiograph
J. Differential Diagnosis
- Deep carious lesions
- Reversible pulp inflammation
- Irrreversible pulp inflammation
- Partial pulp necrosis
- Total pulp necrosis
K. Diagnosis and Problem List
Diagnosis
- Based on the history of pain, clinical examination, and radiographic findings, the most probable diagnosis for the left mandibular first primary molar is a deep carious lesions with reversible pulp inflammation
Problem List
- Several untreated carious lesions
- High caries risk due to several factors (cariogenic diet, poor oral hygiene with extensive plaque accumulation)
- Lack of dental home
- Eradicate potential for infection
- Maintain tooth in a quiescent state
- Preserve space for underlying permanent tooth
- Retain primary tooth if permanent tooth is congenitally absent
- Tooth with deep caries without pulp exposure
- Carious or traumatic pulp exposure with transitory thermal and/or chemical stimulated pain
- Physiologic mobility
- Normal soft tissues
- No percussion sensitivity (except in cases of food impaction)
- Intact continuous ligament space
- Intact periapical and/or furcation bone
- Color of pulpal hemorrhage not a reliable indicator of pulp histological status
- Excessive bleeding is strongly correlated with degenerative changes
- One-third of teeth with carious pulp exposures have “normal” pulps
- One-third of teeth with deep caries with no pulp exposures have “abnormal” pulps
L. Comprehensive Treatment Plan
- Urgent treatment of the left first primary molar with formocresol pulpotomy and stainless steel crown (SSC)
- Explanation to the mother of the importance of maintaining the primary molars for proper occlusion
- Comprehensive treatment of other carious lesions
- Follow-up care including:
- Post-op and home care instructions
- Caries prevention plan
- Appropriate prevention and recall plan
- Excavate caries, amputate coronal pulp, achieve hemostasis, treat radicular pulp with medicament, restore with permanent restoration
- Dilute FC using one part FC to four parts vehicle (three parts glycerine: one part water) and apply for five minutes
- Dilution mixture settles out; re-mixing indicated
- Method of action: tissue fixation
- Histological zones in FC-treated radicular pulp
- Acidophilic zone: Fixation (coronal)
- Pale staining zone: Atrophy (middle)
- Broad zone of inflammatory cells (apical)
- Bactericidal
- 62% to 97% acceptable outcome
- No dentinal bridging, but calcific changes evident
- Persistent chronic inflammation
- Small risk of succedaneous tooth damage
- Exfoliation accelerated
- Cellular toxicity
- Immune sensitization risk
- Humoral and cell–mediated responses: Controversial
- Mutagenic and carcinogenic potential: Controversial
- 15.5% in aqueous base, pH = 1
- Method of action: Hemostatic, denatures protein, and forms ferric ion complex that occludes cut blood vessels
- Shorter application time than FC (10 to 15 seconds)
- Equivalent outcome to FC
- Self-limiting internal resorption reported
- Method of action: Mineralization, dental cement with discrete crystals and amorphous structure, pH = 12.5
- Pulp canal obliteration common
- Equivalent outcome to FC
- Promising clinical results
M. Radiographic Follow-up
- Post-operative bite-wing radiographs (Figure 3.3.4.)
Figure 3.3.4a–b. Post-op bitewing radiographs. A. Post-op right bitewing radiograph, B. post-op left bitewing radiograph
N. Prognosis and Discussion
- The pulpotomy procedure is based on the rationale that the radicular pulp tissue is healthy or is capable of healing after surgical amputation of the affected or infected coronal pulp. The presence of any signs or symptoms of inflammation extending beyond the coronal pulp is a contraindication for a pulpotomy. In the present case, removing the soft and mushy dentin in the three first primary molars resulted in pulp exposure, and the teeth were treated with a formocresol pulpotomy and restored with SSCs
- The ideal dressing material for the radicular pulp should:
- Be bactericidal
- Be harmless to the pulp and surrounding structures
- Promote healing of the radicular pulp
- Not interfere with the physiologic process of root resorption
- A good deal of controversy surrounds the issue of pulpotomy agents, and, unfortunately, the “ideal” pulp dressing material has not yet been identified. The most commonly used pulp dressing material is formocresol (Buckley’s solution: formaldehyde, cresol, glycerol, and water). Clinical and radiographic studies have demonstrated that formocresol pulpotomies have success rates up to 97%. Although many studies have reported the clinical success of formocresol pulpotomies, an increasing body of literature has questioned the use of formocresol. (Fuks 2005)
O. Common Complications and Alternative Treatment Plans
Unsuccessful pulpotomy in a primary molar might result in internal resorption progressing into the bone, an inter-radicular pathological lesion, and/or a periapical abscess, with or without a parulis. In most of these situations, the teeth must be extracted.
Self-study Questions
1. Which teeth are good candidates for pulpotomy?
2. What are the contra-indications for a pulpotomy?
3. What are the objectives of a pulpotomy?
4. What are the complications of a pulpotomy failure in a primary molar?
5. What are the desirable characteristics of an ideal pulp dressing?
Answers are located at the end of the case.
Bibliography and Additional Reading
Casas M, Fuks A, 2007, Pulp therapy in primary and young permanent teeth, In: The Handbook of Pediatric Dentistry, American Academy of Pediatric Dentistry, 3rd Edition. Nowak, AJ, Casamassimo, PS (eds), American Academy of Pediatric Dentistry, Chicago, pg. 77–85.
American Academy of Pediatric Dentistry. 2011–2012. Guideline on pulp therapy for primary and young permanent teeth. Reference Manual. pp.212–19.
Fuks AB. 2005. Pulp therapy for the primary dentition. In: Pediatric Dentistry, Infancy Through Adolescence, 4th Edition Pinkham JR, Casamassimo PS, McTigue DJ, Fields HW Jr., Nowak AJ (eds). Elsevier Saunders: St. Louis. pp. 375–93.
SELF-STUDY ANSWERS
1. Teeth with carious or traumatic pulp exposure with transitory thermal and/or chemical stimulated pain, with physiologic mobility, normal soft tissues, no percussion sensitivity (except in cases of food impaction), intact continuous ligament space, and intact periapical and/or furcation bone
2. Teeth with carious or traumatic pulp exposure with spontaneous pain, persistent thermal and/or chemical stimulated pain, pathologic mobility, inflamed soft tissues, parulis, percussion sensitivity, widened and/or discontinuous ligament space, furcation and/or periapical radiolucencies, external and/or progressive internal resorption, dystrophic intrapulpal calcifications, less than one-third physiologic root resorption
3. To maintain tooth vitality and to cause no harm to the succedaneous tooth
4. Unsuccessful pulpotomy in a primary molar might result in internal resorption progressing into the bone, in an inter-radicular pathological lesion, and/or a periapical abscess, />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


