chapter 18
Psychologic Factors and Orofacial Pain: Axis II
In recent years, the advancement of medical science has been phenomenal. We know more today about disease processes then ever before. As we study a disease and begin to understand the mechanisms responsible for its development, we learn ways of interrupting its progression, thereby terminating the disease. This new knowledge has certainly improved the health and well-being of the human race. This processing of information, however, can pose some interesting conflicts in the understanding and management of pain.
Most of the medical community has a belief that every disease has a physical condition associated with it. Once the physical condition that is responsible for the disease is found, it can be corrected and the disease is terminated. This mechanistic model of disease makes complete sense for some diseases, such as pulpitis. When a caries lesion nears the dental pulp, the pulpal tissues become inflamed and painful symptoms begin. If the caries lesion is removed and the pulpal tissue recovers, the symptoms resolve. The successful management of this type of pulpal disease occurs every day in the practice of dentistry. If removal of the caries lesion does not resolve the pain symptoms, it is assumed that the pulpal tissues are necrotic and a new therapy (endodontics) is performed. When this disease process is present, the removal of the pulp eliminates the painful symptoms. These clinical findings reinforce the physical cause-and-effect (mechanistic) approach to treating pulpal pain. Since pulpal pain fits this model so well, it perfectly supports the mechanistic approach to disease.
Taking this example one step further, however, helps demonstrate the limitations of the mechanistic model of disease. Assume that after the endodontic procedure was completed on the tooth, the pain continued. The mechanistic approach would suggest that the endodontic therapy has failed, even though no clinical evidence of failure exists, and the tooth would logically be extracted. Unfortunately, after extraction of the tooth, the pain continues. Since there is no longer evidence of disease, the mechanistic approach to the disease fails to explain the pain. It is at this time the clinician will often blame the pain on some psychologic factor. Since the condition is now psychologic, the clinician who is not trained in the management of psychologic issues will likely feel inadequate and without any treatment strategies. A common occurrence at this time is for the clinician to brand the patient as neurotic. This type of thinking greatly limits the clinician’s ability to manage pain.
Every clinician who manages pain needs to appreciate that no pain is without some influence of psychologic factors. As nociception enters the brainstem, it ascends to the higher centers for interpretation and evaluation. As it reaches the thalamus, the nociceptive input is influenced by neural interaction between the limbic structures, the cortex, and the hypothalamus. It is at this level that the nociceptive input is given meaning. The limbic structures add instincts, drives, and emotions to the input. The cortex adds the influence of prior experiences and present environmental conditions to the input. The hypothalamus prepares the body to react to the input through responses of the autonomic nervous system (eg, blood pressure, heart rate, vigilance). It is this unique response at the thalamic level that makes the experience of pain so individual and personal. It is at this level that one can begin to understand why the experience of pain is dependent upon the attention drawn to the injury and the consequence of the injury (see chapter 1).
As discussed in chapter 1, nociception is merely the mechanism by which noxious information is carried into the central nervous system (CNS). Pain is an unpleasant sensation perceived in the cortex, usually as a result of incoming nociceptive input. The presence or absence of nociceptive input, however, does not always relate closely to pain. The term suffering refers to still another phenomenon. Suffering refers to how the human reacts to the perception of pain. It is at this level that the complex interaction of the cortex, thalamus, hypothalamus, and limbic structures becomes evident. Suffering, therefore, may not be proportionally related to nociception or pain. Patients experiencing little pain may suffer greatly, while others with significant pain may suffer less. Pain behavior is something different still. Pain behavior refers to the individual’s audible and visible actions that communicate his suffering to others. Pain behavior is sometimes the only observed evidence the clinician receives regarding the pain experience. This behavior is as individual as people themselves.
When one appreciates the complexity of the pain experience, it becomes evident that the mechanistic model of disease is inadequate in the management of pain conditions. A more suitable model is the biopsychosocial model of disease (Fig 18-1). The “bio” represents the nociceptive input arising from the somatic tissues and the “psychosocial” component represents the influence of the interaction between the thalamus, cortex, and limbic structures. It is interesting to note that the neurotrans-mission of impulses between all these higher centers is responsible for what we call the psychologic aspects of pain. In fact, like all neural functions, psychologic factors and moods are based on neurotransmitter activity. Although some clinicians cling to the notion that psychologic activity somehow operates independently of somatic structures, there is a preponderance of evidence that points to an organic neural basis for all such activity. Receptors, neurons, synapses, electric charges, and neurochemicals are the structural elements that underlie all functional activities, psychologic as well as physiologic. Neurochemistry seems to be the key to such mechanisms. As mentioned in chapter 5, psychology could be construed as actually neurology that is not yet fully understood. No doubt, as these mechanisms are better understood, we shall know a great deal more about suffering and pain behavior.
It is with this appreciation of pain that a dual-axis classification of orofacial pain has been developed for this text. Axis I represents those conditions that have a physical basis, while Axis II represents those conditions with a psychosocial basis. A detailed review of Axis I conditions was presented in chapters 9 through 17. The clinician must appreciate that each Axis I diagnosis is likely to be influenced by the presence of an Axis II diagnosis. For complete patient management, the presence and influence of each axis must be accessed for proper diagnosis. In some pain conditions, treatment of only the Axis I factors will fail to manage the patient’s complaints. Unfortunately, this concept is foreign to many health professionals.
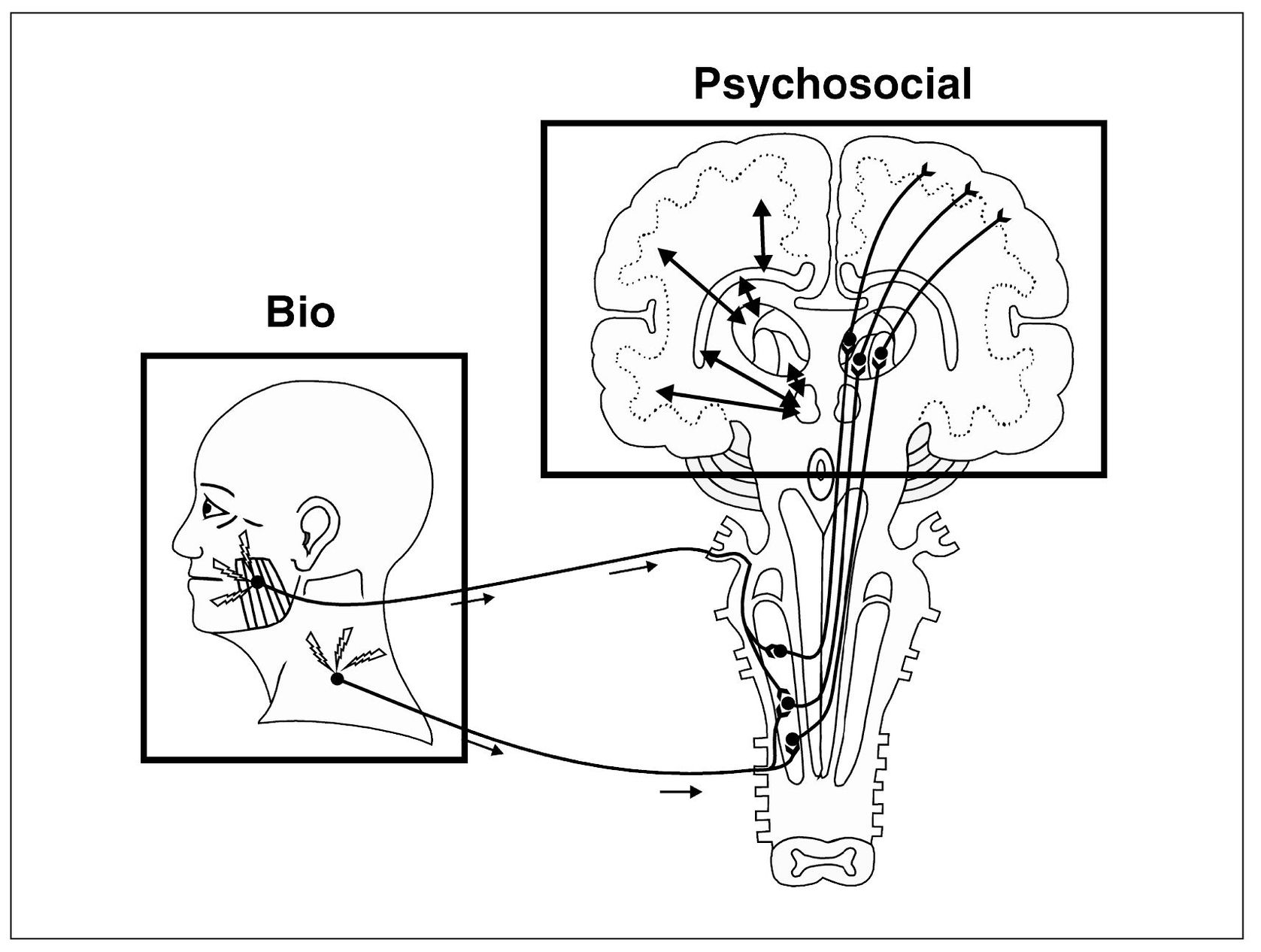
Fig 18-1 A graphic depiction of the biopsychosocial model of disease. Nociceptive input arises from the masseter and the trapezius muscles. This input represents the “bio” portion of model. Once the nociceptive input enters the CNS and ascends to the higher centers, the interaction of the thalamus, limbic structures, hypothalamus, and cortex interrupts the input and labels it as painful or not. This higher center interaction represents the “psychosocial” portion of the model. Both areas are likely to be of equal importance in the pain experience.
Acute Pain Versus Chronic Pain and the Biopsychosocial Model
As discussed in chapter 5, acute pains are of short duration and are often closely related to somatic tissue changes, such as those produced by trauma or disease. Chronic pain refers to pains of long duration, and these pains take on a different therapeutic meaning. Most clinicians use the term to describe any pain that has lasted longer than 6 months, regardless of its origin. Although this is the classic definition, perhaps a better concept of chronic pain would be pains that last longer than normal healing time. It is expected that tissue damage will produce nociception and pain, but when healing is complete, pain should subside. If pain continues after normal healing time, the origin of the pain is in doubt. One reason for continued pain is the influence of the Axis II psychologic factors. As pain becomes protracted, a shift in the origin of the pain can be expected from primary somatosensory input to the affective, cognitive, and behavioral inputs of pain. As the duration of pain input continues, the level of suffering increases, even when the intensity of somatosensory input remains the same (Fig 18-2). In fact, chronic pain can be sustained at high level of discomfort, even though the intensity of the somatosensory input may decrease or disappear altogether. As pain becomes chronic, management options shift from local to systemic modalities. Pain that could initially be managed on a purely Axis I level may require extensive and coordinated interdisciplinary therapy to be effective.
When considering the effects of acute and chronic pains within the biopsychosocial model, one realizes that early in the pain experience the somatosensory input (bio) often has the greatest influence on the pain experience. As pain becomes protracted, the influence from the higher centers (psychosocial) will likely become predominant. As already stated, this has therapeutic significance.
Psychologic intensification of pain is a normal modulating effect peculiar to humans and has to do with their evaluation of the consequences attending the experience. All pains are subject to some degree of intensification. It is only when psychogenic factors (Axis II) dominate the complaint that it becomes a significant therapeutic consideration. Since duration increases pain intensification, a component of Axis II factors become an ingredient in the development of chronicity.
Another element that appears to be important in the development of chronic pain is the continuity of nociceptive input. Intermittency lessens the likelihood of the development of pain chronicity, as is seen in such conditions as trigeminal neuralgia and migraine. Even though they persist and recur indefinitely, such disorders usually do not change appreciably in their response to therapy and therefore are not likely maintained by Axis II factors. Pain disorders that have a constant input, even if it is of variable high and low intensity, are more likely to develop symptoms of chronicity. A combination of duration and continuity of nociceptive input predisposes a patient to pain chronicity.
In the past, the term atypical facial pain was used to categorize a group of patients who had chronic facial pain of unknown etiology. In a study of 34 cases of chronic atypical facial pain, Mock et al1 reported that all of the patients displayed nonanatomic distribution with no identifiable organic or physiologic cause and complained of symptoms that were not compatible with any known neurologic syndrome. Of the 34 patients, 76.5% were women. More than 50% had undergone some dental treatment for the pain that made it worse rather than better. Some 38% reported a sensory complaint such as anesthesia, paresthesia, or hyperesthesia; 55% had headaches; and 73% had associated depression, anxiety, or a highly stressed state. Of course these findings would be expected by definition in a population of patients classified as having atypical facial pain. It would appear that this general classification should diminish as the profession becomes more knowledgeable of orofacial pain mechanisms. For this reason, the term atypical facial pain will not be used in this text.
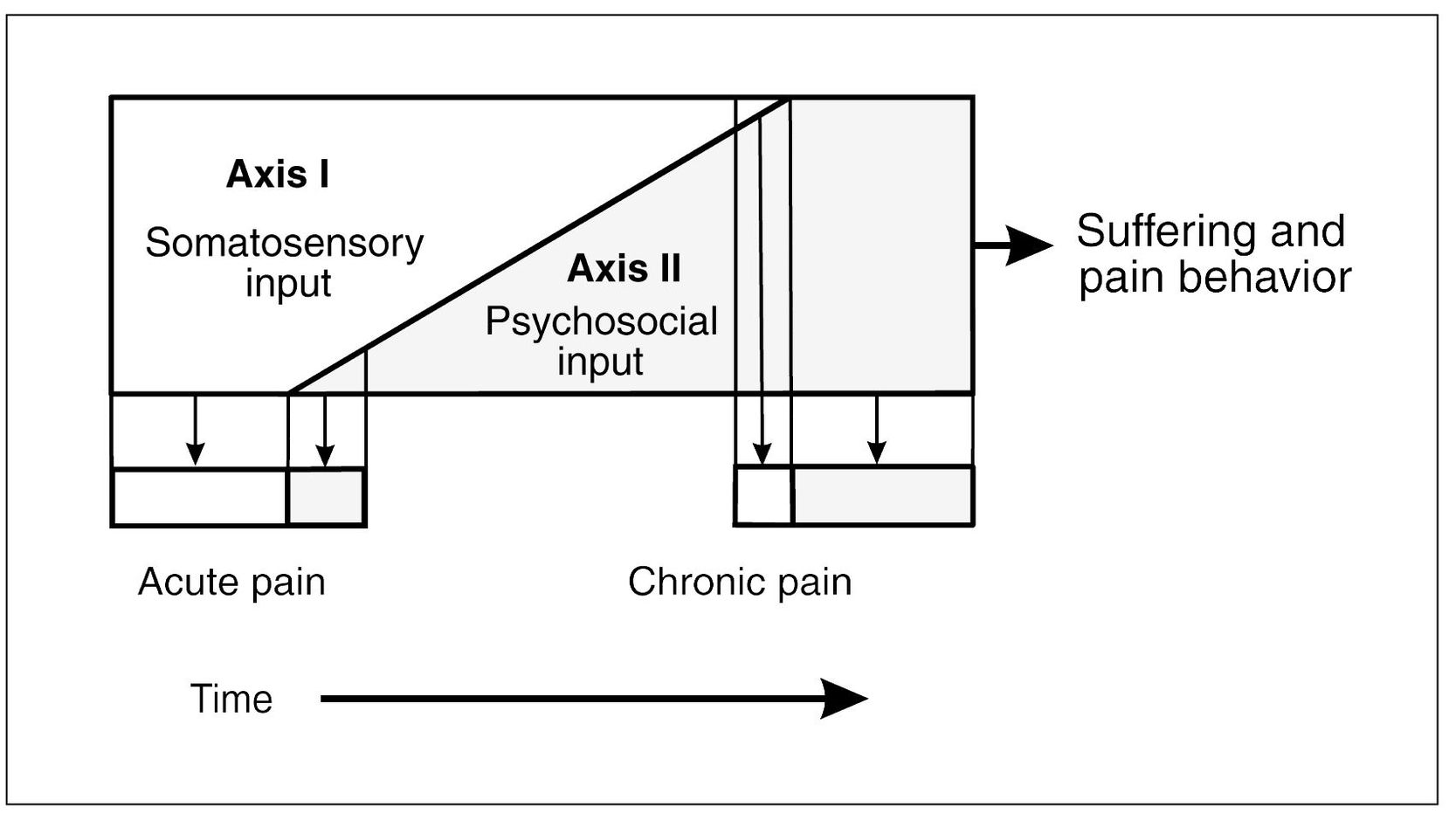
Fig 18-2 Axis I input represents the somatosensory (bio) input that contributes to the patient’s pain and suffering. Axis II represents the psychosocial input that contributes to pain and suffering. Both Axis I and Axis II factors must be considered when evaluating a patient’s pain and suffering. Early in the pain experience, Axis I input often dominates the degree of pain and suffering. As the condition becomes chronic, Axis II factors often become the dominant input. An understanding of this relationship is important in therapy.
It is important to note that pain experienced in the orofacial structures may be significantly related to Axis II factors. In a review2 of 430 patients with psychogenic regional pain, the head and heart regions were the most frequent sites of pain. In a study of 40,000 patients with orofacial pain,3 2% to 5% had no organic disease or had exaggerated responses to minimal pathologic conditions. It was noted that depressive illness occurred especially with glossodynia, glossopyrosis, recalcitrant masticatory pain, and atypical facial pain. In one clinic that treated chronic pain patients of all types,4 40% complained of chronic craniofacial and neck pains. In these patients, there were few or no signs of Axis I pathosis, or it was not consistent with the degree of discomfort. The characteristics that these patients displayed included the following:
- A high level of stress expressed as anxiety and depression
- A marked tendency toward tolerance, dependence, and addiction, not only to medications but also to surgery and treatments of all kinds
- A marked dependency on family, friends, and doctors
- Evidence of loss of self-esteem, impotence, apathy, regressive attitude, and withdrawal behavior
- Hostility
Moulton5 identified two types of patients with chronic pain: (1) people who were overtly dependent on someone who was either inadequate, overdominant, or unapproachable and thus became angry and hostile; and (2) unusually competent people who were obsessive and domineering and therefore became hostile secretly. The author warned that local treatment in patients with chronic pain may serve to focus their attention on the area treated, with the result that they would continue to seek relief on a purely peripheral level thereafter.
Beck et al6 associated depression with glossodynia, myofascial pain, and atypical facial pains. They listed the symptoms of mild depression as disappointment, lack of self-confidence, and feelings of inadequacy; a desire to be alone and inactive; undue concern for physical appearance; decreased mental and physical alertness; and loss of weight and disturbed sleep. They listed the symptoms of severe and potentially suicidal depression as apathy, self-hate, despondency, immobility, poor posture, decreased muscle tone, insomnia, and fatigue.
Fordyce7 pointed out that pain behavior, which consists of audible and visible communications that imply suffering, is subject to the influence of conditioning or “learning.” Examples of such conditioning are (1) the effect of imitating the behavior of others who suffer (social modeling); (2) the reinforcement of the “reality” of pain by medications prescribed to be used as needed, as well as by the attention received from others because of suffering; and (3) the indirect reinforcement of pain by avoidance of obligations, commitments, or duties to escape or minimize pain. Pain behavior that is contingent upon expectancy or secondary gain may be reinforced by cues in the environment that suffering may be imminent when actually no noxious stimulation is ever sensed. It may be necessary only to anticipate that pain may occur for overt pain behavior to be displayed.
Sternbach8 observed that subjective improvement in a patient’s pain condition follows behavioral improvement. This suggests that pain responses change if the state of mind changes. Thus, if the pain behavior of chronic pain patients is acquired or learned, it may be unlearned by proper techniques. Chronic pain is modifiable through coping strategies.
Roberts9 attempted to control chronic pain by focusing on the patient’s behavior and not on the source of nociception nor on an attempt to change an alleged emotional state. His objective was to rehabilitate the patient rather than to alleviate the pain. He believed that it is better to teach the patient to live a normal life, even though pain may still be present. In chronic pain disorders, treatment measures that are aimed only to alleviate pain tend to reinforce the “pain concept” that the patient holds.
It should be noted that in patients with chronic pain, the endorphin system does not offer protection of any importance.10 Perhaps the experience of chronic pain depletes the CNS of these pain modulators. Although the action of tricyclic antidepressants in normal subjects has no greater effect on the pain threshold than does placebo,11 in depressed individuals the analgesic effect parallels the antidepressant action.12
The Psychologic Significance of Orofacial Pains
All pains carry with them certain importance and meaning. As already mentioned, the attention drawn to the injury and the consequence of the injury directly determine the degree of suffering experienced by the patient. This concept is extremely important when addressing facial pain. The clinician should never forget the significant psychologic meaning of pain in this portion of the body. The face and mouth are the primary structures needed for survival. Without these, the individual will not be able to take in food. These structures are basic to life itself. Damage or significant loss of function is a significant threat to the individual.
The orofacial structures are also basic to communication. In our social environment, where communication is so vital, dysfunction of these structures threatens meaningful existence. These structures provide the means by which we relate to others our feelings, goals, opinions, and aspirations. They are a source of gratification and satisfaction physically, emotionally, spiritually, and sexually. When these structures are threatened by pain or dysfunction, the quality of life can greatly diminish.
Not only do the mouth and face have unusual emotional significance for the individual, but they also relate to concepts of body image, in that the individual interprets a damaged face as a damaged self. Distortion of body image results in anxiety that is frequently expressed as pain.13 This is likely to have an important bearing on the severity and duration of chronic post-traumatic pain syndromes of the maxillofacial region. This trauma may be not only that of actual tissue damage to the face, but also that of emotional trauma such as that associated with physical or sexual abuse.14,15,16,17,18,19,20
It is wise for the clinician to always be mindful of the unique emotional significance of the orofacial structures. The clinician should always approach the patient with care and respect, never too quickly or abruptly. The successful clinician learns the appropriate examination and management style that gains the confidence of the patient.
Axis II: Classification of Mental Disorders
Understanding the complex neurologic interaction between the thalamus, cortex, hypothalamus, and limbic structures is indeed a difficult task. Dysfunction of this neural interaction results in what are referred to as mental disorders. The study of mental disorders encompasses an enormous body of information. The main purpose of this text is to provide information to the clinician regarding orofacial pain disorders. Although the Axis II conditions described as mental disorders are enormously important, they cannot be reviewed completely in this text. This author has therefore limited the discussion in this chapter to a few of the more important mental disorders that may involve orofacial pain conditions. For a thorough discussion of mental disorders, a review of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), published by the American Psychiatric Association,21 is recommended.
There are four general categories of mental disorders that will be reviewed in this chapter. The description of each disorder will be in accord with the DSM-IV21 publication. The categories that will be discussed are mood disorders, anxiety disorders, somatoform disorders, and a broad category that includes other conditions that may be a focus of clinical attention. Each of these categories will be divided into important subcategories and will be discussed strictly for the purpose of identification and not treatment. It is important for the dental clinician and physician to recognize these conditions so that optimum therapy is provided by appropriate health care personnel.
Mood Disorders
Mood disorders are mental disorders that are characterized by disturbances in the patient’s mood. Mood disorders are divided into three categories: depressive disorders, bipolar disorders, and mood disorders resulting from a medical condition (Fig 18-3).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


