8
Orthodontically driven corticotomy: Tissue engineering to enhance adult and multidisciplinary treatment
Federico Brugnami1 and Alfonso Caiazzo2,3
1 Private Practice Limited to Periodontics, Oral Implants and Adult Orthodontics, Piazza dei Prati degli Strozzi 21, Rome, Italy
2 Department of Oral and Maxillofacial Surgery, Boston University Henry M. Goldman School of Dental Medicine, Boston, MA, USA
3 Centro Odontoiatrico Salernitano, Via Bottiglieri 13 Salerno, Italy
Introduction
In Chapters 6 and 7 we described how the principles of tissue engineering applied to orthodontics may enhance treatment. In other words, it is the surgical insult that facilitates, improves, and hastens the tooth movement. In this chapter we would like to show how corticotomy-assisted orthodontics may enhance inter- or multidisciplinary treatment. Multidisciplinary treatment requires excellent communication and coordination between different specialists. Although this can be difficult to achieve at first, interdisciplinary collaboration may result in a very efficient execution that patients appreciate and benefit from. When appropriately coordinated, the goal of each different specialist is to facilitate the work of the other team members. For example, orthodontists can be of considerable assistance in periodontal and prosthetic treatment. Dental alignment of the arches can, in fact, facilitate the periodontist’s and prosthodontist’s objectives. This is done, for example, by aligning the natural dentition and making possible a path of insertion of a prosthesis, or establishing a physiologic alveolar crestal topography to facilitate periodontal surgery. Orthodontic tooth movement can then be a substantial benefit for the patient (Mihram and Murphy, 2008).
Many adults seeking routine restorative dentistry have, in fact, problems with tooth malposition that compromises either the final restorative outcome or the ability to clean the natural dentition. A particular emphasis on adult treatment will also be undertaken here not only because adult treatment is facing periodontal and/or restorative challenges that the youth treatment may not be facing, but also because adult orthodontics has recently become very popular, especially in the western part of the world. Many adults realize that correction of dental malocclusions in adulthood is certainly possible and has the benefit of preserving long-term dental and periodontal health besides causing significant esthetic enhancement. This rise in popularity has further been hastened by significant improvements in dental and surgical techniques and biotechnology. Orthodontic appliances have become smaller, less noticeable, and are easier to maintain during therapy. Invisible and/or lingual appliances are in high demand. In addition, dental implants have become a major part of the comprehensive treatment plans for adults with missing teeth.
The length of treatment still remains one of the major deterrents against universal acceptance of orthodontic treatment by the adult population. Corticotomy-assisted adjunctive orthodontics is the essence of multidisciplinary treatment: a periodontal procedure that enhances orthodontics in enhancing periodontal and prosthetic treatment.
Corticotomy in multidisciplinary treatment
As previously seen, the concept of surgically accelerated orthodontics (SAO) can significantly reduce the total treatment time of orthodontic therapy, and when associated with bone graft, an expansion of the basal bone may be achieved. This may be translated clinically into less need for extractions, a better protection of periodontal health, and become a new powerful tool in adult complex cases needing an inter- or multidisciplinary approach. The major obstacle to a widespread application of corticotomy is the reluctance of the patients toward surgery. In most adult patients, which can be classified as mutilated dentition cases, many problems may be associated with malocclusion, such as periodontal disease, missing dentition, resorbed edentoulous alveolar ridge, pathologic migration of the remaining teeth in the edentoulous space, complicating the path to an acceptable esthetical and functional rehabilitation of the mouth. Therefore, other oral surgical procedures, such as wisdom teeth extractions, bone augmentation, and/or implant placement may be already planned. Corticotomy may be combined and planned with these procedures in order to minimize the patient’s surgical exposure. This approach may look somewhat cumbersome and time consuming at first, but has the potential to achieve optimal results that may be beneficial for many patients. It requires efficient communication between multiple clinicians who have expertise in varying fields. When appropriately coordinated and executed, the input of each specialist can help facilitate the work of other team members.
Orthodontics for prosthetics
Alignment of the alveolar arches by an orthodontist can, in certain select cases, be aimed to develop a path of insertion of a prosthesis or can be done to establish physiologic gingival margin topography to correct a gummy smile or asymmetry prior to esthetic prosthetic rehabilitation. Similarly, in patients where dental migration precludes prosthetic rehabilitation, orthodontic therapy has the potential to selectively move teeth into predesigned positions to allow for surgical implant placement and dental restoration. Many adult malocclusion cases are associated with tooth loss, bone resorption, and consequent need for implants and/or periodontal treatment and bone augmentation procedures. In such patients, reshaping and augmentation of bone by an endosseous implant placement by a surgical specialist can theoretically be used to obtain adequate anchorage and increase precision and predictability of tooth movement by the orthodontist.
Periodontics and orthodontics synergy: The two dental specialties that need a healthy periodontium
As already mentioned and demonstrated in different chapters, considering corticotomy just as a method to accelerate orthodontic movement would be limitative. One of the most interesting effects is that this technique may help (as confirmed here by the clinical and histologic findings) in expanding the basal bone. This will clinically translate into at least two main positive effects: (1) more space to accommodate crowded teeth and then less extraction of healthy premolars in growing patients; (2) a thicker, more robust periodontium, which may help minimize the risk of gingival recession during or after orthodontic movement. The concept can be stretched to the point that, according to Williams and Murphy (2008), “the alveolar ‘envelope’ or limits of alveolar housing may be more malleable than previously believed and can be virtually defined by the position of the roots.” Please refer to Chapter 6 for a more detailed discussion on periodontal considerations during or after orthodontic treatment.
Adult orthodontics
Adult orthodontics is only expected to increase in prevalence. It is not uncommon for many adults to have a periodontium without optimal bone width and volume. The risk of creating root dehiscence in patients with such a thin periodontium is very high, even with slow, traditional orthodontic movement and light forces. Root fenestrations or dehiscences can be present even without the clinical manifestation of gingival recession. In these cases, a careful treatment planning using a multidisciplinary approach is critical for a successful recipe. Accelerated orthodontic movement techniques can be successfully used to hasten dental movement, treat and prevent periodontal problems, and to regenerate ridge defects, thereby allowing delayed implant placement. In this chapter we would like to present a variety of different combinations of corticotomy in adult patients to facilitate the multidisciplinary treatment.
Case presentation
Case 1. Mutilated dentition 1: Orthodontics and prosthodontics connection, enhancing the periodontal outcome
A 42-year-old white female presented with a class II, division I malocclusion, deep bite, and severe crowding in the lower jaw (Figure 8.1). She additionally complained of her smile, crowding of lower teeth, and wanting replacement of her missing lower teeth (Figure 8.2). Clinical examination revealed an edentulous and severely atrophic mandibular alveolar ridge (Figure 8.3) and missing teeth nos. 24 and 25. The patient also had ceramic dental restorations on teeth nos. 5 and 6 and an implant-supported ceramic restoration on tooth no. 11. Radiographically, there were no signs of periodontal or periapical disease. Clinically, periodontal heath was good, with only mild buccal gingival recession on teeth nos. 21, 23, and 28 (class I Miller classification).



Figure 8.1 A 42-year-old white female presented with a class II, division I malocclusion, deep bite, severe crowding in the lower jaw, severely atrophic mandibular alveolar ridge and missing teeth nos. 24 and 25.

Figure 8.2 Case 1: Detail of the anterior sextant, showing mild crowding and gingival misalignment.
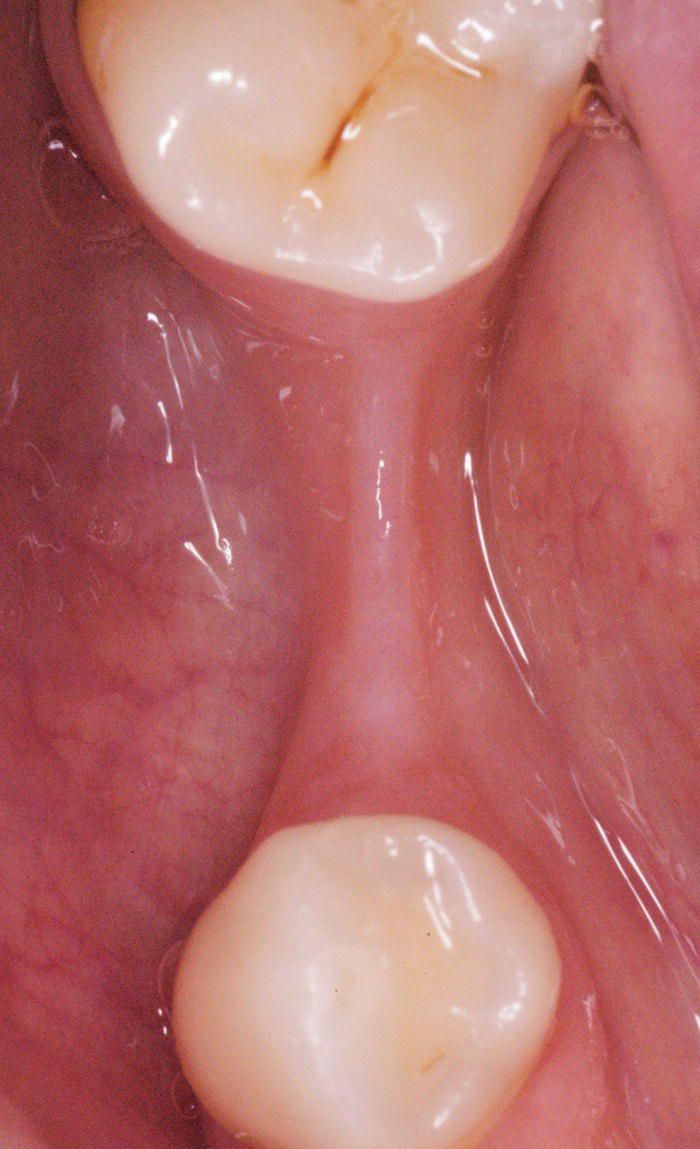
Figure 8.3 Occlusal view of edentulous ridge before augmentation.
The objective of the orthodontic therapy was to resolve lower crowding, correct deep bite, and level gingival margin of the anterior upper sextant to facilitate prosthodontist’s work in achieving an optimal esthetic. No attempt to correct the skeletal and dental class II was planned.
The comprehensive dental treatment plan included augmentation of edentulous ridge, fixed restoration on implant for missing lower right premolar, crowns on teeth nos. 6, 7, and 8 for esthetics.
She was given the two following options:
- Conventional treatment, whereby the orthodontic treatment would be performed, followed by the augmentation procedure, and then the implant placement once the orthodontic movement had been completed later as a secondary procedure.
- Corticotomy-Assisted Orthodontics.
The second treatment option was accepted, especially because it was possible to perform the ridge augmentation, including the harvesting of autologous bone, and the corticotomy in one combined surgical procedure.
Technical procedure
The patient was bracketed 2 weeks before surgery (Figure 7.8). She opted for ceramic brackets (Leone, Florence, Italy) in the upper arch and metal ones for the lower for esthetic reasons. Nickel–titanium 0.016″ wire was used in the upper arch and 0.012″ archwire was used in the lower arch. The periodontal procedure to accelerate the orthodontic movement was planned at the lower incisor level together with the ridge augmentation in the contiguous edentulous area and performed 2 weeks after bracketing. The symphysis area was also targeted as a source of autologous bone for the bone augmentation procedure. The patient was premedicated orally with 2 g of amoxicillin 1 h before surgery. A full-thickness muco-periosteal flap was elevated under local anesthesia using a sulcular incision extending from the distal line angle of the second lower right molar to the distal line angle of the first lower left premolar. Care was taken to preserve the papillae in the anterior area (lower incisors level). Autologous graft was then harvested from the same area using a manual bone-scraping instrument and placed over the deficient ridge. This area was then further augmented with xenogeneic bone (Endobone, Biomet Palm Beach Gardens, FL, USA) and covered with a resorbable membrane (Osseoguard, Biomet Palm Beach Gardens, FL, USA). The xenogeneic bone was also placed over the buccal plate in the anterior sextant, with particular care to ensure coverage of the areas with dehiscence of the roots. In the region of tooth no. 26 a resorbable membrane was used to cover the osseous defect following the principles of conventional guided tissue regeneration (GTR) technique, while the recession at tooth no 28 no membrane or bone graft were used, the site was considered to be the control site (Figure 7.8c and d). The flap was then coronally repositioned and sutured in an interrupted fashion to obtain primary closure. The patient was placed on chlorhexidine 0.2% rinses twice a day, oral amoxicillin for 1 week, and nonsteroidal anti-inflammatory drugs (naproxen) for pain twice a day if needed. The orthodontic wires were replaced 1 week after surgery. The patient had no significant pain or discomfort during the first postoperative week. On postoperative day 7, a 0.014″ nickel–titanium archwire was placed. The patient was put on a soft diet for the following 10 days and was instructed to continue rinsing with the antimicrobial agent. On post-operative day 17 the archwire was changed to a 0.016″ and the patient advanced to a regular diet. The lower anterior dental alignment was almost completed 3 weeks post-operatively, and 6 weeks after surgery the anterior crowding was completely resolved (Figure 7.8). Soft tissue architecture and the periodontium continued to remain healthy, and the area of teeth nos. 29 and 30 retained the horizontal augmentation. Six months after surgery, an endosseous implant was placed into the augmented area. At the re-entry time, an adequately regenerated area was evident, with enough bony width and height to place an implant (Figure 8.4).
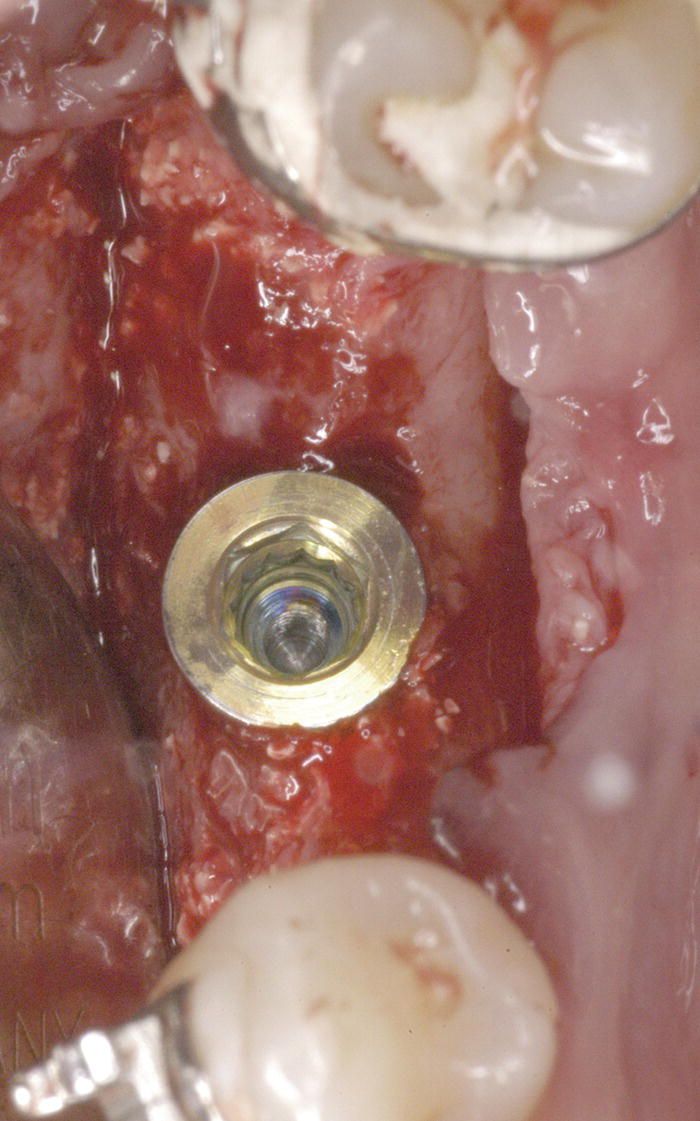
Figure 8.4 At the re-entry time, an adequately regenerated area was evident, with enough bony width and height to place an implant.
A bone core biopsy as a part of the implant placement as described by Brugnami et al. (1996) was performed (Figure 8.5). The specimen was fixed in formalin and decalcified in Mielodec Bio-Optica for 90 min. After being embedded in paraffin and cut to a 3 μm thickness, the sections were stained with hematoxylin and eosin, and then examined using light microscopy. The Image J software was used to calculate the percentage of mineralized tissue at a 4× magnification. The histology showed residual particles of the graft that were completely surrounded by a newly regenerated mixture of woven and lamellar bone. Histomorphometry results indicated that 62% of the area is occupied by bone. Despite the movement outside the original bony envelope that eventually takes place in the decrowding treatment because of the very nature of the straight-wire technique, a regeneration of the bony dehiscence overlying tooth no. 26 was evident in the anterior area while the control (tooth no. 28) remained unchanged (Figure 7.8e), confirming the importance of combination of the corticotomy with a regenerative procedure (bone graft alone or with guided bone regeneration (GBR)/GTR). The buccal plate on tooth no. 27 also appeared augmented in thickness. In the area of tooth no. 27, where the bone graft was not originally covered with the membrane, a fragment of tissue was harvested with a blade (Figure 7.8f) and processed as described previously. The result showed a prominent bone marrow portion with some rare fibrous connective tissue and mature bone for 35% of the core area (Figure 7.8 g). Although we should refrain from making definitive conclusions based on analyzing one histologic sample, we can make some preliminary hypothesis:
- Particulate graft alone may be enough to regenerate some bone (in the inner side, facing the tooth), while some of the original graft becomes encapsulated in fibrous connective tissue (in the outer side, facing the soft tissues).
- Approximately two-thirds of the graft facing the tooth may turn into new bone.
- Some of the the graft facing the flap may be encapsulated by fibrous connective tissue. This part will not contribute to the regeneration of periodontal attachments and may act as a (modified) connective tissue graft. In other words, it does not regenerate the periodontal attachment, but may thicken the soft tissue, changing the periodontal biotype. It may be speculated that the slow resorption particles of the graft may act as a filler and contribute to a long-term stability of the soft tissues (Figure 8.6).
- The difference in mature bone percentage between the implant area and the buccal plate of no. 27 (62% versus 35%) may be explained by the difference in harvesting (trephine for a depth to 6–7 mm versus blade for a superficial layer only), but also by the presence/absence of the membrane. This is an interesting topic that may require further investigation and clarification. The original PAOO technique, in fact, does not include the use of a membrane and the re-entry at 10 years shown by the Wilcko brothers definitely has proven their way of grafting to be very effective (Wilcko MW et al., 2001; Wilcko MT et al., 2008).
The main differences between the PAOO and our single-flap corticotomy (SFC) is the quantity of bone graft used: 0.5–1 cm3 per tooth and 0.5 cm3 for quadrant respectively. To overcome the difference in quantity, we suggest the use of a membrane.
- In SFC the use of membrane may be required in cases where the surgery is attempting to solve skeletal transverse or sagittal discrepancy (i.e., palatal expansion and/or minor class II or class III). It may be less crucial in protecting the periodontium in decrowding cases.
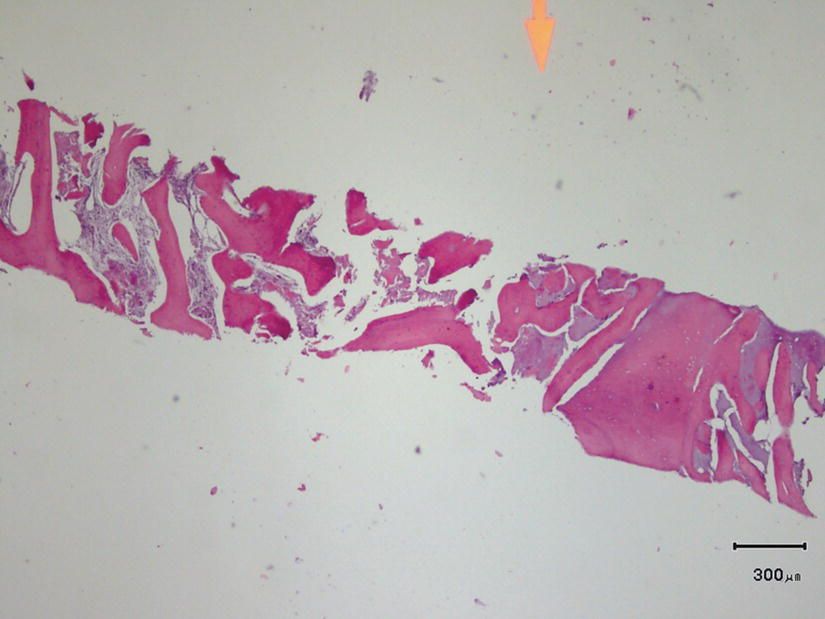
Figure 8.5 The histology showed residual particles of the graft that were completely surrounded by a newly regenerated mixture of woven and lamellar bone. Histomorphometry results indicated 62% of the area occupied by bone.
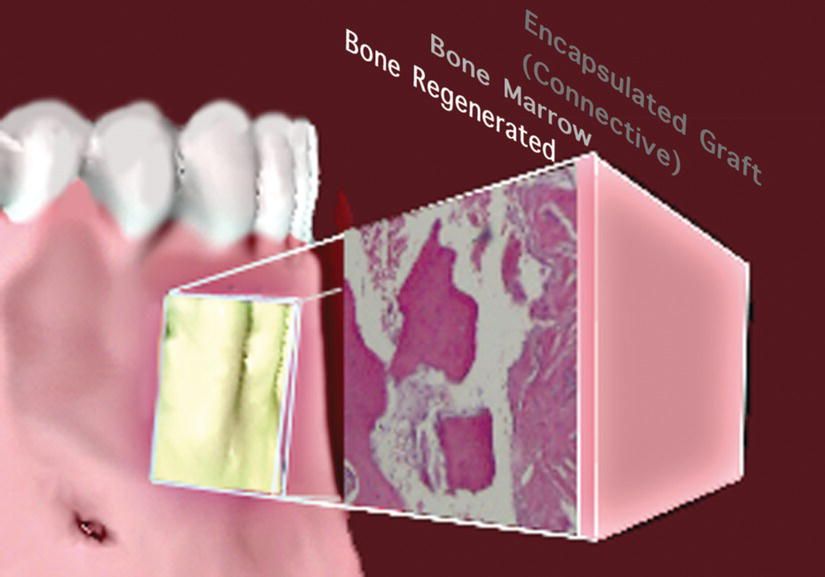
Figure 8.6 According to the histologic sample harvested in the area, the inner portion of the graft may turn into newly regenerated bone, with some portion of bone marrow, while the outer layer most likely becomes encapsulated by fibrous connective tissue. This is not necessarily a negative result, since it may be speculated that the slow resorption particles of the graft may act as a filler and contribute to a long-term stability of the soft tissues.
Six months after implant placement a provisional crown was delivered. The case was de-bracketed when de-crowding, deep bite correction, and proper alignment of the cervical margin of the anterior sextant were achieved (Figures 8.7 and 8.9).

Figure 8.7 End of orthodontic treatment, before definitive prosthetic treatment; note the resolution of deep bite and crowding and alignment of cervical margins of upper anterior sextant.

Figure 8.8 Delivery of final restorations. Note excellent final esthetic as a result of combination of optimal prosthetic work and gingival health and harmony (prosthetic work by Dr Graziano Brugnami, private practice, Rome, Italy; technical work by odt. Mauro Merletti, Rome, Italy).


Figure 8.9 Pre- and post-operative detail of overbite correction, before definitive crown delivery on teeth nos. 7, 8, and 9; note the difference in thickness of the periodontal tissues of the lower anterior sextant.
Final functional and esthetic adjustments were accomplished with the delivery of the final prosthetic (Figure 8.8).
Case 2. The summer break case: an alternative to veneers to correct esthetics in the anterior area
The patient, a healthy 21-year-old woman who was dissatisfied with her smile, presented with a slight crowding of the anterior superior teeth and overlapping central incisors (Figure 8.10).

Figure 8.10 Case 2: Patient presented a very mild crowding and central incisors overlapping in the upper anterior sextant.
This college student on summer break wanted to resolve this rather mild esthetic problem before returning to college in the fall. The medical/dental history and intraoral examination found no medical contraindication to treatment. The periodontium was healthy, with no recession or bone resorption, as confirmed by interproximal radiography.
Various treatment modalities were proposed to the patient, including porcelain veneers and conventional orthodontic movement. Also, in an effort to accelerate the treatment, a lingual approach was proposed, combined with the minimally invasive P/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


