chapter 8
Principles of Pain Diagnosis
Every day, patients seek care for the reduction or elimination of pain. Nothing is more satisfying to the clinician than the successful elimination of the patient’s pain. This elimination is usually the result of some form of therapeutic intervention. Both the patient and clinician therefore tend to focus on the importance of the therapy. The most important part of managing pain, however, is in understanding the problem and establishing a proper diagnosis. It is only through proper diagnosis that the appropriate therapy can be selected. Diagnosis is not easy. Too often it is overlooked or de-emphasized; yet success cannot be achieved without it. This chapter will describe the necessary components for making the proper diagnosis.
The objective of diagnosis is to accurately identify the what, where, how, and why of the patient’s complaint. Pain diagnosis is complicated by some very difficult problems. Pain is a dynamic, changing experience that embraces sensation, emotion, and reaction. Nociception is predominantly subjective in nature, while objective pain behavior reflects consequences as much as cause. A complex pain modulation phenomenon individualizes every painful experience. These characteristics of pain make the diagnosis and management of obscure pains a sobering and sometimes humbling experience for even the most astute clinician.
One difficulty that many clinicians face is his or her mechanistic approach to disease. We are often very “cause” oriented. The “why” in diagnosis, important as it is, may become a stumbling block when dealing with obscure pain, for there may be no cause at all. An understanding that not all pains are somatic is basic to diagnosis. Neuropathic pains and psychologic factors are not always obvious upon examination. The clinician must be cognitive of the biopsychosocial model of disease. On the other hand, if the condition seems related to an actual stimulus of somatic structures, then identification of the cause is essential for proper management.
Another difficulty of which we must be aware is the temptation to assume that the symptoms of which the patient complains represent the real problem that needs to be investigated and managed. Pain behavior consists of audible and visible signals exhibited by the patient that indicate his or her suffering. These signals have filtered down through a chain of modulating influences, not the least of which are the consequences that attend the whole experience. Thus, the complaint as manifested by suffering may bear little relevance to the real underlying problem. Yet it is the suffering itself that the patient presents for treatment.
Diagnosis of a pain complaint consists essentially of three major steps:
- Accurate identification of the location of the structure from which the pain emanates.
- Establishment of the correct pain category that is represented in the condition under investigation. This is a matter of recognizing the clinical characteristics that are displayed. Establishment of the proper pain category is dependent upon a good understanding of the genesis and mechanisms of pain.
- Choice of the particular pain disorder that correctly accounts for the incidence and behavior of the patient’s pain problem. This requires familiarity with the clinical symptoms displayed by pain disorders that occur in the orofacial region.
Preliminary Interview
The initial contact with the patient and discussion of his or her problem are extremely important. Unless satisfactory professional rapport can be initially established, it may be wise to refer the patient before becoming further involved. The rapport on which proper communication must rest requires sincere effort by both patient and clinician. The patient must be willing to honestly and accurately divulge the information that the clinician needs. He or she must do so cooperatively and with a sincere desire to obtain relief from the complaint. If the patient’s intentions and objectives are anything less than this, not only will valuable time and effort be wasted, but chances are, more harm than good will result.
The clinician must feel confident of his or her own competence in the identification and management of pain problems. Any lack of confidence will quickly be sensed by the patient and can destroy the chances of a satisfactory patient-clinician relationship. Moreover, it would be professionally dishonest for a therapist to pursue any course of action for which he felt unprepared. Competence, honesty, patience, and an earnest desire by the therapist to serve the patient are the minimal prerequisites for establishing a satisfactory professional rapport.
At the preliminary interview, sufficient data should be collected to help determine the future course of the examining procedure. Some overall idea of the location, inception, duration, and clinical behavior of the complaint should be obtained. Plans should then be made to either continue the examination, refer the patient to another practitioner, or plan for needed consultations as indicated. Very simple pain problems, such as mucogingival pain of local origin, localized pain due to obvious dental cause, and some cases of typical trigeminal neuralgia, may be solved without extensive examination. More obscure pain complaints justify a carefully planned diagnostic procedure.
It is important to evaluate the patient’s pain in terms of what it means to him or her. This is accomplished by obtaining specific and meaningful descriptors from the patient that accurately describe the complaint. Many patients may not have at their disposal an adequate means of communicating such exact information. In his McGill Pain Questionnaire, Melzack1,2,3,4 arranged descriptive adjectives in several groups. Each series of words is arranged in order of increasing intensity. The patient can be instructed to select one word in each series that best describes the complaint. The first group is composed of sensory descriptors that help describe what the discomfort feels like to the patient.
- Temporal: flicking, quivering, pulsing, throbbing, beating, pounding
- Spatial: jumping, flashing, shooting
- Punctate pressure: pricking, boring, drilling, stabbing, lancinating
- Incisive pressure: sharp, cutting, lacerating
- Constrictive pressure: pinching, pressing, gnawing, cramping, crushing
- Traction pressure: tugging, pulling, wrenching
- Thermal: hot, burning, scalding, searing
- Brightness: tingling, itchy, smarting, stinging
- Dullness: dull, sore, hurting, aching, heavy
- Miscellaneous: tender, taut, rasping, splitting
The second group consists of affective descriptors that yield information about how the patient is reacting to the pain.
- Tension: tiring, exhausting
- Autonomic: sickening, suffocating
- Fear: fearful, frightful, terrifying
- Punishment: punishing, grueling, cruel, vicious, killing
- Miscellaneous: wretched, blinding
The third group is a series of evaluative descriptors that tend to classify the intensity of pain.
- 1. Annoying, troublesome, miserable, intense, unbearable
A fourth group of general descriptors has been added to the questionnaire.
- Spreading, radiating, penetrating, piercing
- Tight, numb, drawing, squeezing, tearing
- Cool, cold, freezing
- Nagging, nauseating, agonizing, dreadful, torturing
Patients who cannot verbalize the description of their complaint may find these descriptors useful.
When the clinician identifies a complex pain complaint, a more thorough evaluation should be accomplished. This evaluation is composed of two major components: the history and the clinical examination. Information gained during the history and examination should allow the clinician to place the pain complaint into the proper pain category so that effective therapy may be selected. Establishment of the proper diagnosis is the most important task accomplished by the clinician and should never be underemphasized, since it is the basis for successful pain management.
The history needs to investigate all aspects of the pain complaint. It should assess the present location of the pain complaint, the time it began, and a detailed description of the pain as initially felt. An evaluation of the early characteristics of the complaint may give valuable clues to its identification prior to modification. Information concerning the duration and clinical course of the complaint with special reference to efforts at treatment is valuable. The general physical and emotional background for the complaint should be noted, as well as the influence of prior trauma, infection, or systemic illness. All medications currently in use should be listed.
The examination should gather information from clinical, radiographic, and laboratory procedures relative to the oral cavity, masticatory system, and regional musculature. Special information derived from diagnostic analgesic blocking, the effect of diagnostic drugs, and trial therapy may also be helpful.
History for Orofacial Pain
An accurate history is the most important aspect in diagnosing obscure pain. It is far more important than the examination. If the clinician will carefully listen, the patient will report the precise pain problem that exists. The patient may use nonmedical terms; nevertheless, the information should allow the clinician to establish a differential diagnosis. The examination can then be used to further clarify the proper pain category or disorder. Much thought should therefore be given to the skillful interviewing of the patient.
History taking can be accomplished in one of two forms: oral or written. An oral history provides some advantages over the written history in that it allows the clinician to meet the patient and establish important rapport. It also allows the patient to express feelings and experiences in his or her own words. The clinician can often gain insight regarding the patient’s feelings concerning past experiences, anger, fear, hostility, and disability. Oral history taking allows the clinician to gain information in a logical sequence, asking appropriate questions as needed. The major disadvantage of the oral history is that it relies heavily on the clinician’s ability to remember all aspects of the history so that no important information is missed. A written history form can eliminate this concern. With a written history form, all important aspects can be included and the patient can fill the form out leisurely in advance of the appointment. Although this type of history is certainly more reliably complete, it may be frustrating to the patient when the questions do not adequately allow him or her to depict the problem.
In many offices both types of histories are used. The written form is completed in advance of the appointment. This is reviewed by the clinician before actually meeting the patient. Then, when the patient is seated, the clinician allows the patient to verbalize the pain complaint while establishing the important doctor/patient rapport. Any confusing items observed in the written history can then be clarified.
Table 8-1 lists important features that should be included in a thorough orofacial pain history. Each item will be discussed in more detail.
The Chief Complaint
A good starting point in history taking is to obtain an accurate description of the patient’s chief complaint. This should first be taken in the patient’s own words and then restated in technical language as indicated. If the patient has more than one pain complaint, each complaint should be noted and when possible placed in a list according to its significance to the patient. Each complaint needs to be evaluated according to each factor listed in the history outline. Once this has been accomplished, each pain complaint should be assessed with respect to its relationship to any of the other complaints. Some complaints may be secondary to another complaint, while others may be independent. An understanding of these relationships is basic to management.
Location of the pain
The patient’s ability to locate the pain with accuracy is diagnostic. However, the examiner should always guard against assuming that the site of pain necessarily identifies the true source of pain, ie, the structure from which the pain actually emanates. The patient’s description of the location of the complaint identifies only the site of pain. It is the examiner’s responsibility to determine whether it is also the true source of the pain. Sometimes, what appears to be adequate cause at the site of pain may mislead both the patient and the doctor, such as visible superficial herpetic lesions or deep tenderness to manual palpation.
It is very helpful to provide the patient with a drawing of the head and neck and ask him or her to outline the location of the pain (Figs 8-1a to 8-1c). This allows the patient to reflect in his or her own way any and all of the pain sites. The patient can also draw arrows revealing any patterns of pain referral. These drawings can give the clinician significant insight regarding the location and even the type of pain the patient is experiencing.
Table 8-1 Features to Include in an Orofacial Pain History
| A. The chief complaint (perhaps more than one) | |||
| 1. Location of the pain | |||
| 2. Onset of the pain | |||
| a. Association with other factors | |||
| b. Progression | |||
| 3. Characteristics of the pain | |||
| a. Quality of the pain | |||
| b. Behavior of the pain | |||
| i. Temporal nature | |||
| ii. Frequency | |||
| iii. Duration | |||
| c. Intensity | |||
| d. Concomitant symptoms | |||
| e. Flow of the pain | |||
| 4. Aggravating and alleviating factors | |||
| a. Physical modalities | |||
| b. Function and parafunction | |||
| c. Sleep disturbances | |||
| d. Medications | |||
| e. Emotional stress | |||
| 5. Past consultation and/or treatments | |||
| 6. Relationship to other complaints | |||
| B. Past medical history | |||
| C. Review of systems | |||
| D. Psychologic assessment | |||
Onset of the pain
It is important to assess any circumstances associated with the initial onset of the pain complaint. These circumstances can give great insight as to etiology. For example, in some instances, the pain complaint began immediately following a motor vehicle accident. Trauma can frequently cause a pain condition, and knowing this not only gives insight as to etiology but also enlightens the examiner to other considerations such as other injuries, related emotional trauma, and possible litigation. The onset of some pain conditions is associated with systemic illnesses or jaw function, or may even be wholly spontaneous. It is important that the patient presents the circumstances associated with the initial onset in chronologic order so that proper relationships can be evaluated.
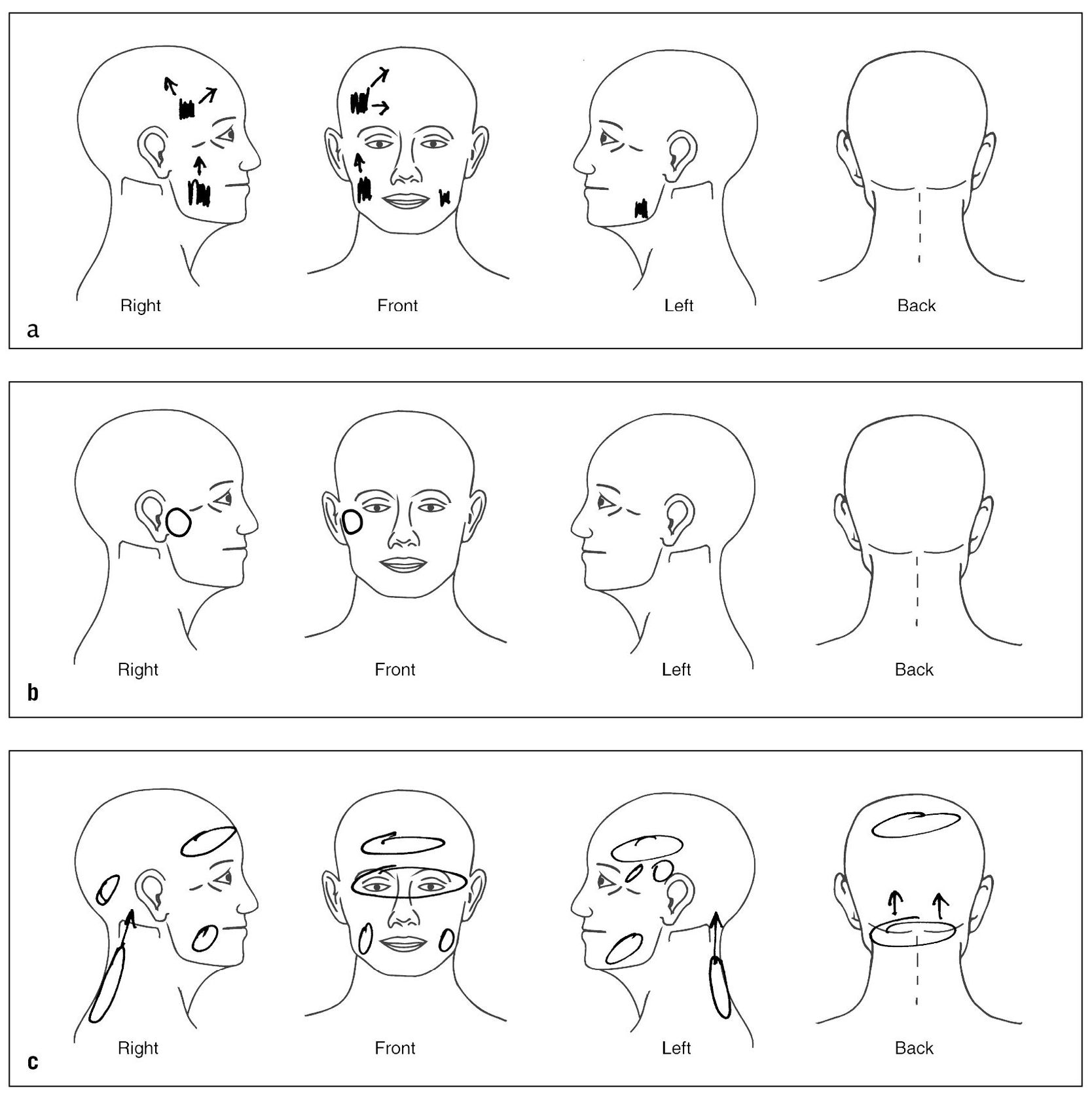
Fig 8-1 Asking the patient to draw the location of the pain and any patterns of referral on a drawing of the head and neck can be very helpful. (a) Example of how a patient with masticatory muscle pain described her pain. Note the broad areas of pain and the radiating patterns of referral. (b) Example of how a patient experiencing temporomandibular joint (TMJ) pain described the location of her pain. (c) Locations of the pain felt by a patient suffering with myofascial pain in the cervical region with referral to the head, initially described as “headache.”
It is equally important to ask the patient what he or she believes caused the pain condition. This may provide great insight into the patient’s view of the pain. In many instances the patient knows precisely what caused the condition. Even if the patient is confused as to cause, the examiner may gain valuable information that is useful in management. For example, this question may reveal anger associated with blame for the pain condition. It is important to know whether the patient believes the pain has been caused by mistreatment or another practitioner. This type of anger may greatly influence future treatment outcome.
Characteristics of the pain
The characteristics of the pain need to be precisely described by the patient, ie, the quality, behavior, intensity, concomitant symptoms, and manner of flow of the pain.
Quality of the pain
The quality of pain should be classified according to how it makes the patient feel. This classification is usually termed bright or dull. When pain has a stimulating or exciting effect on the patient, it is classified as bright. When the pain has a depressing effect that causes the patient to withdraw to some extent, it is classified as dull. It is important that such judgment be wholly independent of pain intensity, variability, temporal characteristics, or any accompanying lancinating exacerbations that may punctuate the basic underlying painful sensation.
Further evaluation of the quality of pain should be made to classify it as pricking, itching, stinging, burning, aching, or pulsating. Many pains, of course, require more than a single designation. Bright, tingling pain is classified as a pricking sensation, especially when mild and stimulating. Superficial discomfort that does not reach pain threshold intensity may be described as itching. As the intensity increases, the pain may take on a pricking, stinging, aching, or burning quality. Deep discomfort that does not reach pain threshold intensity may be described as a vague, diffuse sensation of pressure, warmth, or tenderness. As the intensity increases, the pain may take on a sore, aching, throbbing, or burning quality. When the discomfort has an irritating, hot, raw, caustic quality, it is usually described as burning. Most pains have an aching quality. Some increase noticeably with each heartbeat and are described as pulsating or throbbing.
Behavior of the pain
The behavior of the pain should be evaluated according to frequency or temporal behavior, as well as its duration and localizability.
Temporal behavior reflects the frequency of the pain as well as the periods between episodes of the pain. If the suffering distinctly comes and goes, leaving pain-free intervals of noticeable duration, it is classified as intermittent or episodic. If such pain-free intervals do not occur, it is classified as continuous. Intermittency should not be confused with variability, in which there may be alternate periods of high-level and low-level discomfort. Intermittent pain implies the occurrence of true intermissions or pain-free periods during which comfort is complete. This temporal behavior should not be confused with the effect of medications that induce periods of comfort by analgesic action. When episodes of pain, whether continuous or intermittent, are separated by an extended period of freedom from discomfort, only to be followed by another similar episode of pain, the syndrome is said to be recurrent.
The duration of individual pains during an episode is an important descriptive feature that aids in pain identification. A pain is said to be momentary if its duration can be expressed in seconds. Longer-lasting pains are classified in minutes, hours, or a day. A pain that continues from one day to the next is said to be protracted.
The localization behavior of the pain should be included in its description. If the patient is able to define the pain to an exact anatomic location, it is classified as localized pain. If such description is less well defined and somewhat vague and variable anatomically, it is termed diffuse pain. Rapidly changing pain is classified as radiating. A momentary cutting exacerbation is usually described as lancinating. More gradually changing pain is described as spreading, and if it progressively involves adjacent anatomic areas, the pain is called enlarging. If it changes from one location to another, the complaint is described as migrating. Referred pain and secondary hyperalgesia are clinical expressions of secondary pain.
Intensity of the pain
The intensity of the pain should be established by distinguishing between mild and severe pain. This can be based on how the patient appears to react to the suffering. Mild pain is associated with pain that is described by the patient but without a display of visible physical reactions. Severe pain is associated with significant reactions of the patient to provocation of the painful area. One of the best methods of assessing the intensity of the pain is with a visual analogue scale. The patient is given a piece of paper with a line that has “no pain” written on one end and “the worst possible pain experienced ever” written on the other end. The patient is then asked to place a mark on the location of the line that best describes the pain at that time. A scale of 0 to 5 or 0 to 10 can be used to assess the intensity of the pain, with 0 indicating no pain and 10 indicating the most pain possible. This scale is not only helpful for the initial assessment of pain, but is also useful at follow-up appointments to evaluate the success or failure of therapies.5
Concomitant symptoms
All concomitant symptoms, such as sensory, motor, or autonomic effects that accompany the pain, should be included. Sensations such as hyperesthesia, hypoesthesia, anesthesia, paresthesia, or dysesthesia should be mentioned. Any concomitant change in the special senses affecting vision, hearing, smell, or taste should be noted. Motor changes expressed as muscular weakness, muscular contractions, or actual spasm should be recognized. Various localized autonomic symptoms should be observed and described. Ocular symptoms may include lacrimation, injection of the conjunctivae, pupillary changes, and edema of the lids. Nasal symptoms include nasal secretion and congestion. Cutaneous symptoms may include changes in skin temperature or color, sweating, and piloerection. Gastric symptoms include nausea and indigestion.
Manner of flow of the pain
The manner of flow informs the clinician whether the individual pains are steady or paroxysmal. A flowing type of pain, although it may vary in intensity or be distinctly intermittent, is described as steady. Such pain is to be distinguished from paroxysmal pain, which characteristically consists of sudden volleys or jabs. The volleys may vary considerably in both intensity and duration. When they occur frequently, the pain may become nearly continuous.
Aggravating and alleviating factors
Effect of functional activities
The effect of functional activities should be observed and described. Common biomechanical functions include such activities as movement of the face, jaw, or tongue and the effects of swallowing, head position, and body position. The effect of such activities as talking, chewing, yawning, brushing the teeth, shaving, washing the face, turning the head, stooping over, or lying down should be noted. In addition, the effect of emotional stress, fatigue, and time of day should be recorded.
The pain may be triggered by minor superficial stimulation, such as touch or movement of the skin, lips, face, tongue, or throat. When triggered by such activities, it is well to distinguish between merely incidental stimulation of overlying tissues and stimulation that is the result of functioning of the joints and muscles themselves. The former is true triggering, while the latter is pain induction. This distinction can usually be made by stabilizing the joints and muscles with a bite block to prevent their movement while the other structures are stimulated or moved. If uncertainty exists, the distinction can be made more positively by utilizing local anesthesia. Topical anesthesia of the throat effectively arrests triggering in the glossopharyngeal nerve distribution. Mandibular block anesthesia stops triggering from the lower lip and tongue. Infraorbital anesthesia arrests triggering from the upper lip and maxillary skin. None of these procedures prevents the induction of true masticatory pain.
Parafunctional activities should also be assessed. The patient should be questioned regarding bruxism, clenching, or any other oral habit. One should remember that often these activities occur at subconscious levels and therefore the patient may not report them accurately.
Effect of physical modalities
The patient should be questioned regarding the effectiveness of hot or cold on the pain condition. The patient should be asked whether other modalities, such as massage or transcutaneous electrical nerve stimulation therapy, have been tried, and if so, what the results were. The results of such therapies may shed light on the type of pain condition and its therapeutic responsiveness.
Medications
The patient should report all past and present medications taken for the pain condition. Dosages should be acquired, along with the frequency taken and effectiveness in altering the chief complaint. It is also helpful to know who prescribed these medications, since their input may also shed light on the pain condition.
Emotional stress
As has already been discussed, emotional stress can be a major contributing factor to the pain condition. In some instances, however, emotional stress may not be a major factor but instead an aggravating factor. When this is present, patients will report that although their pain is present at all times it seems to be accentuated during times of increased stress. It is important for both the clinician and the patient to recognize this relationship.
Sleep quality
There appears to be a relationship between some pain conditions and the quality of the patient’s sleep.6,7,8,9,10,11,12,13 It is important, therefore, that quality of sleep be reviewed. Patients who report poor-quality sleep should be questioned regarding the relationship of this finding with the pain condition. Particular notice should be taken when the patient reports waking during the night in pain or when the pain actually wakens the patient.
Litigation
During the interview it is important to inquire whether the patient is involved in any form of litigation related to the pain complaint. This information may help the clinician better appreciate all conditions surrounding the pain. The presence of litigation does not directly imply secondary gains, but this condition may be present.
Psychologic Assessment
As pain becomes more chronic, psychologic factors relating to the pain complaint become more common. Routine psychologic evaluation may not be necessary with acute pain; however, with chronic pain it becomes essential. It may be difficult for the general practitioner to confidently evaluate psychologic factors. For this reason, chronic pain patients are best evaluated and managed by a multidisciplinary approach.
There are a variety of measuring tools that can be used to assess the psychologic status of the patient. Turk and Rudy14 have developed the Multidimensional Pain Inventory (MPI). This scale evaluates three pain profiles: adaptive coping, interpersonal distress, and dysfunctional chronic pain. Dysfunctional chronic pain is a profile of severe pain, functional disability, psychologic impairment, and low perceived life control.
Another useful tool is the Symptom Check List 90 (SCL-90).15 This evaluation provides both a depression scale and a scale measuring the severity of nonspecific physical symptoms (the somatization subscale). Assessment of these factors for a chronic pain patient is essential.
Often the general practitioner may not have immediate access to psychologic evaluation support. In this instance, the practitioner may elect to use IMPATH16 or the TMJ Scale.17,18 These two scales have been developed for use in the private dental practice to assist in evaluating clinical and certain psychologic factors associated with orofacial pains. Although these scales are helpful, they are not as complete as the above psychologic tests and certainly do not replace the personal evaluation of a clinical psychologist.
As discussed in chapters 6 and 7, there are a number of psychologic conditions that can contribute to or actually be responsible for pain disorders. One category of psychologic conditions is the somatoform disorders. These disorders are characterized by complaints of physical symptoms for which there are no demonstrable organic findings or known physical mechanisms. When pain is the chief complaint, this disorder is called a somatoform pain disorder.19 Another type of somatoform disorder is a conversion disorder. The essential feature of this disorder is an alteration or loss of physical functioning that suggests a physical disorder, but instead of the presence of an actual physical disorder, the symptoms are an apparent expression of a psychologic conflict or need. The symptoms are not intentionally produced, yet they cannot be explained by any physical disorder or known pathophysiologic mechanism. A third type of somatoform disorder is hypochondriasis. The essential feature of this disorder is preoccupation with the fear of having—or the belief that one has—a serious disease, based on the patient’s interpretation of physical signs or symptoms as evidence of physical illness.
Psychologic assessment is also important in identifying other mental disorders such as mood disorders (ie, depression) and anxiety disorders (ie, posttraumatic stress disorder). There is also a broad category that includes psychologic factors that are affecting a physical condition. In this category, the psychologic factor may not be significant enough to warrant its own disorder but in fact it does affect an existing condition. This category may likely be the most common psychologic condition associated with chronic orofacial pain disorders.
Psychologic assessment is an essential part of the orofacial pain history. The manner by which it is performed will vary according to the expertise of the clinician. As pain disorders become more chronic, it is best for the clinician to rely on a trained clinical psychologist or psychiatrist for this evaluation.
Clinical Examination for Orofacial Pain
An effective examination form helps the practitioner obtain essential data with the least expenditure of time and effort. Ensuring that such data are complete is important in the identification of pain. An examination form should be as simple and flexible as possible so as to be readily adaptable to the many different pain problems that present themselves.
The purpose of the clinical examination is to identify any variations from the normal health and function of the orofacial structures. The examination should include an assessment of nonmasticatory structures, such as the neurologic status, as well as evaluation of the eyes, ears, and neck. If abnormal findings are identified, an immediate referral to the appropriate specialty is indicated. The examination should also include an assessment of the masticatory structures.
Locating the Source of Pain
Although the history is important in identifying the site of pain, it is the examination that is most helpful in locating the true source of the pain. The clinician should always be suspicious of heterotopic pains, since they are so common in the orofacial structures. Remember, for therapy to be effective, it must be directed toward the source of pain, not the site. Of course, this is no problem if the pain is primary pain, since both the site and source are in the same location. If, however, the pain is referred, this presents an interesting twist. When referred pains are present, the clinician may often have a tendency to direct therapy to the site of pain as directed by the patient. Of course this type of therapy will fail, since it will not affect the cause of the pain. The astute pain clinician will always be suspicious of referred pain and will always clinically confirm the source of the pain.
Primary pains can be differentiated from referred pains by their characteristics during local provocation (Fig 8-2a). Remember, referred pains are wholly dependent upon the original source of the pain. Therefore, when a source of pain is located during an examination, palpation of the source will not only increase the pain at the source but will also likely increase the pain at the referred site (Fig 8-2b). If palpation of the site of pain does not increase the pain, one should be suspicious of a referred site of pain. If the information gained during the examination is not complete enough to identify the pain, then selective local anesthetic blocking of selected tissues may be needed. Local anesthetic blocking of the site of pain will not decrease the pain, since it does not interrupt the true source of the pain (Fig 8-2c). On the other hand, when the source of pain is anesthetically blocked (Fig 8-2d), the pain will be reduced not only at the source, but also at the site. When the clinician is confused regarding the true source of the pain, local anesthetic blocking should be used. In some instances it may be the only way to locate the true source of pain. Pain therapists need to be familiar with the various local anesthetic blocks used in the head and neck. These will be discussed later in this chapter.
The following four rules summarize the examination techniques used to differentiate primary pain from referred pain:
- Local provocation of the site of pain does not increase the pain.
- Local provocation of the source of pain increases the pain, not only at the source but also at the site.
- Local anesthetic blocking of the site of pain does not decrease the pain.
- Local anesthetic blocking of the source of pain decreases the pain at the source as well as the site.
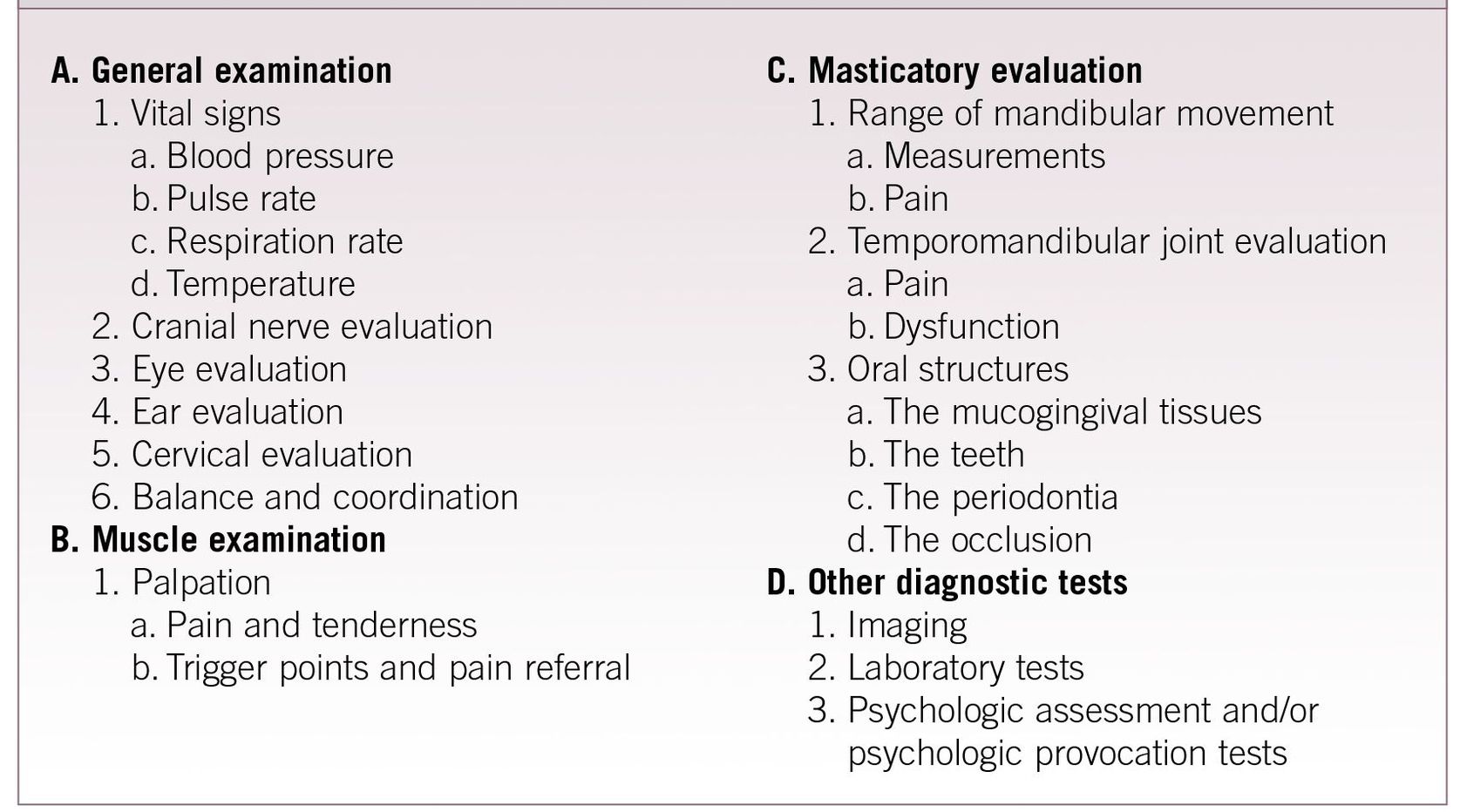
An orofacial pain examination should thoroughly evaluate all structures of the orofacial region. Table 8-2 provides a summary of a comprehensive examination.
General Examination
Cranial nerve evaluation
The 12 cranial nerves supply sensory information to and motor impulses from the brain. Any gross problem relating to their functions must be identified so that abnormal conditions can be immediately and appropriately addressed. The orofacial pain therapist does not need to be trained as a neurologist. In fact, a cranial nerve examination need not be a complex evaluation. Any clinician who regularly evaluates pain problems can test the gross function of the cranial nerves to evaluate for any neuropathic disorders. Each nerve can be assessed with the following simple evaluation procedures.
Olfactory nerve
The first cranial nerve has sensory fibers originating in the mucous membrane of the nasal cavity and provides the sensation of smell. It is tested by asking the patient to detect differences between the odors of peppermint, vanilla, and chocolate. (It is helpful to have these available in the office for testing.) It must also be determined whether or not the patient’s nose is obstructed. This can be done by asking the patient to exhale nasally onto a mirror. Fogging of the mirror from both nostrils indicates adequate air flow.
Optic nerve
The second cranial nerve, also sensory, with fibers originating in the retina, provides for sight. It is tested by having the patient cover one eye and read a few sentences. The other eye is checked in the same manner. The clinician assesses the visual field by standing behind the patient and slowly bringing the fingers from behind around into view (Fig 8-3). The patient should report when the fingers first appear. There normally will be no variation between when they are seen on the right and on the left.
Figs 8-2a to 8-2d Proper examination procedures are necessary to identify the true source of the pain. When one is unsure of the source of pain the following sequence should be followed.
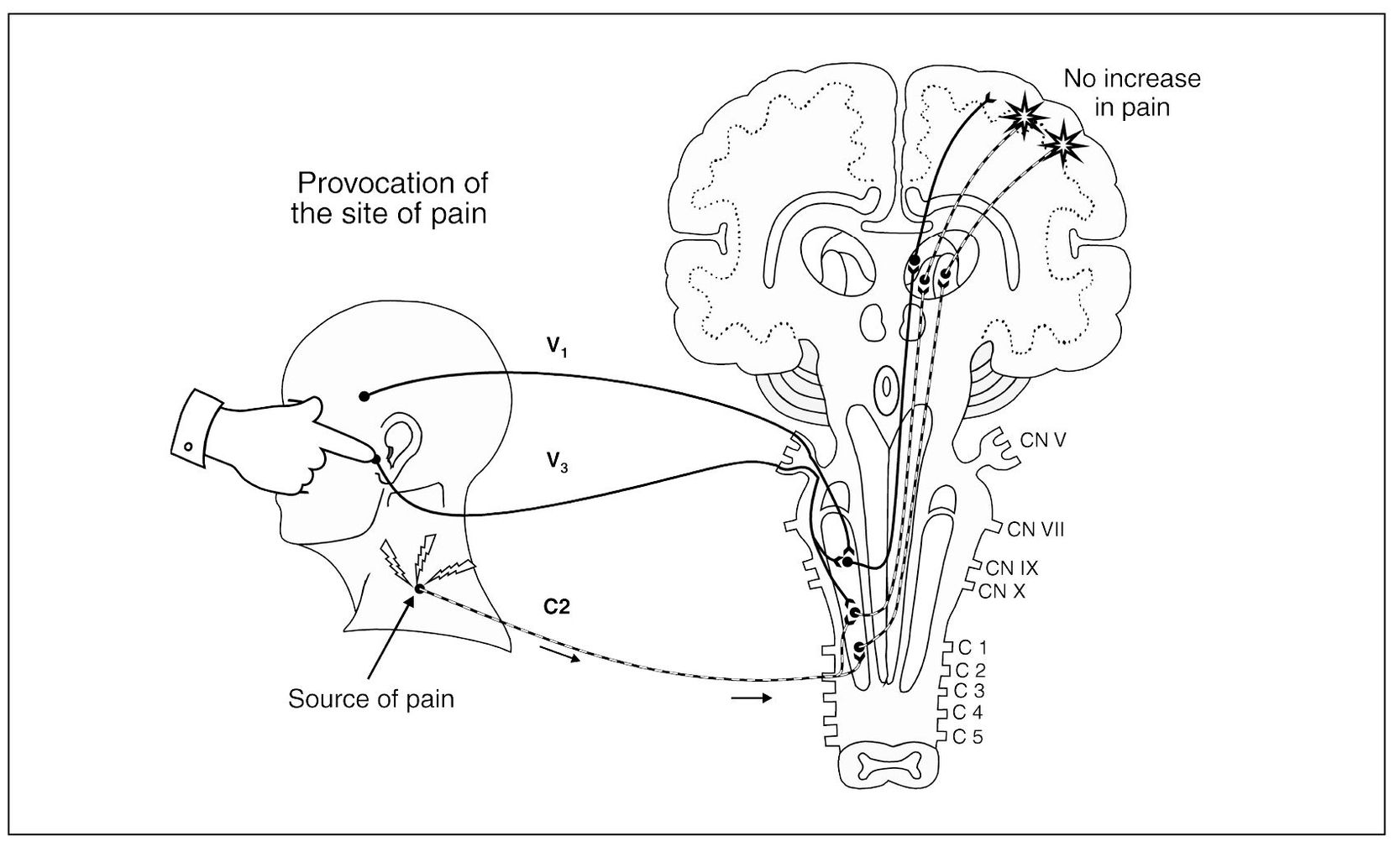
Fig 8-2a Provocation of the site of pain does not increase the pain.
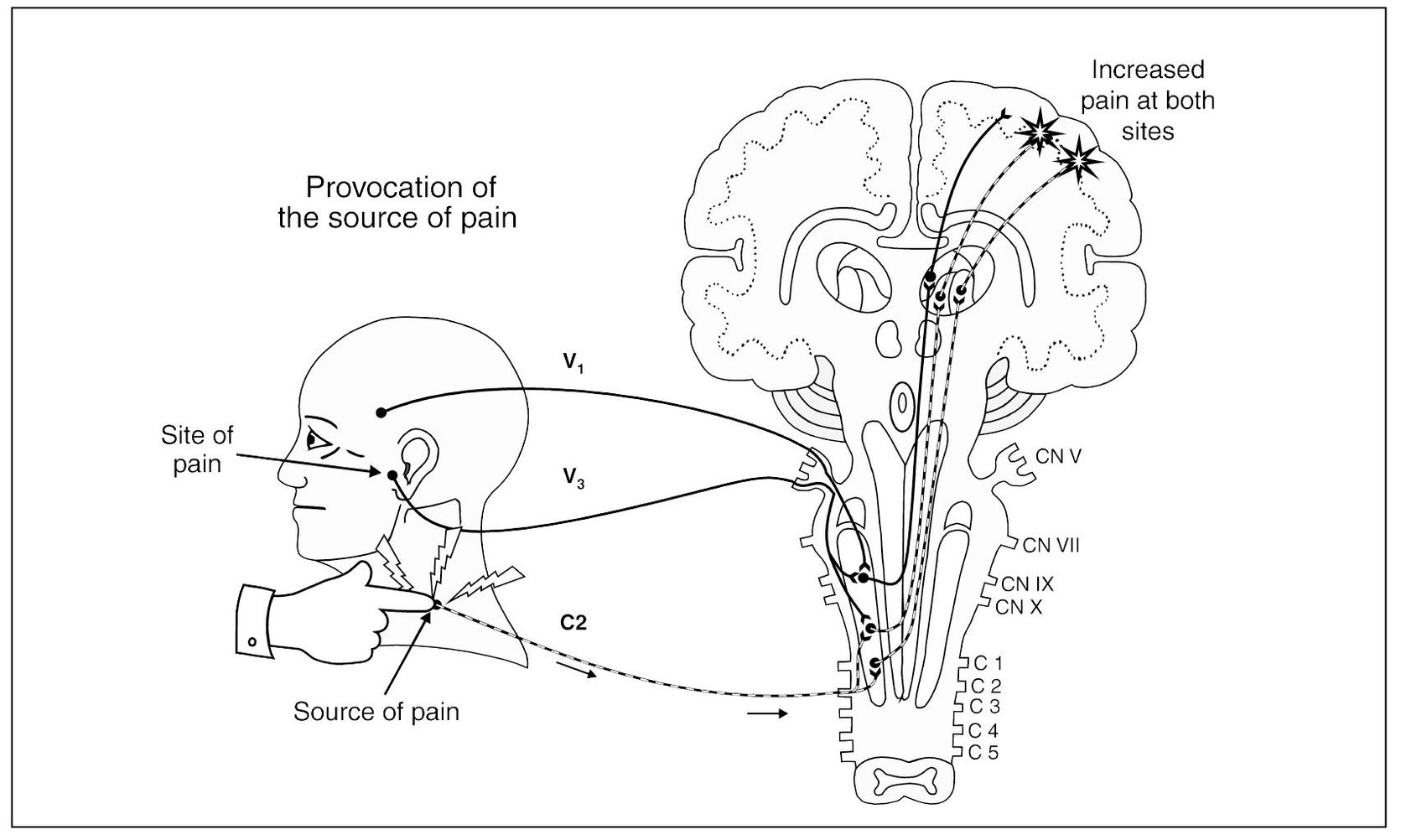
Fig 8-2b Provocation of the source of pain increases the pain, not only at the source but also at the site.
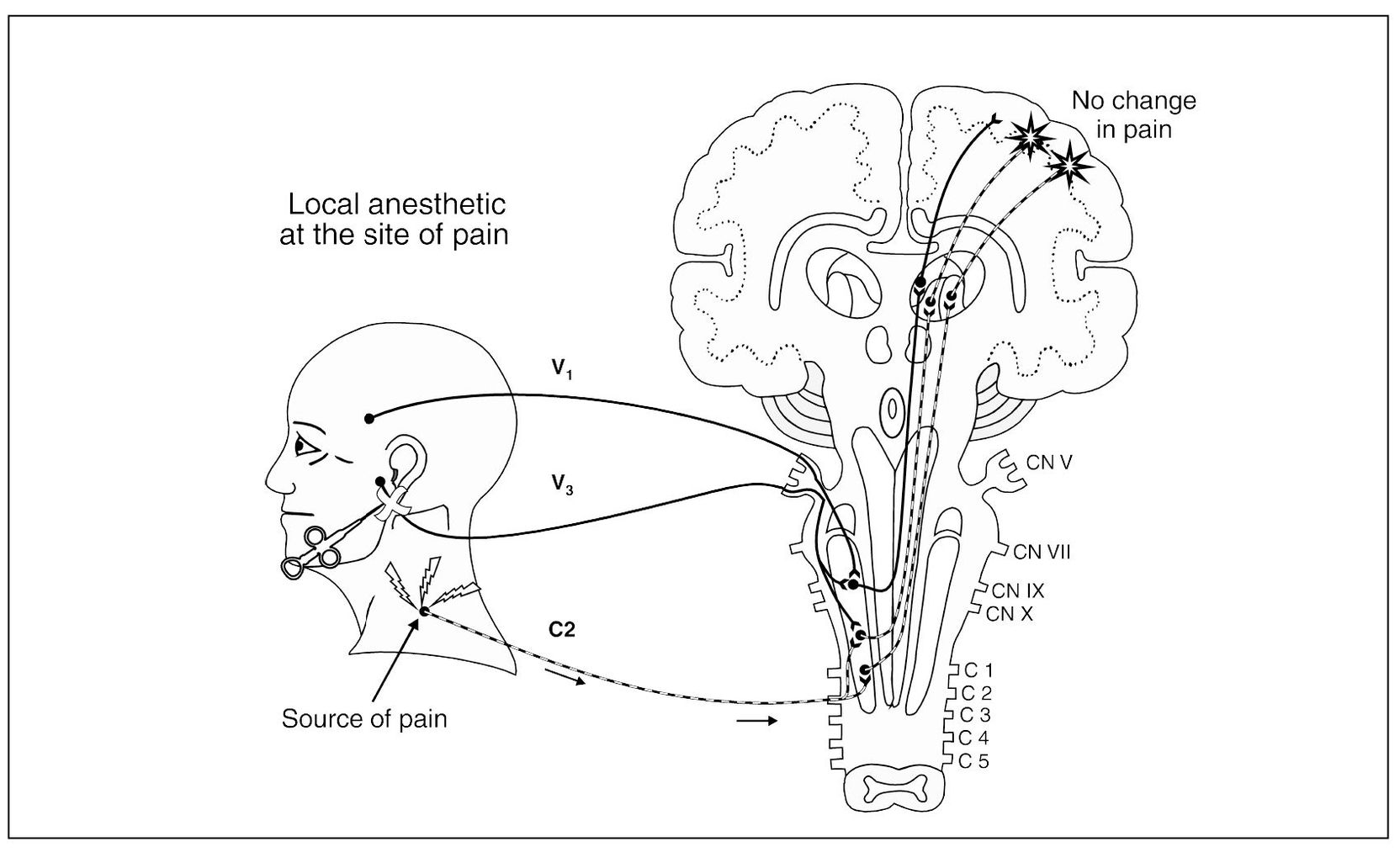
Fig 8-2c Local anesthesia at the site of pain fails to reduce the pain.
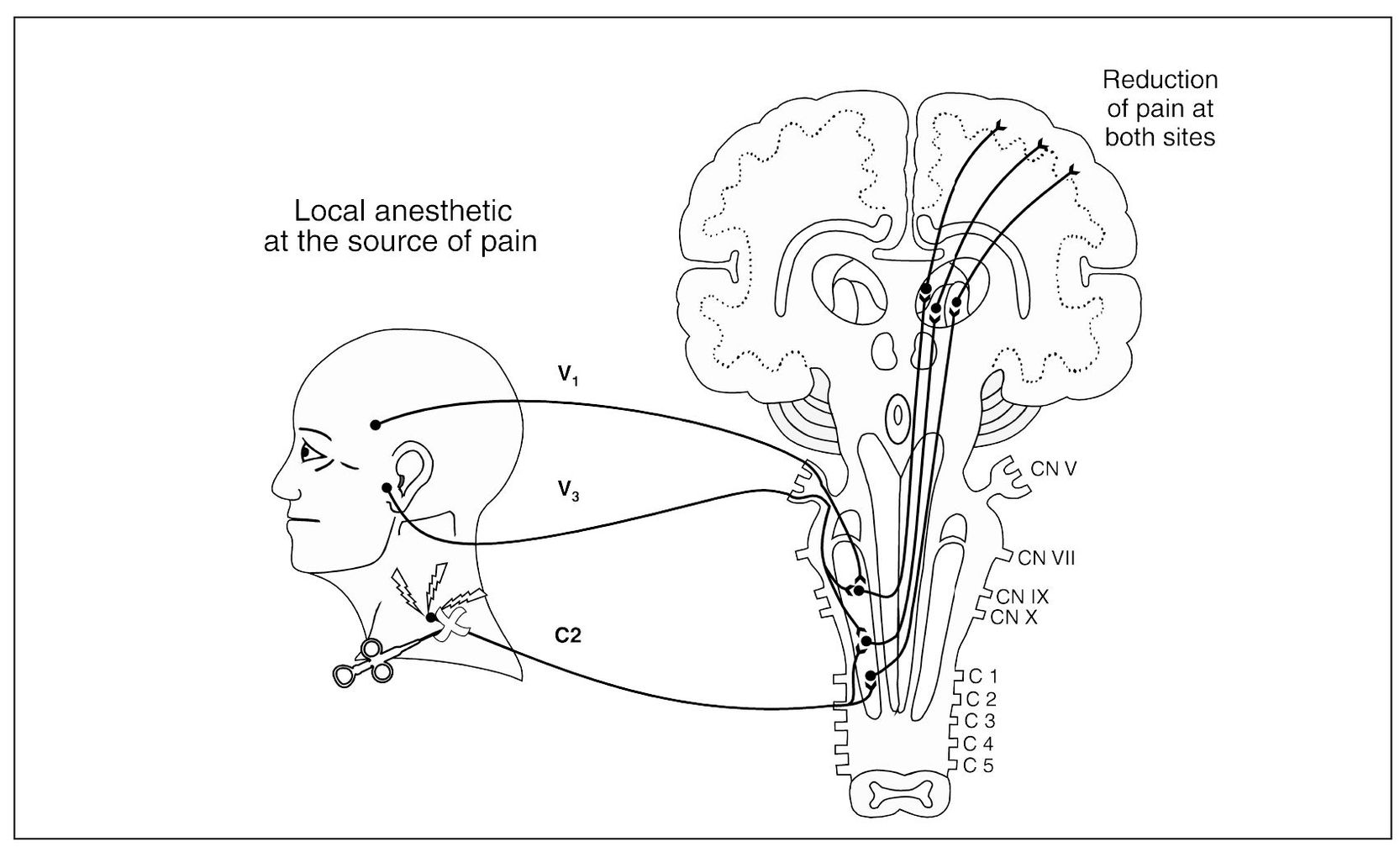
Fig 8-2d Local anesthesia at the source of pain reduces the pain at the source as well as the site.
Table 8-2 Summary of a Comprehensive Clinical Examination
Oculomotor, trochlear, and abducent nerves
The third, fourth, and sixth cranial nerves, which supply motor fibers to the extraocular muscles, are tested by having the patient follow the clinician’s finger as the clinician makes an X (Fig 8-4). Both eyes should move smoothly and similarly as they follow the finger. The pupils should be of equal size and rounded and should react to light by constricting. The accommodation reflex is tested by having the patient change focus from a distant to a nearby object. The pupils should constrict as the object (the finger) approaches the patient’s face. Not only should they both constrict to direct light, but each should also constrict to light directed in the other eye (consensual light reflex) (Fig 8-5).
Trigeminal nerve
The fifth cranial nerve is both sensory (from the face, scalp, nose, and mouth) and motor (to the muscles of mastication). Sensory input is tested by lightly stroking the face with a cotton tip bilaterally in three regions: forehead, cheek, and mandible (Fig 8-6). This will give a rough idea of the function of the ophthalmic, maxillary, and mandibular branches of the trigeminal nerve. The patient should describe similar sensations on each side. The trigeminal nerve also contains sensory fibers from the cornea. The corneal reflexes can be tested by observing the patient’s blink in response to light touch on the cornea with a sterile cotton pledget or tissue. Gross motor input is tested by having the patient clench while the clinician feels both masseter and temporal muscles (Fig 8-7). The muscles should contract equally bilaterally.
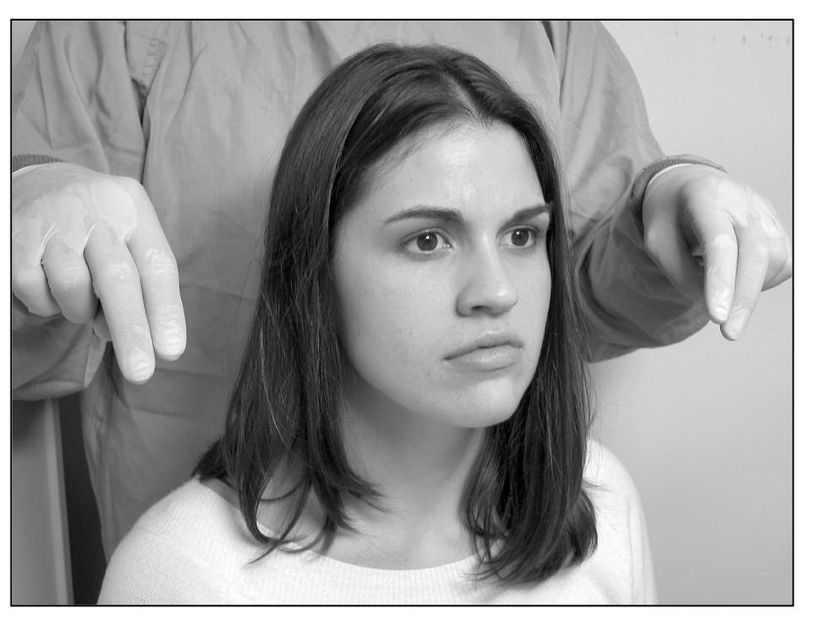
Fig 8-3 Checking the patient’s visual field (optic nerve): With the patient looking forward, the examiner’s fingers are brought around to the front from behind. The initial position at which the fingers are seen marks the extent of the visual field. Right and left fields should be very similar.
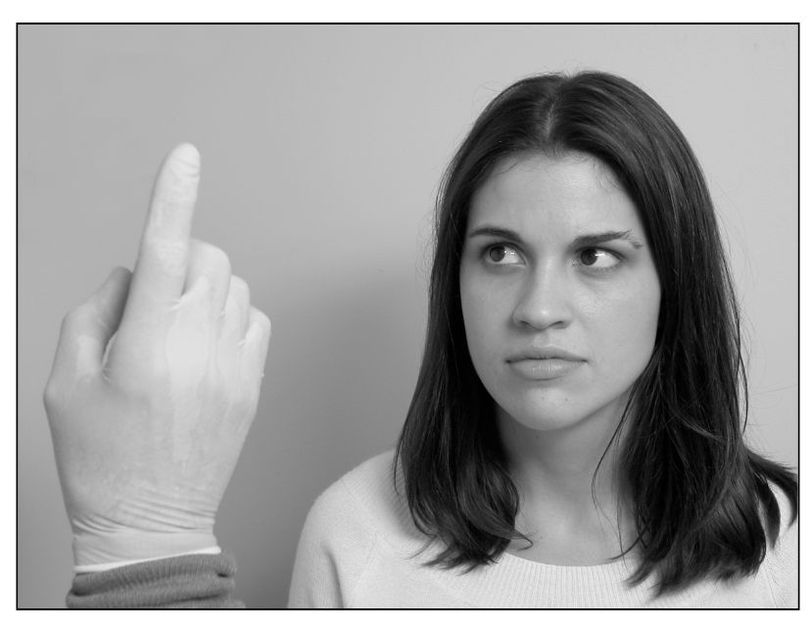
Fig 8-4 Checking the patient’s extraocular muscles: Without moving the patient’s head, the examiner asks the patient to follow the finger as it makes an X in front of the patient. Any variation in right or left eye movement is noted.

Fig 8-5 Constriction of the pupil can be seen when light is directed toward the eye. The opposite pupil should also constrict, demonstrating the consensual light reflex.
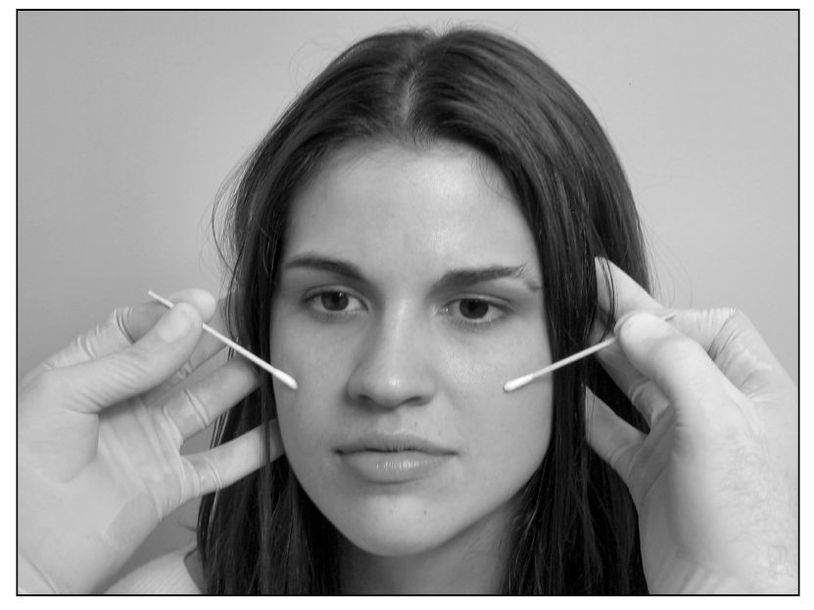
Fig 8-6 Cotton tip applicators can be used to compare discrimination of light touch between the right and left maxillary branches of the trigeminal nerve. The ophthalmic and mandibular branches are also tested.

Fig 8-7 Motor function of the trigeminal nerve to the masseter muscles is tested by asking the patient to clench the teeth together while the examiner feels for bilateral contraction.

Fig 8-8 Gross hearing can be evaluated by asking the patient if she can hear the sound of rubbing a strand of hair between the finger and thumb. Any difference in hearing between the right and left ear is noted.
Facial nerve
The seventh cranial nerve also is sensory and motor. The sensory component, which supplies taste sensations from the anterior portion of the tongue, is tested by asking the patient to distinguish between sugar and salt using just the tip of the tongue. The motor component, which innervates the muscles of facial expression, is tested by asking the patient to raise both eyebrows, smile, and show the lower teeth. During these movements, any bilateral differences should be recorded.
Acoustic nerve
Also called the vestibulocochlear nerve, the eighth cranial nerve supplies the senses of balance and hearing. The patient should be questioned regarding any recent changes in upright posture or in hearing, especially if they were associated with the problem that initiated the office visit. If there is a question regarding balance, the patient should be asked to walk heel-to-toe along a straight line. Gross hearing can be evaluated by rubbing a strand of hair between the first finger and thumb near the patient’s ear and noting any difference between right and left sensitivities (Fig 8-8).
Glossopharyngeal and vagus nerves
The 9th and 10th cranial nerves are tested together because they both supply fibers to the back of the throat. The patient is asked to say “ah,”’ and the soft palate is observed for symmetric elevations. The gag reflex is tested by touching each side of the pharynx.
Accessory nerve
The spinal accessory nerve supplies fibers to the trapezius and sternocleidomastoid muscles. The trapezius is tested by asking the patient to shrug the shoulders against resistance. The patient is then asked to tilt the head to one side while the clinician resists the movement (Fig 8-9). The sternocleidomastoid is tested by having the patient look first to the right and then to the left against resistance. Any differences in muscle strength between sides should be noted.
Hypoglossal nerve
The 12th cranial nerve supplies motor fibers to the tongue. To test it, the patient is asked to protrude the tongue and note any uncontrolled or consistent lateral deviation is noted. The strength of the tongue can also be evaluated by having the patient push laterally against a tongue blade.

Fig 8-9 The spinal accessory nerve is tested by asking the patient to move the head laterally to one side against resistance. The examiner assesses for equal muscle strength between the right and left sides.
Autonomic function
The parasympathetic functioning of the oculomotor (third cranial) nerve has already been checked by testing pupillary accommodation to light. That of the facial (seventh cranial) and glossopharyngeal
(ninth cranial) nerves can be checked by lacrimation and salivation. The parasympathetic functioning of the vagus (10th cranial) nerve can be checked by testing the carotid sinus reflex by which the heart rate is reduced in response to pressure on the internal carotid artery at the level of the cricoid cartilage. A deficit in cranial sympathetic functioning is recognized by the presence of Horner syndrome, which presents with narrowing of the palpebral fissure, ptosis of the upper lid, elevation of the lower lid, constriction of the pupil, and facial anhidrosis.
Superficial reflexes
The corneal reflex has already been tested by closure of the eyelids in response to irritation of the cornea by touching with a sterile cotton applicator. It involves afferent impulses transmitted by the trigeminal (fifth cranial) nerve and efferent motor impulses via the facial (seventh cranial) nerve. The palatal reflex is involuntary swallowing in response to stimulation of the soft palate. It involves afferent impulses transmitted by the trigeminal (5th cranial) and glossopharyngeal (9th cranial) nerves and efferent motor impulses via the glossopharynge/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


