Paediatric dentistry II
Chapter Contents
Overview
This chapter covers dental trauma, dental anomalies and the special needs of medical, physical and intellectual disability.
Increased knowledge of the pathophysiology of dental trauma has resulted in an improvement in the standard of care for traumatised teeth and an increase in the prognosis for such teeth. Teeth that would have been extracted in the recent past can now often be maintained in function during adolescence and early adulthood. The category of special needs has increased with successful scientific advances in paediatric medicine and surgery. More children now survive previously fatal illnesses. However, they often do so with either direct oral and dental side-effects of the original illness or its treatment or with significant risk of morbidity or mortality from oral or dental infection.
8.1 Traumatic injuries
Traumatic injuries to teeth and jaws can occur at any age. They are, however, very common in children. Boys have twice as many injuries as girls in both the primary and permanent dentitions. The majority of injuries affect the maxillary incisors. The most common types of injury are:
Peak injury times occur at 2–4 years in the primary dentition when a young child is exploring and becoming adventurous and 7–10 years in the permanent dentition owing to falls when playing. At age 5 years, 31–40% of boys and 16–30% of girls will have injured their teeth. The respective figures at age 12 years are 12–33% and 19%.
Assessment
Classification
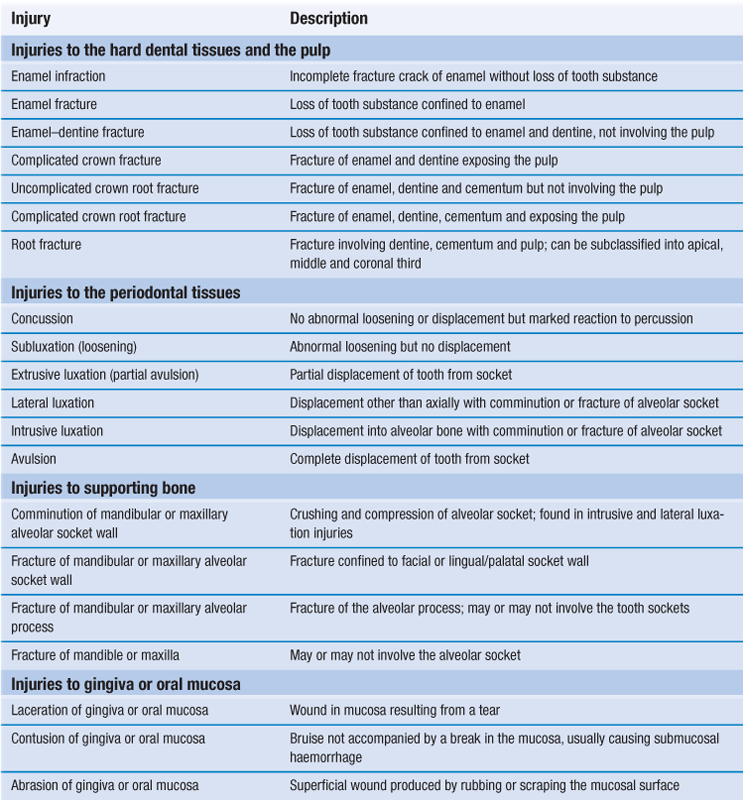
Table 8.1 summarises the classification of dento-alveolar injuries based on the World Health Organization (WHO) system.
History
Dental history
When did injury occur?
The time interval between injury and treatment significantly influences the prognosis of avulsion, luxations, crown fractures (with or without pulpal exposures) and dento-alveolar fractures.
Where did the injury occur?
May indicate the need for tetanus prophylaxis.
How did the injury occur?
The nature of the accident can yield information on the type of injury expected. Discrepancy between history and clinical findings raises suspicion of non-accidental injury (NAI).
Lost teeth/fragments?
If a tooth or fractured piece cannot be accounted for when there has been a history of loss of consciousness, then a chest radiograph should be obtained to exclude inhalation.
Concussion, headache, vomiting or amnesia?
Brain damage must be excluded and referral to a hospital for further investigation organised.
Previous dental history?
Previous trauma can affect pulpal sensibility tests and the recuperative capacity of the pulp and/or periodontium. In addition, for a child, is the child injury prone or are there suspicions of NAI? Previous treatment experience, age and parental/child attitude will affect the choice of treatment.
