Immediate Implant Placement and Provisionalization of Maxillary Anterior Single Implants
At the conclusion of this chapter, the reader will be able to:
 . Recognize prognostic factors that are esthetically important for anterior implants
. Recognize prognostic factors that are esthetically important for anterior implants
 . Accurately diagnose the conditions of the failing tooth
. Accurately diagnose the conditions of the failing tooth
 . Perform appropriate patient selection for immediate implant placement and provisionalization in the anterior maxillary region
. Perform appropriate patient selection for immediate implant placement and provisionalization in the anterior maxillary region
 . Demonstrate proficiency in the immediate implant placement and provisionalization procedures
. Demonstrate proficiency in the immediate implant placement and provisionalization procedures
The impending loss of a single tooth in the esthetic zone of an otherwise healthy periodontium can be a distressing experience for patients.1,2 In such a circumstance, the right procedure can make all the difference. In 1998 Wohrle first demonstrated success with immediate implant placement and provisionalization (IIPP) of single anterior maxillary implants, and then others followed.1,3,4–15 One of the most desirable features of IIPP is its efficacy in optimizing esthetic success by preserving the existing osseous and gingival architecture.1,3,16,17
The esthetic success of IIPP procedures is influenced by a number of factors that can be identified as intrinsic or extrinsic.18 Intrinsic factors are patient dependent and include the relationship between hard and soft tissues, gingival biotype, and sagittal root position in the alveolar bone.19,20 Extrinsic factors, on the other hand, are clinician dependent and include three-dimensional (3D) implant positioning and angulation and contouring of the abutment and provisional restoration.16,19
Diagnosis and Treatment Planning
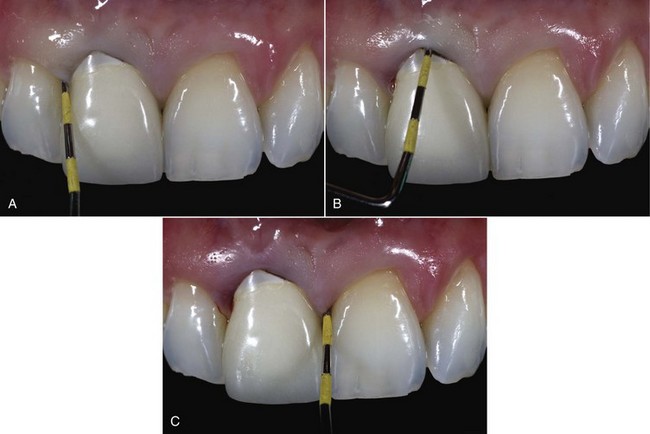
1. Gingival level: The gingival level of the failing tooth should be (1) the same as (or more coronal than) that of the contralateral tooth and (2) harmonious with adjacent dentition, because some gingival recession can be expected after the procedure (Figure 8-1).1 Therefore, when the gingival level of the failing tooth is more apical than that of the contralateral tooth, orthodontic forced eruption, if possible, should be implemented before IIPP.21
2. Osseous-gingival tissue relationship: The osseous-gingival tissue relationship can be evaluated by bone sounding, which entails probing until the bone crest is detected. The bone sounding measurement is the distance between the soft tissue crest and the bone crest. When the bone sounding measurements on the facial and proximal aspects of the tooth are about 3 and 4.5 mm, respectively, they are considered “normal crest.”19 When the bone sounding measurements are greater or less than “normal,” they are classified as “low crest” or “high crest,” respectively.19 With a low crest, tissue recession tends to occur after extraction, with or without immediate implant placement.19 Therefore, for IIPP the bone sounding measurements should be 3 mm on the facial aspect of the failing tooth and 4.5 mm on the proximal aspect of adjacent teeth (Figure 8-2). Depending on the gingival level, a compromised osseous-gingival relationship can be improved by orthodontic or periodontal treatments, or both.
3. Gingival biotype: The gingival biotype can be assessed during bone sounding and categorized according to the visibility of the underlying periodontal probe (SE Probe SD12 Yellow; American Eagle Instruments, Missoula, Montana) through the gingival tissue. If the probe is visible, the patient has a thin biotype; if it is not visible, the patient has a thick biotype (see Figure 8-2).22,23 A thin gingival biotype, which has been shown to sustain more tissue recession after surgical insults than a thick biotype, can be enhanced by using a bilaminar subepithelial connective tissue graft (SCTG) at the time of IIPP.18
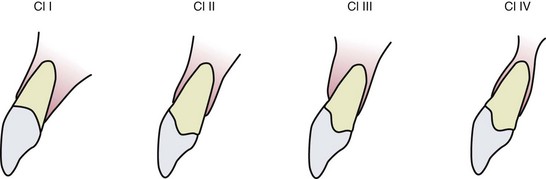
4. Sagittal root position (SRP): The sagittal root position of the failing tooth in the alveolar bone can be identified with cone beam computed tomography (CBCT) and can be categorized as one of four different classes (Box 8-1 and Figure 8-3).20 Because changing the SRP is impractical, it is important for practitioners to recognize cases that are favorable for IIPP (Class I SRP), cases that are more technique sensitive and entail additional attention (Class II and Class III SRP), and cases in which IIPP is contraindicated and hard and/or soft tissue augmentation is required before implant placement (Class IV SRP).20
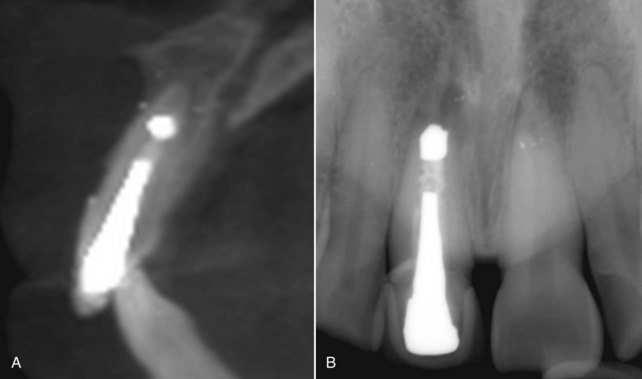
5. Buccolingual width and interradicular mesiodistal widths: The buccolingual width and interradicular mesiodistal widths of the failing tooth determine the diameter of the implant to be used. These widths can be evaluated using CBCT and periapical radiographs (Figure 8-4).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses