CHAPTER 8
Orofacial pain (including sensory and motor disturbance)
• Temporomandibular joint dysfunction
• Facial nerve palsy (Bell’s palsy)
• Trigeminal nerve paresthesia or anesthesia
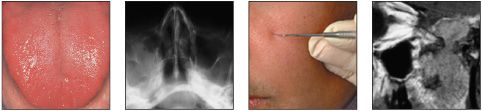
General approach
• Orofacial pain is often the reason why a patient attends a dental clinic. In most cases, clinical examination will reveal an obvious dental cause of the symptoms, such as a carious tooth, lost restoration, or acute dentoalveolar abscess. In such circumstances, diagnosis is usually relatively straightforward and appropriate treatment can be provided. (Pain of dental origin is not covered in this book.)
• Patients may also present with pain for which there is no apparent dental cause, either clinically or radiographically. In this case a diagnosis can only be made on the basis of a detailed assessment of the character of the pain, including factors such as duration, site, severity, initiating factors, and relieving factors. Clinical examination and questioning will reveal other typical findings associated with each condition.
Orofacial pain can be initially divided into those conditions in which symptoms are episodic and those in which the pain is constant (Tables 8–10). This chapter also covers neurological disorders that may present as either altered sensation or loss of motor function.
Table 8 Patterns of pain and differential diagnosis
Episodic pain
• Trigeminal neuralgia
• Glossopharyngeal neuralgia
• Postherpetic neuralgia
• Giant cell arteritis
Constant pain
• Burning mouth syndrome
• Atypical facial pain
• Atypical odontalgia
• Postherpetic neuralgia
• Temporomandibular joint dysfunction
Loss of function or sensation
• Facial nerve palsy (Bell’s palsy)
• Trigeminal nerve paresthesia
Table 9 Episodic pain symptoms
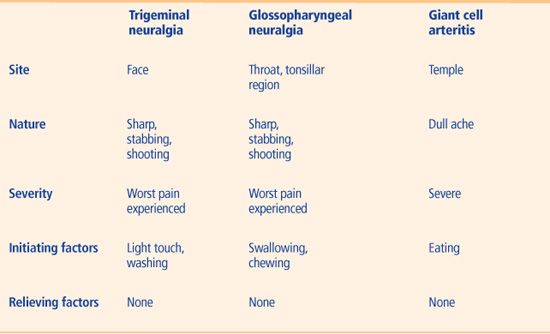
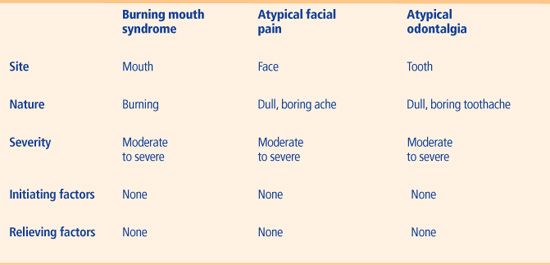
Table 10 Constant pain symptoms
Trigeminal neuralgia
ETIOLOGY AND PATHOGENESIS
A number of theories have been proposed as to the etiology of trigeminal neuralgia. Histopathological examination of autopsy material from patients with a history of trigeminal neuralgia has led to a suggestion that pain occurs due to the presence of areas of demyelination along the distribution of the trigeminal nerve, particularly where the nerve exits the base of the skull. Alternatively, other studies using MRI have implicated the involvement of aberrant intracranial blood vessels in the cerebellopontine region. Rarely, an accompanying organic disease, such as a neoplasm within the nasopharynx, maxillary antrum, middle ear, or base of the skull, or a vascular aneurysm in close relation to the trigeminal nerve, may produce symptoms attributable to trigeminal neuralgia. Trigeminal neuralgia is a relatively common condition in older individuals; however, diagnosis in a patient under the age of 40 years should raise suspicion of the presence of an underlying systemic disease, in particular multiple sclerosis or HIV infection.
CLINICAL FEATURES
The pain of trigeminal neuralgia is characteristic in that it is unilateral and limited to the anatomical pathway of one of the three main branches (mandibular, maxillary, or ophthalmic) of the trigeminal nerve. The pain is of short duration, lasting only a matter of seconds. However, despite being brief, the severity of the symptoms is extreme and many patients report that the pain is the worst that they have ever experienced. The nature of the pain is shooting, stabbing, or ‘electric shock’-like. Sufferers may describe trigger spots on their skin or in their mouth, while others report that smiling, eating, or washing can bring on an attack. In males, such a trigger spot may prevent shaving in a particular area, resulting in an area of facial hair growth (369). Clinical examination will not reveal any abnormality apart from the site of any trigger spots. Indeed, intraoral examination may be complicated or limited due to the patient’s fear that movement or contact with facial tissues may precipitate an attack of pain. The presence of any other neurological signs or symptoms, such as muscle weakness or altered nerve sensation, would indicate the need for a full neurological assessment.
DIAGNOSIS
Diagnosis is based on the clinical history and the nature of the symptoms. CT or MRI should be performed on any patient suspected of having trigeminal neuralgia to rule out organic disease such as a brainstem tumor, although this may not be practical in all clinical settings.
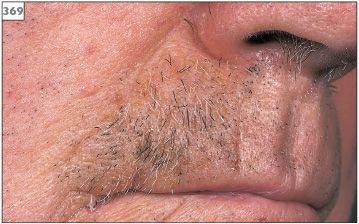
369 Unshaven area due to a trigger spot on the upper lip.
MANAGEMENT
Trigeminal neuralgia can usually be successfully managed pharmacologically using the anticonvulsant drug carbamazepine. Initial treatment should comprise 100 mg carbamazepine, taken every 8 hours. It is likely that this will have to be increased over the subsequent days to achieve full control of the pain. In practice, a dose of 600–800 mg, in divided dosages, is usually required. Carbamazepine may be given at up to levels of 1,600 mg/day. The half-life of carbamazepine varies, depending on the frequency of the dosage prescribed, and therefore the more frequently the drug is administered the shorter the half-life. If a regimen of divided doses fails to control the pain, it is worthwhile trying a single- or two-dose approach. Alternatively, therapy may be changed to a modified release preparation, carbamazepine retard.
The duration of treatment remains speculative but most patients can gradually reduce therapy after 6–12 symptom-free months. Prescribing the drug for short periods of time (1–2 months) will almost certainly result in a recurrence of pain. Carbamazepine therapy has recognized side-effects of suppression of white blood cell production and induction of liver enzymes. In view of these effects, baseline CBC and liver function tests (LFTs) should be taken prior to the start of therapy. These tests should be repeated at approximately 3-monthly intervals while treatment is being given. If a progressive neutropenia is encountered, then the drug should be changed. In the first instance, oxcarbazepine, which may be given at levels of up to 2,400 mg per day with reduced likelihood of inducing neutropenia, may be tried. In addition, carbamazepine may produce other adverse events, in particular nausea, ataxia, and an erythematous, pruritic skin rash. Cases of erythema multiforme have also been reported in association with the use of carbamazepine.
If carbamazepine therapy is found to be ineffective or has to be discontinued because of the side-effects mentioned above, then consideration can be given to the use of phenytoin, clonazepam, sodium valproate, gabapentin, or pregabalin. Should all types of medical therapy fail, then surgical treatment may have to be considered. Peripheral techniques involving alcohol or glycerol nerve blocks are effective in some cases, although symptoms do return after approximately 18 months. Cryotherapy, surgical section, fractional rhizotomy, or thermocoagulation have also been tried, with varying success. Unfortunately, surgical techniques produce permanent facial anesthesia and a risk of dysesthia, which can be troublesome to the patient. Microvascular decompression (MVD) is a neurosurgical procedure involving displacement of aberrant blood vessels from immediate contact with the trigeminal nerve (370). MVD has achieved a high success rate but the use of this technique should be considered on an individual basis due to the significant risks of morbidity or mortality.

370 Scar following microvascular decompression surgery.
Glossopharyngeal neuralgia
ETIOLOGY AND PATHOGENESIS
The etiology of glossophayngeal neuralgia is uncertain. However, since the symptoms of this condition are similar to those of trigeminal neuralgia, similar mechanisms may be involved. In contrast, glossopharyngeal neuralgia is a rare condition and tends to affect a slightly younger age group than trigeminal neuralgia. It is important to remember that cases of glossopharyngeal neuralgia are often found to represent the presence of a neoplasm at the base of the tongue or in the oropharynx.
CLINICAL FEATURES
The pain of glossopharyngeal neuralgia is identical to that of trigeminal neuralgia (above), but in this condition the severe shooting sensation is sited within the tonsil region or oropharynx, possibly with radiation to the ear. The symptoms are usually initiated by swallowing, chewing, or coughing.
DIAGNOSIS
Diagnosis is based on the clinical history and the nature of the symptoms. As with trigeminal neuralgia, the presence of organic disease, in particular pharyngeal carcinoma or salivary gland neoplasm, should be excluded by appropriate examination of the oropharynx supplemented with CT (371) or MRI.
MANAGEMENT
Carbamazepine is usually successful in controlling the pain. Resolution of symptoms following a trial course of carbamazepine in a suspected case can support the diagnosis. Surgical options may be considered in cases that are unresponsive to drug therapy.
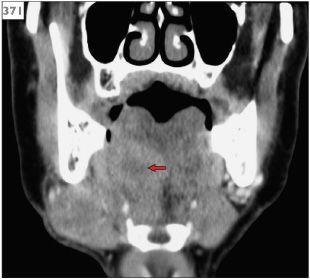
371 CT scan showing squamous cell carcinoma at the base of the tongue (arrow).
Postherpetic neuralgia
ET/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