Medical history
Congenital heart disease, rheumatic fever or severe immunosuppression are contraindications for prolonged endodontic treatment with a persistent necrotic focus. Endodontic treatment should be under antibiotic cover, at least during extirpation and working length calculation.
Bleeding disorders must be of prime concern if there is soft tissue laceration, avulsion or luxation, or if extractions are required.
Allergies require a suitable alternative antibiotic if necessary.
Tetanus status may lead to referral for tetanus toxoid booster (if no previous infection in the last 5 years).
Extraoral examination
Swelling, bruising or lacerations may indicate underlying bony and tooth injury. Lacerations require careful debridement to remove foreign bodies. Crown fracture with associated lip swelling and a penetrating wound may suggest fragment retention in the lip.
Intraoral examination
Examination must be systematic and include recording of lacerations, haemorrhage and bruising as well as abnormalities of tooth occlusion, displacement, fractures or cracks. Tooth examination should include:
• mobility assessment: possible root fracture, displacement, dento-alveolar fracture
• percussion: duller note may indicate root fracture
• colour: early change seen on palatal or gingival third of crown
• thermal with warm gutta-percha or ethyl chloride
• notoriously unreliable, never use in isolation from other clinical and radiographic data
Radiographic examination
Periapical radiographs
Reproducible ‘long cone technique’ periapicals are the best for accurate diagnosis and clinical audit. Two radiographs at different angles may be essential to detect a root fracture. However, if access and co-operation are difficult, one anterior occlusal radiograph rarely misses a root fracture.
Occlusal radiographs
To detect fractures and foreign bodies within the soft tissues:
Orthopantogram
An orthopantogram is essential in all trauma. It may detect unsuspected underlying bony injury. Other views include:
Primary dentition
During its early development, the permanent incisor is located palatally to, and in close proximity with, the apex of the primary incisor. With any injury to a primary tooth, there is risk of damage to the underlying permanent successor.
The most accident prone time is between 2 and 4 years of age. Realistically, this means that few restorative procedures will be possible and in the majority of children the decision is between extraction or maintenance without extensive treatment. A primary incisor should always be removed if its maintenance will jeopardise the developing tooth bud.
A traumatised primary tooth that is retained should be assessed regularly for clinical and radiographic signs of pulpal or periodontal complications. Radiographs may even detect damage to the permanent successor. Soft tissue injuries in children should be assessed weekly until healed. Tooth injuries should be reviewed every 3–4 months for the first year and then annually until the primary tooth exfoliates and the permanent successor is in place.
Crown fractures
Uncomplicated crown fracture
This is treated either by smoothing sharp edges or by restoring with an acid-etch restoration if co-operation is satisfactory.
Complicated crown fracture
Normally, extraction is the treatment of choice. However, pulp extirpation and canal obturation with zinc oxide cement, followed by an acid-etch restoration, is possible with reasonable co-operation.
Crown root fracture
The pulp is usually exposed and any restorative treatment is very difficult. The tooth is best extracted.
Root fracture
A root fracture without displacement and with only a small amount of mobility should be treated initially by keeping the tooth under observation. If the coronal fragment becomes non-vital and symptomatic, it should be removed. The apical portion usually remains vital and undergoes normal resorption. Similarly, with marked displacement and mobility, only the coronal portion should be removed.
Concussion, subluxation and luxation injuries
Associated soft tissue damage should be cleaned by the parent twice daily with 0.2% chlorhexidine using cotton buds or gauze swabs until healing is completed.
Concussion
Concussion is often not brought to a dentist until a tooth discolours.
Subluxation
If the tooth has slight mobility, a soft diet for 1–2 weeks is advised, with the traumatised area kept as clean as possible. Marked mobility requires extraction.
Extrusive luxation
Marked mobility requires extraction.
Lateral luxation
If the crown is displaced palatally, the apex moves buccally and hence away from the permanent tooth germ. If the occlusion is not gagged, conservative treatment to await some spontaneous realignment is possible. If the crown is displaced buccally, the apex will be displaced towards the permanent tooth bud and extraction is indicated in order to minimise further damage to the permanent successor.
Intrusive luxation
This is the most common type of injury. The aim of investigation is to establish the direction of displacement through radiographical examination. If the root is displaced palatally towards the permanent successor, then the primary tooth should be extracted to minimise the possible damage to the developing permanent successor. If the root is displaced buccally, then periodic review to monitor spontaneous re-eruption should be allowed. Review should be weekly for a month, then monthly for a maximum of 6 months. Most re-eruption occurs between 1 and 6 months. If this does not occur, then ankylosis is likely and extraction is necessary to prevent ectopic eruption of the permanent successor.
Exarticulation (avulsion)
Replantation of avulsed primary incisors is not recommended because of the risk of damage to the permanent tooth germs. Space maintenance is not necessary following the loss of a primary incisor as only minor drifting of adjacent teeth occurs. The eruption of the permanent successor may be delayed for about 1 year as a result of abnormal thickening of connective tissue overlying the tooth germ.
Sequelae of injuries to the primary dentition
Pulpal necrosis
Necrosis is the most common complication of primary trauma. Evaluation is based upon colour and radiography. Teeth of a normal colour rarely develop periapical inflammation; conversely, mildly discoloured teeth may be vital. A mild pink colour occurring soon after trauma may represent intrapulpal bleeding with a pulp that is still vital. This colour may recede; if it persists, then necrosis should be suspected. Radiographic examination should be 3-monthly to check for periapical inflammation. Failure of the pulp cavity to reduce in size is an indicator of pulpal death. Teeth should be extracted whenever there is evidence of periapical inflammation, to prevent possible damage to the permanent successor.
Pulpal obliteration
Obliteration of the pulp chambers and canals is a common reaction to trauma. Clinically, the tooth becomes yellow/opaque. Normal exfoliation is usual, but occasionally periapical inflammation may intervene and, therefore, annual radiography is advisable.
Root resorption
External inflammatory resorption is usually seen after intrusive injuries and internal resorption with subluxation and other luxation injuries. Extraction is advised for all types of root resorption.
Injuries to developing permanent teeth
Injuries to the permanent successor tooth can be expected in 12–69% of primary tooth trauma and 19–68% of jaw fractures. Intrusive luxation causes most disturbances; exarticulation (avulsion) of a primary incisor will also cause damage if the apex moves towards the permanent tooth bud before the avulsion. Most damage to the permanent tooth bud occurs under 3 years of age, during its developmental stage. However, the type and severity of disturbance are closely related to the age at the time of injury. Changes in the morphology and mineralisation of the crown of the permanent incisor are most common but later injuries can cause radicular anomalies. Injuries to developing teeth can be classified as:
• white or yellow–brown discoloration of enamel: injury at 2–7 years
• white or yellow–brown discoloration of enamel with circular enamel hypoplasia: injury at 2–7 years
• crown dilaceration: injury at about 2 years
• odontoma-like malformation: injury at <1–3 years
• root duplication: injury at 2–5 years
• vestibular or lateral root angulation and dilaceration: injury at 2–5 years
• partial or complete arrest of root formation: injury at 5–7 years
Most enamel hypoplasia can be treated with a combination of microabrasion or veneers. Most dilacerations and eruption abnormalities require surgical exposure and orthodontic alignment.
Permanent dentition
The aims and principles of treatment are considered as emergency, intermediate and permanent actions.
1. Emergency:
• retain vitality of fractured or displaced tooth
• reduction and immobilisation of displaced teeth
• antiseptic mouthwash, antibiotics and tetanus prophylaxis.
• with or without pulp therapy
• minimally invasive crown restoration.
3. Permanent:
• root filling with or without root extrusion
Trauma cases require painstaking follow-up to disclose any complications and institute the correct treatment. The intervals between examinations depend on the severity of trauma, but the following schedule is a guide: 1, 3 and 6 weeks then at 3, 6 and 12 months with annual checks for 4–5 years. At these times, colour, mobility, percussion and sensitivity are routinely noted while radiographs are examined for periradicular conditions and changes within the pulp cavity.
Injuries to the hard dental tissues and the pulp
Enamel infraction
These are incomplete fractures and without proper illumination are easily overlooked. Periodic recalls are necessary to review pulpal status.
Enamel fracture
Treatment is usually limited to smoothing any rough edges and splinting if there is mobility. Periodic review is necessary.
Enamel–dentine fracture
Immediate treatment is necessary because of the involvement of dentine. The pulp requires protection against thermal irritation and from bacteria via the dentinal tubules. Restoration of crown morphology also stabilises the position of the tooth in the arch. Emergency protection of the exposed dentine can be achieved by:
These will serve as temporary retainers until further eruption occurs.
Intermediate restoration of most enamel–dentine fractures can be achieved by:
If the fracture line through dentine is not very close to the pulp, the fragment may be reattached immediately. If, however, it runs close to the pulp, it is advisable to place a suitably protected calcium hydroxide dressing over the exposed dentine for at least 1 month while storing the fragment in saline, which should be renewed weekly (Box 8.1).
Complicated crown fracture
The major concern after pulpal exposures in immature teeth is the preservation of pulpal vitality in order to allow continued root growth. The injured pulp must be sealed from bacteria so that it is not infected during the period of repair. Partial pulpotomy or pulpotomy is often the treatment of choice.
Uncomplicated crown root fracture
After removal of the fractured piece of tooth, these vertical fractures are commonly a few millimetres incisal to the gingival margin on the labial surface but down to the cementoenamel junction palatally. Prior to placement of a restoration, the fracture margin has to be brought supragingival either by gingivoplasty or extrusion (orthodontically or surgically) of the root portion.
Complicated crown root fracture
As above, with the addition of endodontic requirements. If extrusion is planned, then the final root length must be no shorter than the final crown length, otherwise the result will be unstable. Root extrusion can be successful in a motivated patient and leads to a stable periodontal condition.
Root fracture
Root fractures occur most frequently in the middle or the apical third of the root. The coronal fragment may be extruded or luxated. Luxation is usually in a lingual or palatal direction.
If displacement has occurred, the coronal fragment should be repositioned as soon as possible by gentle digital manipulation and the position checked radiographically. Mobile root fractures need to be splinted to encourage repair of the fracture. Apical third fractures, in the absence of concomitant periodontal ligament injury, are often firm and do not require splinting. They do need to be regularly reviewed to check pulpal status and to be treated endodontically if necessary.
Apical and middle third fractures must be splinted, as repair of the fracture is important to the long-term stability and prognosis of the tooth. A functional splint with one abutment tooth on either side of the fractured tooth should remain in place for 4 weeks. If the fracture is in the coronal third of the root, splinting should be for at least 4 months. The splint should allow colour observations and sensitivity testing and access to the root canal if endodontic treatment is required. The splint design and placement techniques are discussed below. In about 80% of all root-fractured teeth, the pulp remains viable and repair occurs in the fracture area. Three main categories of repair are recognised:
1. Repair with calcified tissue: invisible or hardly discernible fracture line.
3. Repair with bone and connective tissue: a bony bridge separates the two fragments.
In addition to these changes in the fracture area, pulp canal obliteration is commonly seen. Fractures in the cervical third of the root will repair as well as those in the middle or apical thirds as long as no communication exists between the fracture line and the gingival crevice. If such a communication exists, splinting is not recommended and a decision must be made to extract the coronal fragment and retain the remaining root, to extract the two fragments or to splint the root fracture internally. The latter can only be regarded as a temporary solution.
If the root is retained, the remaining radicular pulp should be removed and the canal temporarily dressed prior to obturating with gutta-percha. Three options are now available for the root-treated radicular portion:
Pulpal necrosis occurs in about 20% of root fractures and is the main obstacle to adequate repair. Most instances of necrosis are diagnosed within 3 months of a root fracture. A persistent negative response to electric stimulation is usually confirmed on radiography by radiolucencies adjacent to the fracture line.
Splinting
Trauma may loosen a tooth either by damaging the periodontal ligament or by fracturing the root. Splinting immobilises the tooth in the correct anatomical position so that further trauma is prevented and healing can occur. Different injuries require different splinting regimens.
Periodontal ligament injuries
Approximately 60% of periodontal ligament healing has occurred after 10 days and it is complete within a month. The splinting period should be as short as possible and the splint should allow some functional movement to prevent replacement root resorption (ankylosis). As a general rule, exarticulation (avulsion) injuries require 2 weeks, luxation injuries 4 weeks.
Apical and middle third root fractures
These require 3–4 weeks of functional splinting to encourage a repair. A connective tissue repair may be satisfactory, but if mobility persists the fracture site becomes filled with granulation tissue and the tooth remains mobile.
Dento-alveolar fractures
These require 4 weeks of rigid splinting.
Coronal third root fractures
These require 4 or more months of functional splinting to repair.
Splint construction
The composite resin/acrylic and wire splint uses either a composite resin or a temporary crown material (Box 8.2). The composite resin is easier to place but the acrylic resin is easier to remove. Although acrylic resin does not have the bond strength to enamel of the composite resin, it is suitable for all types of splinting apart from root fractures. Generally, functional splints should have one abutment tooth each side of the injured tooth and rigid splints two abutment teeth each side.
Other types of splint include orthodontic brackets and wire, interdental wiring, foil/cement splint (temporary) and laboratory splints (acrylic or thermoplastic).
Injuries to the periodontal tissues
Figures for pulp survival 5 years after periodontal ligament injuries are shown in Table 8.2.
Table 8.2
Pulpal survival at 5 years after injuries involving the periodontal ligament
| Injury | Open apex (%) | Closed apex (%) |
| Concussion | 100 | 96 |
| Subluxation | 100 | 85 |
| Extrusive luxation | 95 | 45 |
| Lateral luxation | 95 | 25 |
| Intrusive luxation | 40 | 0 |
| Replantation | 30 | 0 |
Concussion
The impact force causes oedema and haemorrhage in the periodontal ligament and the tooth is tender to percussion (TTP). There is no rupture of periodontal ligament fibres and the tooth is firm in the socket.
Subluxation
In addition to the above, in subluxation there is rupture of some periodontal ligament fibres and the tooth is mobile in the socket, although not displaced. The treatment for both these injuries is:
There is little risk of pulp necrosis or resorption.
Extrusive luxation
In extrusive luxation, there is rupture of the periodontal ligament and pulp. These injuries should have a functional splint for 2 weeks.
Lateral luxation
Lateral luxation involves rupture of periodontal ligament and pulp and compression injury of the alveolar plate. The treatment for extrusive and lateral luxation is:
• local anaesthesia (buccal and palatal)
• atraumatic repositioning of tooth with gentle firm digital pressure
• antibiotics: age-related dose of amoxicillin or alternative for 5 days
The decision to progress to endodontic treatment depends on subsequent regular clinical and radiographic examination.
With more significant damage to the periodontal ligament, there is an increased risk of root resorption (up to 35% of injuries).
Orthodontic appliances should be used to reduce firm older injuries, as digital pressure could further damage the periodontal ligament.
Intrusive luxation
Intrusive luxation injuries are the result of an axial, apical impact. There is extensive damage to the periodontal ligament and alveolar plate(s). Two distinct categories exist: the open and closed apex. At the outset, both categories should receive antibiotics, chlorhexidine mouthwash and a soft diet as previously described. The risk of pulpal necrosis in these injuries is high, especially with a closed apex. The incidence of resorption and ankylosis sequelae is also high.
Open apex
There are two treatment courses for open apex intrusive luxation:
Non-setting calcium hydroxide in the root canal does not preclude orthodontic movement. Once apexification has occurred and orthodontic movement has ceased, obturate with gutta-percha.
Closed apex
The treatment of a closed apex intrusive luxation is:
• elective orthodontic/surgical extrusion immediately
• functional splint for 2 weeks after surgical extrusion
• elective pulp extirpation at 10 days
• maintenance of non-setting calcium hydroxide in the root canal during orthodontic movement
If endodontic treatment is commenced within 2 weeks of an injury to the periodontal ligament, the initial intracanal dressing should be with a polyantibiotic or antibiotic/steroid (Ledermix) paste.
Avulsion and replantation
Replantation of a lost tooth should nearly always be attempted even though it may offer only a temporary solution because of the frequent occurrence of external inflammatory resorption. Even when resorption occurs, the tooth may be retained for years, acting as a natural space maintainer and preserving the height and width of the alveolus to facilitate later implant placement.
Successful healing after replantation can only occur if there is minimal damage to the pulp and the periodontal ligament. The type of extra-alveolar storage medium and the extra-alveolar time (i.e. the time the tooth has been out of the mouth) are critical factors. The suggested protocol for replantation can be divided into advice on the telephone, immediate treatment in surgery and review (Box 8.3). The immature tooth with an extra-alveolar time of less than 45 minutes may undergo pulp revascularisation. However, these teeth require regular clinical and radiographic review because once external inflammatory resorption occurs, it progresses rapidly.
Replantation of teeth with a dry storage time of greater than 1 hour
Mature teeth with a dry storage time of greater than 1 hour will have a non-vital periodontal ligament. The periodontal ligament and the pulp should be removed at the chair side and the tooth placed for 20 minutes in 2.4% sodium fluoride solution at pH 5.5. The root canal is then obturated with gutta-percha and the tooth replanted and splinted for 4 weeks. The aim of this treatment is to produce ankylosis, allowing the tooth to be maintained as a natural space maintainer, perhaps for a limited period only. The sodium fluoride is believed to slow down resorptive processes.
Very immature teeth with an extra-alveolar dry time of greater than 1 hour should not be replanted.
Injuries to supporting alveolar bone
The extent and position of the alveolar fracture should be verified clinically and radiographically. If there is displacement of the teeth to the extent that their apices have risen up and are now positioned over the labial or lingual/palatal alveolar plates (‘apical lock’), they will first require extruding to free the apices prior to repositioning.
The segment of alveolus with teeth requires only 4 weeks of splintage (composite-wire type) with two abutment teeth either side of the fracture, together with antibiotics, chlorhexidine, soft diet and tetanus prophylaxis if necessary.
Pulp survival is more likely if repositioning occurs within 1 hour of the injury. Root resorption is rare.
Child physical abuse (non-accidental injury)
A child is considered to be abused if he or she is treated in a way that is unacceptable in a given culture at a given time. NAI is now recognised as an international issue and has been reported in many countries. Each week at least four children in the UK and 80 children in the USA will die as a result of abuse or neglect. At least one child per 1000 in Britain suffers severe physical abuse, for example fractures, brain haemorrhage, severe internal injuries or mutilation. In the USA, more than 95% of serious intracranial injuries during the first year of life are the result of abuse. Although some reports will prove to be unfounded, the common experience is that proved cases of child abuse are four- to five-fold more common than they were in the 1980s.
NAI is not a full diagnosis – it is merely a symptom of disordered parenting. The aim of intervention is to diagnose and cure the disordered parenting. Simply to aim at preventing death is lowly ambition. It has been estimated in the USA that 35–50% of severely abused children will receive serious reinjury and 50% will die if they are returned to their home environment without intervention. In some cases, the occurrence of physical abuse may provide an opportunity for intervention. If this opportunity is missed, there may be no further opportunity for many years.
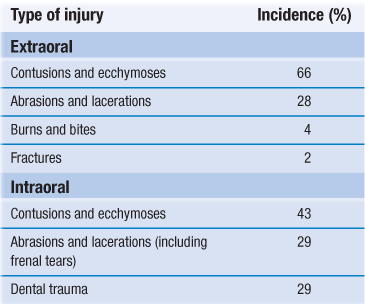
Approximately 65% of cases diagnosed as NAI have extra- and intraoral facial trauma; consequently, the dental practitioner may be the first professional to see or suspect abuse. Injuries may take the form of contusions and ecchymoses, abrasions and lacerations, burns, bites and dental trauma. The incidences of common orofacial injuries are shown in Table 8.3.
The following points should be considered whenever doubts and suspicions are aroused.
1. Could the injury have been caused accidentally and, if so, how?
2. Does the explanation for the injury fit the age and the clinical findings?
4. If there has been any delay seeking advice, are there good reasons for this?
5. Does the story of the accident vary?
6. The nature of the relationship between parent and child.
7. The child’s reaction to other people.
8. The child’s reaction to any medical/dental examinations.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses