Preventive and Intermediary Materials
Prevention is a foundation of dentistry. Low-level fluorides in water supplies have provided tremendous benefit in reducing the incidence of dental caries in children. Fluorides can be introduced into community water supplies to ensure systemic ingestion during early life, when the teeth are forming. Fluoride can also be provided as a dietary supplement to inhibit caries where drinking water is not fluoridated. Patients who are at high risk for developing caries in spite of receiving systemic fluoride can be given various topical applications such as toothpastes, mouth rinses, gels, and varnishes. A combination of systemic and topical fluoride applications has contributed to a dramatic reduction in the prevalence of smooth surface caries over the past 50 years. Pits and fissures on the occlusal surfaces of posterior teeth, however, are more resistant to fluoride uptake because of the irregular morphology of the occlusal surface. This, combined with the retention of food and the difficulty of proper brushing in the posterior segment, can lead to the start of a carious lesion. A preventive therapy consisting of a sealant to fill in the irregularities can reduce the risk of caries by creating a smoother surface that is easier to clean and less likely to retain food and harbor bacteria.
Pit and Fissure Sealants
The most common sealants are based on Bis-GMA resin and are light cured, although some self-cured products are still available. The expanded name for Bis-GMA is 2,2-bis[4(2-hydroxy-3-methacryloyloxy-propyloxy)-phenyl] propane. The chemistry of Bis-GMA sealants is the same as that described for resin composites in Chapter 9. The principal difference is that sealants are much more fluid to enable them to penetrate the pits, fissures, and etched areas on the enamel, which promote retention of the sealant. The viscous Bis-GMA resin is mixed with a diluent, such as triethylene glycol dimethacrylate, to produce a reasonably low viscosity, flowable resin. An alternative but similar oligomer base is urethane dimethacrylate; some materials are formulated from a combination of the two base resins. To provide stiffness to the material and improve wear resistance, filler particles of fumed silica or silanated inorganic glasses can be added to form low-viscosity composites.
Light-Cured Sealants
Today, most sealants are light cured, activated by a diketone and an aliphatic amine. The complete reactions for resin composites are given in Chapter 9. Light-cured sealants are supplied in light-tight containers and should have a shelf-life of more than 12 months. The sealant is applied to the pit and fissure with an appropriate applicator and is cured by exposing it to light for 20 seconds, with the end of the light source positioned about 1 to 2 mm from the surface. Sealants are applied in thin sections so depth of cure should be adequate with 20-second exposure times, even for opaque materials. The advantage in using a light-cured sealant is that the working time can be completely controlled by the operator.
Air Inhibition of Polymerization
During polymerization there is a surface layer of air inhibition that varies in depth with different commercial products. Sufficient material must be applied to completely coat all pits and fissures with a layer thick enough to ensure complete polymerization after removal of the tacky surface layer. The uncured, air inhibited, layer can be easily removed after curing using an abrasive slurry of pumice, applied on a cotton pellet or with a prophylaxis cup in a rotary handpiece. This is more effective than wiping or rinsing.
Properties of Sealants
Reports of the physical properties of sealants are scarce because specimen preparation with such low-viscosity materials is difficult. Because sealants are completed circumscribed by enamel and are not subjected to occlusal stresses, the mechanical properties of sealants are less important than those for resin composite restoratives. By adding ceramic or glass filler particles up to 40% by weight, as in the restorative composites, all properties except tensile strength show improvement. The modulus of elasticity shows the most dramatic improvement, and the increased rigidity makes the filled material less subject to deflection under occlusal stress. Filler is also added with the hope of improving wear resistance and making the material more visible on clinical inspection (Figure 8-1).
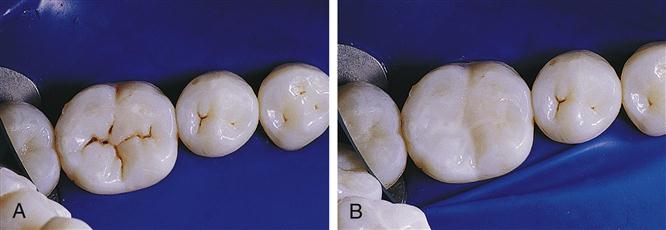
A, Before sealing, and B, after sealing with a natural-colored sealant material. (From Hatrick CD, Eakle WS, Bird WF: Dental materials: clinical applications for dental assistants and dental hygienists, ed 2, Saunders, St. Louis, 2011.)
Optimal adhesion of the sealant to enamel occurs when the sealant has a high surface tension, good wetting, and a low viscosity. These properties permit the sealant to flow easily along the enamel surface. The surface wettability is demonstrated by the contact angle of a drop of liquid on the enamel surface. A drop that spreads readily produces a low contact angle. This highly wetted surface is conducive to a strong adhesive bond. Polymer tags form when the resin flows into the surface irregularities created by acid etching and are responsible for the mechanical bond that retains the sealant to enamel. Functional durability of the sealant bond is related to stresses induced by shrinkage of the resin during curing, thermal cycling, deflection from occlusal forces, water sorption, and abrasion, with total failure manifested by the clinical loss of material.
Sealant materials have a variety of features that must be selected carefully by the healthcare provider. Most current materials are light-cured rather than self-cured because of the ease and controlled rate of cure. Tooth-colored or clear resins are available that are very natural looking on the tooth surface, but they are also available in opaque or tinted materials to make the recall examination process easier (Figure 8-2). A new class of color-reversible, photosensitive sealants has recently been developed. They are very similar to the light-cured sealants in resin composition and filler loading. In addition, photosensitive pigments are added that are normally colorless but change to green or pink when exposed to the dental curing light. The color change lasts for about 5 to 10 minutes after exposure, to help determine whether the sealant adequately covers the pit and fissures. The color change can be repeated at recall visits with another exposure to a dental curing light.
An increasing number of sealants are marketed with the claim that they release fluoride. The release is highest in the first 24 hours after placement and then tapers to a low maintenance level, which may or may not be sufficient to provide extended clinical protection against caries.
Clinical Studies
Many clinical studies using Bis-GMA resins have been documented. In earlier studies on effectiveness of treatment with sealant in newly erupting teeth, a light-cured sealant demonstrated a retention rate of 42% and an effectiveness of 35% in caries reduction after 5 years. In a similar study, a filled resin sealant showed a retention rate of 53% and a clinical effectiveness of 54% after 4 years. Results involving a quicker-setting unfilled resin sealant with very good penetration showed a retention rate of 80% and an effectiveness of 69% after 3 years. The longest published study on sealant effectiveness is a 15-year evaluation of a self-cured unfilled material, which showed 27.6% complete retention and 35.4% partial retention.
In pair-wise comparisons, the treated first molars had 31.3 decayed and filled primary tooth surfaces (dfs) and the untreated controls had 82.8 dfs. In a more current 4-year study comparing a fluoride-releasing sealant with one that did not have fluoride, retention rates were 91% for the fluoride material (77% complete and 14% partial) and 95% for the nonfluoride sealant (89% complete and 6% partial). Although the retention was somewhat lower in the fluoride-containing sealant, the caries incidence for both groups was identical (10%). In a study conducted in private practice, the 2-year retention rates for two newer fluoride-containing resins were greater than 90%, and no caries was detected on the test teeth. In a continuing study with retreatment of all defective sealant surfaces at 6-month recalls, the teeth were maintained caries-free for a 5-year period. The retreatment rate was highest (18%) at 6 months, and then diminished as time progressed, but at each recall period at least two teeth (about 4%) required reapplication.
Almost all studies show a direct correlation between sealant retention and caries protection. Therefore, it is important to use materials that are retentive to enamel, resistant against occlusal wear, and easily applied with minimal opportunities for surface contamination. Current evidence indicates that sealants are most effective on occlusal surfaces where pits and fissures are well defined and retentive to food and in patients with elevated risk for pit and fissure caries.
Application of Sealants
The handling characteristics of a sealant depend on the composition of the material and the surface to which it is applied. Optimal preparation of both aspects will lead to close adaptation of the sealant to the tooth enamel, a strong seal against the ingress of oral fluids and debris, and long-term material retention.
Enamel Surface Preparation
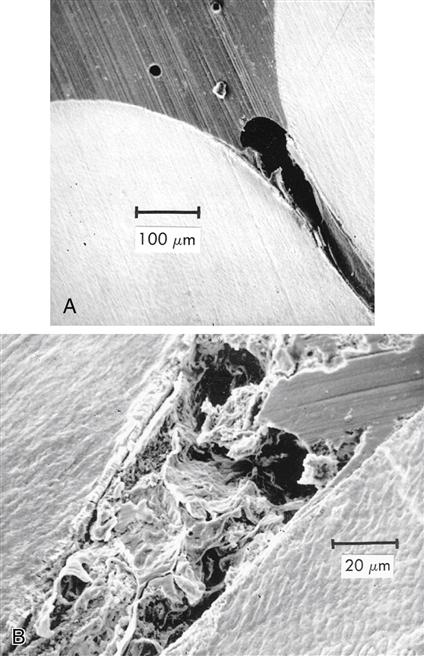
The penetration of any of the sealants to the bottom of the pit is important. The wettability of the enamel by the sealant is improved by etching, and some advocate pretreatment with silanes in solution. Filling the pit or fissure without voids is critical. Air or debris can be trapped in the bottom of the fissure that prevents it from being completely filled, as shown in Figure 8-3. Control of the viscosity of the sealant is important to obtain optimum results. The viscosity determines the penetration of resin into the etched areas of enamel to provide adequate retention of the sealant. Penetration of sealant, forming tags, to a depth of 25 to 50 μm is shown in Figure 8-4.
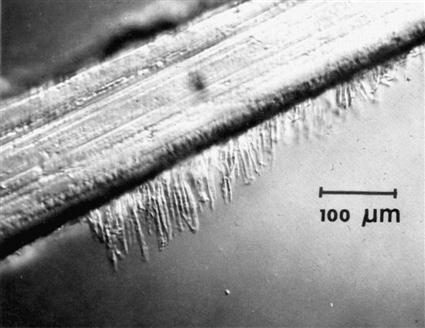
These tags are responsible for the bonding to enamel. (From Gwinnett AJ: J. Am. Soc. Prevent. Dent. 3,21, 1973.)
Etching the pit and fissure surface for a specified time (15 to 30 seconds is adequate for enamel with a normal mineral and fluoride content) with a solution or a gel of 35% to 40% phosphoric acid is recommended. The acid etchant should be flushed thoroughly with water, and the area dried with warm air. Inadequate rinsing permits phosphate salts to remain on the surface as a contaminant, interfering with bond formation. The enamel surface should not be rubbed during etching and drying because the roughness developed can easily be destroyed. Isolation of the site is imperative throughout the procedure to achieve optimum tag formation and clinical success. If salivary contamination occurs during the treatment, the surface should be rinsed and the etch reapplied. On clinical inspection, acid-etched enamel should appear white and dull with an obviously rough texture. If the appearance is not uniform, an additional 30 seconds of etching should be done. The etched area should extend beyond the anticipated area for sealant application to secure optimum bonding along the margin and reduce the potential for early leakage, but without extensive overcoverage. A light-cured bonding agent (see Chapter 13) placed on the freshly etched enamel before placing the sealant will improve retention.
Single step etching and priming systems appear to provide a weaker bond to uncut enamel than to cut enamel walls and bevels.
Sealant Application
Depending on its viscosity and setting time, the sealant may best be applied with a thin brush, a ball applicator, or a syringe. A buildup of excess material should be avoided because it could interfere with the occlusion. A sufficient amount of material should be placed to completely cover all exposed pits and provide a smooth transition along the inclines of the enamel cusps. Overworking of even the light-cured sealants on the tooth surface during application can introduce air voids that appear later as surface defects.
The air-inhibited surface layer should be wiped away immediately after curing and the coating inspected carefully for voids or areas of incomplete coverage. Defects can be covered at this time by repeating the entire reapplication procedure, including the acid etch, and applying fresh sealant only to those areas with insufficient coverage. After the sealant is applied and fully cured, the occlusion should be checked and adjusted if necessary, to eliminate premature contacts.
Glass Ionomers as Sealants
Because of their demonstrated ability to release fluoride and provide some caries protection on tooth surfaces at risk, glass ionomers have been suggested and tested for their ability to function as a fissure sealant. Glass ionomers are generally viscous, and it is difficult to gain penetration to the depth of a fissure. Their lack of penetration also makes it difficult to obtain mechanical retention to the enamel surface to the same degree as with Bis-GMA resins. They are also more brittle and less resistant to occlusal wear. Clinical studies using various formulations of glass ionomers have shown significantly lower retention rates than resin sealants but greater fluoride deposition in the enamel surfaces. Thus there is a greater potential for latent caries protection after sealant loss.
In areas where high-risk children do not have access to definitive treatment, a conservative caries management technique can seal remaining caries in a fluoride-rich environment and establish some degree of remineralization. Atraumatic restorative treatments (ARTs) involve opening a lesion, removing soft surface decay, and filling or sealing the surface with highly filled glass ionomer with a fast setting time. Future studies in this area may produce a new generation of sealant materials noted for their fluoride deposition rather than their mechanical obturation.
Flowable Composites as Sealants
Low-viscosity composites referred to as flowable composites are marketed for a wide variety of applications, such as preventive resin restorations, cavity liners, restoration repairs, and cervical restorations. The properties of flowable composites are described in Chapter 9.
Flowable composites are usually packaged in syringes or in compules (Figure 8-5) for direct application to the pit or fissure. As with lower viscosity resin sealants, trapping of air in the sealant must be avoided. Because they have higher filler content than most resin sealants, flowable composites should have better wear resistance. Flowable composites appear to provide good retention and caries resistance after 24 months.
When flowable composites are used as preventive restorations, their low viscosity is a benefit in extending the restoration into adjacent fissures as a sealant. Long-term clinical efficacy of flowable composites as preventive resin restorations is yet to be established.
Glass Ionomers to Prevent the Progression of Caries
The final materials that need to be considered for caries control and prevention are glass ionomers and hybrid ionomers (resin-modified glass ionomers). Because of their documented slow release of fluoride, glass ionomers are used in cervical restorations when esthetics is not critical. They are specifically recommended for patients with high caries risk (Table 8-1). A detailed description of glass ionomer chemistry can be found in Chapter 9.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses