CHAPTER 3
Blisters
• Primary herpetic gingivostomatitis
• Recurrent herpes simplex infection
• Hand, foot, and mouth disease
General approach
• Blistering of the oral mucosa may due to trauma, infection, or immune-related disease. Although blistering disorders frequently affect the oral mucosa, it is rare to see intact vesicles or bullae since they rapidly rupture, leaving an area of erosion or ulceration (Chapter 2).
• Blistering conditions are usually painful.
• The diagnosis of blistering disease invariably requires the use of immunofluorescence studies on biopsy material and serum. An important exception is herpetic infections.
Although blistering disease may develop at any age, the conditions may be divided into those occurring in younger individuals and those seen most frequently in adults or the elderly (Table 2).
Table 2 Patterns of blistering and differential diagnosis
Blistering conditions in children or young adults
• Primary herpetic gingivostomatitis
• Recurrent herpes simplex infection
• Chickenpox
• Hand, foot, and mouth disease
• Herpangina
• Epidermolysis bullosa
• Mucocele
Blistering conditions in adulthood or the elderly
• Shingles
• Epidermolysis bullosa (acquisita)
• Angina bullosa hemorrhagica
• Erythema multiforme
• Mucous membrane pemphigoid
• Pemphigus
• Linear IgA disease
• Dermatitis herpetiformis
Primary herpetic gingivostomatitis
ETIOLOGY AND PATHOGENESIS
Primary herpetic gingivostomatitis has been exclusively attributed to infection with HSV type I, although it is now recognized that HSV type II, traditionally associated with genital herpes, may occasionally be involved. This condition is the most frequent viral infection of the mouth. HSV spreads easily through saliva and the source of infection may be an individual who is asymptomatically shedding virus in saliva or suffering a recurrent infection, such as herpes labialis. HSV initially infects epithelial cells of the oral mucosa to produce intraepithelial blisters. Following recovery from primary infection, the virus resides latent in neural and other orofacial tissues. Examination of antibody status has revealed that more than 60% of the population of Europe and North America have evidence of HSV infection by the age of 16 years.
CLINICAL FEATURES
Primary infection often goes unnoticed or is dismissed as an episode of teething during childhood. However, it has been estimated that approximately 5% of individuals who first encounter the virus develop significant symptoms. The blisters of primary herpetic gingivostomatitis rupture rapidly to produce blood-crusted lips (88, 89) and widespread painful oral ulceration (90, 91). In addition, the gingivae are swollen and erythematous (92). The condition is associated with pyrexia, headache, and cervical lymphadenopathy.
DIAGNOSIS
Isolation and culture of HSV using a viral swab is the standard method of diagnosis. Confirmation of HSV infection can also be made serologically by the demonstration of a fourfold rise in antibody titer in acute and convalescent samples. Both these methods may take 10 days to provide a result. Chair-side kits that can detect, using immunofluorescence, the presence of HSV in a lesional smear within minutes are available, but their routine use is limited by cost. Biopsy is rarely necessary but if undertaken will show vesiculation and/or ulceration with multinucleated giant cells representing viral-infected keratinocytes.
MANAGEMENT
Patients, and in the case of children usually their parents, should be reassured about the basis of the condition and advised of the infectious nature of the lesions. Instructions should be given to limit contact with the lips and mouth to reduce the risk of spread of infection to other sites. Supportive symptomatic therapy should include a chlorhexidine mouthwash, analgesic therapy, soft diet, and adequate fluid intake. Use of acyclovir (aciclovir), an antiviral agent with activity against HSV, should be considered in severe cases. The standard regimen is 200 mg acyclovir (aciclovir), either as a dispersible tablet or suspension, five times daily for 5 days. The dosage should be halved in children under the age of 2 years.
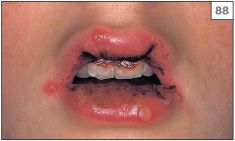
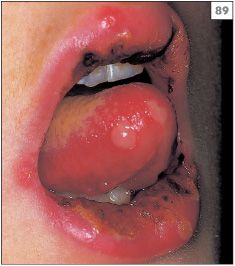

88–90 Vesicles, blood crusting of the lips, and multiple intraoral ulcers characteristic of primary herpes simplex virus infection.

91 Blistering of the upper lip caused by herpes simplex virus.

92 Swelling of the interdental papillae and gingival margins caused by herpes simplex virus.
Recurrent herpes simplex infection
ETIOLOGY AND PATHOGENESIS
Secondary herpes simplex infection is caused by reactivation of latent HSV. Traditionally, it has been thought that HSV migrates from the trigeminal ganglion to the peripheral tissues. While this is possible, it is becoming increasingly apparent that HSV also resides more locally in neural and other tissues. Up to 40% of HSV-positive individuals suffer from recurrent infections. The development of recurrent disease is related to either a breakdown in local immunosurveillance or an alteration in local inflammatory mediators that permits the virus to replicate.
CLINICAL FEATURES
Reactivation of HSV characteristically produces herpes labialis (cold sore, fever, blister). The symptoms of herpes labialis usually begin as a tingling or burning sensation (prodrome) in a localized region of the lips at the vermillion border. However, approximately 25% of episodes of herpes labialis have no prodrome and present initially as a crop of vesicles. Within 48 hours the vesicles rupture to leave an erosion that subsequently crusts over and will eventually heal within 7–10 days (93–96). Factors that predispose to the development of herpes labialis in susceptible individuals include sunlight, trauma, stress, fever, menstruation, and immusuppression.

93 Vesicles of herpes labialis.

94 Vesicle stage of recurrent herpes labialis.

95 Crusting of a healing herpes labialis.

96 Crusting stage of multiple recurrent herpes labialis.
Reactivation of HSV can also produce recurrent intraoral ulceration. Similar to herpes labialis, the patient with an intraoral lesion is usually aware of prodromal tingling. The mucosa of the hard palate is the site most frequently involved (97, 98) but other areas, such as the lower buccal sulcus or gingival margins (99), can also be affected. It can be difficult to determine whether the lesion(s) were precipitated by trauma in these patients or whether they chronically shed HSV in their saliva, which subsequently colonizes traumatized mucosa.
DIAGNOSIS
Taken together with the history, the clinical appearance is usually diagnostic. Confirmation of the presence of HSV can be made by isolation from a swab in tissue culture or the use of immunofluorescence on a smear of a recent lesion.
MANAGEMENT
In many cases no active treatment is indicated, but the patient should be warned about the infectivity of the lesion. The use of topical acyclovir (aciclovir), valacyclovir (valaciclovir) or penciclovir as early as possible can reduce the duration of herpes labialis. A sunscreen applied to the lips can also be effective in reducing the frequency of sunlight-induced recurrences. The use of prophylactic systemic antiviral therapy (acyclovir [aciclovir] 200 mg three times daily, valacyclovir [valaciclovir] 500 mg twice daily, or famciclovir 250 mg twice daily) can be considered in individuals who have frequent and severe episodes of herpes labialis.


97, 98 Multiple ulcers in the hard palate, a frequent site of recurrent herpes simplex virus infection.

99 Ulceration of the gingival margins due to recurrent herpetic infection.
Chickenpox and shingles
ETIOLOGY AND PATHOGENESIS
Primary infection with VZV produces chickenpox in childhood, while reactivation of latent VZV in later life produces herpes zoster (shingles). VZV is highly contagious and transmission is believed to be predominantly through the inspiration of contaminated droplets. During the 2-week incubation period of primary infection, the virus proliferates within macrophages, with subsequent viremia and dissemination to the skin and other organs. VZV progress along the sensory nerves to the nerve ganglia, where it resides in a latent form.
Reactivation of latent VZV characteristically follows immunosuppression due to malignancy, drug administration, or HIV infection. Radiation or surgery of the spinal cord may also trigger secondary infection.
CLINICAL FEATURES
Chickenpox is characterized by the appearance of a maculopapular skin rash. Typically, lesions arise on the trunk and spread to the face and limbs. The skin lesions may be preceded or accompanied by small (less than 5 mm diameter) oral ulcers in the palate and fauces.
The reactivation of VZV in herpes zoster produces severe pain which is followed within 24 hours by the appearance of vesiculobullous lesions (100–102). The trigeminal nerve is affected in about 15% of cases of zoster. The vesicular eruption is characteristically unilateral and limited to the mucosa and skin of one division of the trigeminal nerve. The infection heals with scarring but some patients may develop postinflammatory pigmentation and residual sensory deficit.
DIAGNOSIS
The clinical presentation is usually sufficiently characteristic to enable diagnosis. Confirmation of infection can be made by virus isolation in cell culture or immunofluorescence on a smear from a recent lesion.
MANAGEMENT
Chickenpox does not usually require any treatment, although bed rest and patient isolation are advised during the active phase of the disease.
Although shingles is self-limiting, antiviral therapy should be considered in cases that present within the first 48 hours of onset of symptoms. In the past, treatment with acyclovir (aciclovir) (800 mg tablet five times daily for 7–10 day/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


