Intraoral Anatomy
The radiographic recognition of disease requires a sound knowledge of the radiographic appearance of normal structures. Intelligent diagnosis mandates an appreciation of the wide range of variation in the appearance of normal anatomic structures. Similarly, most patients demonstrate many of the normal radiographic landmarks, but it is a rare patient who shows them all. The absence of one or even several such landmarks in any individual should not necessarily be considered abnormal.
Teeth
Teeth are composed primarily of dentin, with an enamel cap over the coronal portion and a thin layer of cementum over the root surface (Fig. 8-1). The enamel cap characteristically appears more radiopaque than the other tissues because it is the most dense, naturally occurring substance in the body. Because it is 90% mineral, it causes the greatest attenuation of x-ray photons. Its radiographic appearance is uniformly opaque and without evidence of the fine structure. Only the occlusal surface reflects the complex gross anatomy. The dentin is about 75% mineralized, and because of its lower mineral content, its radiographic appearance is roughly comparable to bone. Dentin is smooth and homogeneous on radiographs because of its uniform morphologic features. The junction between enamel and dentin appears as a distinct interface that separates these two structures. The thin layer of cementum on the root surface has a mineral content (50%) comparable to dentin. Cementum is not usually apparent radiographically because the contrast between it and dentin is so low and the cementum layer is so thin.
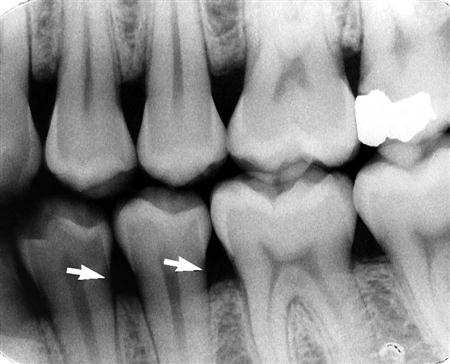
Diffuse radiolucent areas with ill-defined borders may be apparent radiographically on the mesial or distal aspects of teeth in the cervical regions between the edge of the enamel cap and the crest of the alveolar ridge (Fig. 8-2). This phenomenon, called cervical burnout, is caused by the normal configuration of the affected teeth, which results in decreased x-ray absorption in the areas in question. Close inspection reveals intact edges of the proximal surfaces. The perception of these radiolucent areas results from the contrast with the adjacent, relatively opaque enamel and alveolar bone. Such radiolucencies should be anticipated in almost all teeth and should not be confused with root surface caries, which frequently have a similar appearance.
The pulp of normal teeth is composed of soft tissue and consequently appears radiolucent. The chambers and root canals containing the pulp extend from the interior of the crown to the apices of the roots. Although the shape of most pulp chambers is fairly uniform within tooth groups, great variations exist among individuals in the size of the pulp chambers and the extent of pulp horns. The practitioner must anticipate such variations in the proportions and distribution of the pulp and verify them radiographically when planning restorative procedures.
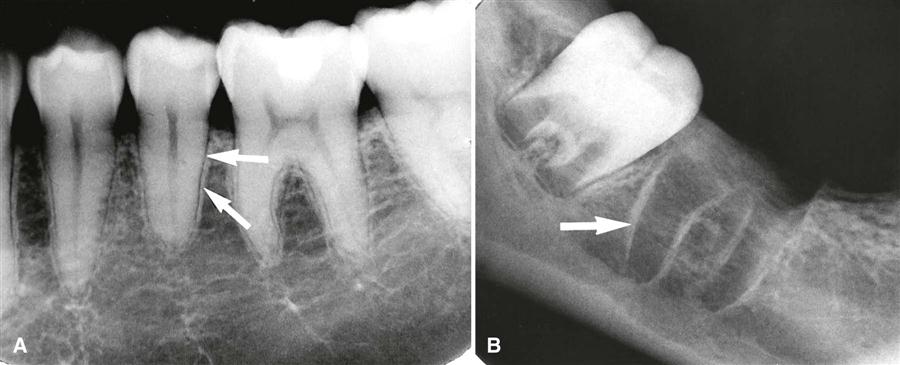
In normal, fully formed teeth, the root canal may be apparent, extending from the pulp chamber to the apex of the root. An apical foramen is usually recognizable (Fig. 8-3). In other normal teeth, the canal may appear constricted in the region of the apex and not discernible in the last 1 mm or so of its length (Fig. 8-4). In this case, the canal may occasionally exit on the side of the tooth, just short of the radiographic apex. Lateral canals may occur as branches of an otherwise normal root canal. They may extend to the apex and end in a normal, discernible foramen or may exit the side of the root. In either case, two or more terminal foramina might cause endodontic treatment to fail if they are not identified.
At the end of a developing tooth root, the pulp canal diverges, and the walls of the root rapidly taper to a knife edge (Fig. 8-5). In the recess formed by the root walls and extending a short distance beyond is a small, rounded, radiolucent area in the trabecular bone, surrounded by a thin layer of hyperostotic bone. This is the dental papilla bounded by its bony crypt. The papilla forms the dentin and the primordium of the pulp. When the tooth reaches maturity, the pulpal walls in the apical region begin to constrict and finally come into close apposition. Awareness of this sequence and its radiographic pattern is often useful in evaluating the stage of maturation of the developing tooth; it also helps avoid misidentifying the apical radiolucency as a periapical lesion.
In a mature tooth, the shape of the pulp chamber and canal may change. A gradual deposition of secondary dentin occurs with aging. This process begins apically, proceeds coronally, and may lead to pulp obliteration. Trauma to the tooth (e.g., from caries, a blow, restorations, attrition, or erosion) also may stimulate dentin production, leading to a reduction in size of the pulp chamber and canals. Such cases usually include evidence of the source of the pathologic stimulus. However, in the case of a blow to the teeth, only the patient’s recollection may suggest the true reason for the reduced pulp chamber size.
Supporting Structures
Lamina Dura
A radiograph of sound teeth in a normal dental arch demonstrates that the tooth sockets are bounded by a thin radiopaque layer of dense bone (Fig. 8-6). Its name, lamina dura (“hard layer”), is derived from its radiographic appearance. This layer is continuous with the shadow of the cortical bone at the alveolar crest. It is only slightly thicker and no more highly mineralized than the trabeculae of cancellous bone in the area. Its radiographic appearance is caused by the fact that the x-ray beam passes tangentially through many times the thickness of the thin bony wall, which results in its observed attenuation (the eggshell effect). Developmentally, the lamina dura is an extension of the lining of the bony crypt that surrounds each tooth during development.
The appearance of the lamina dura on radiographs may vary. When the x-ray beam is directed through a relatively long expanse of the structure, the lamina dura appears radiopaque and well defined. When the beam is directed more obliquely, the lamina dura appears more diffuse and may not be discernible. In fact, even if the supporting bone in a healthy arch is intact, identification of a lamina dura completely surrounding every root on each film is frequently difficult, although it usually is evident to some extent about the roots on each film (Fig. 8-7). In addition, small variations and disruptions in the continuity of the lamina dura may result from superimpositions of cancellous bone and small nutrient canals passing from the marrow spaces to the periodontal ligament (PDL).
The thickness and density of the lamina dura on the radiograph vary with the amount of occlusal stress to which the tooth is subjected. The lamina dura is wider and more dense around the roots of teeth in heavy occlusion and thinner and less dense around teeth not subjected to occlusal function.
The appearance of the lamina dura is a valuable diagnostic feature. The presence of an intact lamina dura around the apex of a tooth strongly suggests a vital pulp. However, because of the variable appearance of the lamina dura, the absence of its image around an apex on a radiograph may be normal. Rarely, the lamina dura may be absent from a molar root extending into the maxillary sinus in the absence of disease. Therefore, the clinician is advised to consider other signs and symptoms as well as the integrity of the lamina dura when establishing a diagnosis and treatment.
Alveolar Crest
The gingival margin of the alveolar process that extends between the teeth is apparent on radiographs as a radiopaque line—the alveolar crest (Fig. 8-8). The level of this bony crest is considered normal when it is not more than 1.5 mm from the cementoenamel junction of the adjacent teeth. The alveolar crest may recede apically with age and show marked resorption with periodontal disease. Radiographs can demonstrate only the position of the crest; determining the significance of its level is primarily a clinical problem (see Chapter 19).
The length of the normal alveolar crest in a particular region depends on the distance between the teeth in question. In the anterior region, the crest is reduced to only a point of bone between the close-set incisors. Posteriorly, it is flat, aligned parallel with and slightly below a line connecting the cementoenamel junctions of the adjacent teeth. The crest of the bone is continuous with the lamina dura and forms a sharp angle with it. Rounding of these sharp junctions is indicative of periodontal disease.
The image of the crest varies from a dense layer of cortical bone to a smooth surface without cortical bone. In the latter case, the trabeculae at the surface are of normal size and density. In the posterior regions, this range of radiodensity of the crest is presumed to be normal if the bone is at a proper level in relation to the teeth. However, the absence of an image of cortex between the incisors is considered by many to be an indication of incipient disease, even if the level of the bone is not abnormal.
Periodontal Ligament Space
Because the PDL is composed primarily of collagen, it appears as a radiolucent space between the tooth root and the lamina dura. This space begins at the alveolar crest, extends around the portions of the tooth roots within the alveolus, and returns to the alveolar crest on the opposite side of the tooth (Fig. 8-9).
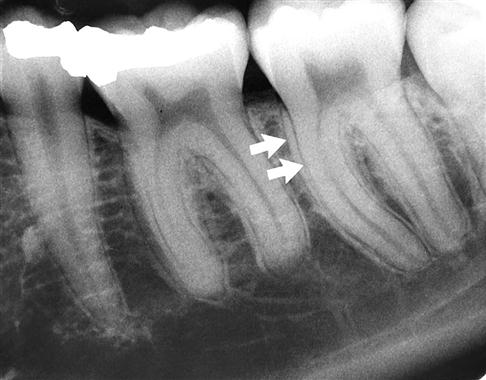
The PDL varies in width from patient to patient, from tooth to tooth in the individual, and even from location to location around one tooth (Fig. 8-10). It is usually thinner in the middle of the root and slightly wider near the alveolar crest and root apex, suggesting that the fulcrum of physiologic movement is in the region where the PDL is thinnest. The thickness of the ligament relates to the degree of function because the PDL is thinnest around the roots of embedded teeth and teeth that have lost their antagonists. The reverse is not true, however, because an appreciably wider space is not regularly observed in persons with especially heavy occlusion or bruxism.
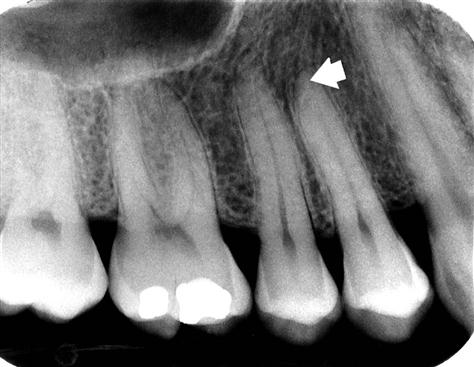
The shape of the tooth creates the appearance of a double PDL space. When the x-ray beam is directed so that two convexities of a root surface appear on a film, a double PDL space is seen (Fig. 8-11). A common example of this double PDL space is seen on the buccal and lingual eminences on the mesial surface of mandibular first and second molar roots.
Cancellous Bone
The cancellous bone (also called trabecular bone or spongiosa) lies between the cortical plates in both jaws. It is composed of thin radiopaque plates and rods (trabeculae) surrounding many small radiolucent pockets of marrow. The radiographic pattern of the trabeculae comes from two anatomic sources. The first is the cancellous bone itself. The second is the endosteal surface of the outer cortical bone where the cancellous bone fuses with the cortical bone. At this surface, trabecular plates are relatively thick and make a significant contribution to the radiographic image. The trabecular pattern shows considerable intrapatient and interpatient variability, which is normal and not a manifestation of disease. To evaluate the trabecular pattern in a specific area, the practitioner should examine the trabecular distribution, size, and density and compare them throughout both jaws and especially with the corresponding region on the opposite side. This comparison frequently demonstrates that a particularly suspect region is characteristic for the individual.
The trabeculae in the anterior maxilla are typically thin and numerous, forming a fine, granular, dense pattern (Fig. 8-12), and the marrow spaces are consequently small and relatively numerous. In the posterior maxilla, the trabecular pattern is usually quite similar to the pattern in the anterior maxilla, although the marrow spaces may be slightly larger.
In the anterior mandible, the trabeculae are thicker than in the maxilla, resulting in a coarser pattern (Fig. 8-13) with trabecular plates that are oriented more horizontally. The trabecular plates are also fewer than in the maxilla, and the marrow spaces are correspondingly larger. In the posterior mandible, the periradicular trabeculae and marrow spaces may be comparable to those in the anterior mandible but are usually larger (Fig. 8-14). The trabecular plates also are oriented mainly horizontally in this region. Below the apices of the mandibular molars, the number of trabeculae dwindles still more. In some cases, the area from just below the molar roots to the inferior border of the mandible may appear to be almost devoid of trabeculae. The distribution and size of the trabeculae throughout both jaws show a relationship to the thickness (and strength) of the adjacent cortical plates. It may be speculated that where the cortical plates are thick (e.g., in the posterior region of the mandibular body), internal bracing by the trabeculae is not required, so there are relatively few except where required to support the alveoli. By contrast, in the maxilla and anterior region of the mandible, where the cortical plates are relatively thin and less rigid, trabeculae are more numerous and lend internal bolstering to the jaw. Occasionally, the trabecular spaces in this region are very irregular, with some so large that they mimic pathologic lesions.
If trabeculae are apparently absent, suggesting the presence of disease, it is often revealing to examine previous radiographs of the region in question. This helps determine whether the current appearance represents a change from a prior condition. An abnormality is more likely when the comparison indicates a change in the trabecular pattern. If prior films are unavailable, it is frequently useful to repeat the radiographic examination at a reduced exposure because this often demonstrates the presence of an expected but sparse trabecular pattern that was overexposed and burned out in the initial projection. Finally, if prior films are unavailable and reduced exposure does not allay the examiner’s apprehension, it may be appropriate to expose another radiograph at a later time to monitor for ominous changes. Considerable variation may exist in trabecular patterns among patients, so examining all regions of the jaws is important in evaluating a trabecular pattern for any individual. This examination enables the dentist to determine the general nature of the particular pattern and whether any areas deviate appreciably from that norm.
The buccal and lingual cortical plates of the mandible and maxilla do not cast a discernible image on periapical radiographs.
Maxilla
Intermaxillary Suture
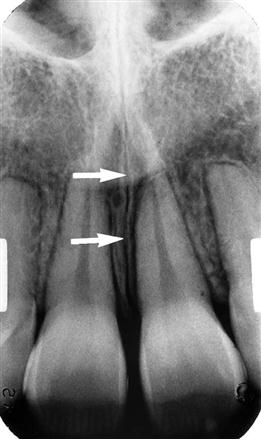
The intermaxillary suture (also called the median suture) appears on intraoral periapical radiographs as a thin radiolucent line in the midline between the two portions of the premaxilla (Fig. 8-15). It extends from the alveolar crest between the central incisors superiorly through the anterior nasal spine and continues posteriorly between the maxillary palatine processes to the posterior aspect of the hard palate. It is not unusual for this narrow radiolucent suture to terminate at the alveolar crest in a small rounded or V-shaped enlargement (Fig. 8-16). The suture is limited by two parallel radiopaque borders of thin cortical bone on each side of the maxilla. The radiolucent region is usually of uniform width. The adjacent cortical margins may be either smooth or slightly irregular. The appearance of the intermaxillary suture depends on both anatomic variability and the angulation of the x-ray beam through the suture.
Anterior Nasal Spine
The anterior nasal spine is most frequently demonstrated on periapical radiographs of the maxillary central incisors (Fig. 8-17). Located in the midline, it lies approximately 1.5 to 2 cm above the alveolar crest, usually at or just below the junction of the inferior end of the nasal septum and the inferior outline of the nasal aperture. It is radiopaque because of its bony composition, and it is usually V-shaped.
Nasal Aperture
Because the air-filled nasal aperture (and cavity) lies just above the oral cavity, its radiolucent image may be apparent on intraoral radiographs of the maxillary teeth, especially in central incisor projections. On periapical radiographs of the incisors, the inferior border of the fossa aperture appears as a radiopaque line extending bilaterally away from the base of the anterior nasal spine (Fig. 8-18). Above this line is the radiolucent space of the inferior portion of the cavity. If the radiograph was made with the x-ray beam directed in the sagittal plane, the relatively radiopaque nasal septum is seen arising in the midline from the anterior nasal spine (Fig. 8-19). The shadow of the septum may appear wider than anticipated an/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses