8
Imaging for sleep-related breathing disorders
CONCEPTUAL OVERVIEW
Imaging of the airway and related structures is used for a variety of reasons. For the most part, imaging has been utilized in an effort to measure anatomical structures of the airway, to understand the dynamics of the airway with and without therapeutic interventions, and to better understand the pathophysiology of sleep-related breathing disorders (SRBD).
In the dental management of SRBD, the use of imaging to predict whether an individual may be at risk for obstructive sleep apnea (OSA) or snoring is limited at this time. As techniques are developed and refined, the possible use of imaging may be of some benefit. Currently, imaging as it relates to the diagnosis of upper airway compromise as well as to assess the dynamics of airway collapse is mainly for research purposes.
IMAGING IN THE DENTAL OFFICE FOR SRBD
The use of imaging associated with the treatment of SRBD in dentistry may be considered in three circumstances:
There are a number of imaging options for the dentist to consider related to these three circumstances (Table 8.1).
Table 8.1 Imaging options related to sleep-related breathing disorders and mandibular repositioning.
| Condition | Imaging option |
| Predict SRBD | Cephlalometric X-ray |
| Cone beam CT | |
| Pharyngometry | |
| Assess condition of dental and related structures | Panoramic X-ray |
| Cephalometric X-ray | |
| Cone beam CT | |
| Cone beam CT | |
| Determine if mandibular repositioning will improve the airway | Pharyngometry |
The three most common imaging options that can be utilized are computed tomography (CT), magnetic resonance imaging (MRI), and nasalpharyngoscopy. These modalities are used on a limited basis and typically are not employed in the treatment of SRBD.
Computed tomography and magnetic resonance imaging
CT and MRI scans may be useful if other pathology is being investigated as a possible factor in patients with sleep disorders. These imaging modalities have been shown to be resourceful when a secondary medical or neurological cause for a sleep disorder was suspected.1, 2
CT is frequently employed by the otolaryngologist to evaluate the nasal airway and the sinuses, particularly for discerning the presence of any airway compromise from craniofacial structures.
CT has also been utilized to do research regarding the airway. A study using dynamic CT determined the impact of an OA on the airway, in particular examining the effect of the OA as it advanced the mandible, also known as anterior or mandibular repositioning, from its habitual maxillomandibular relationship.3 The results demonstrated that the OA appeared to have a greater impact on the lateral aspect of the airway in the retropalatal and retroglossal areas.
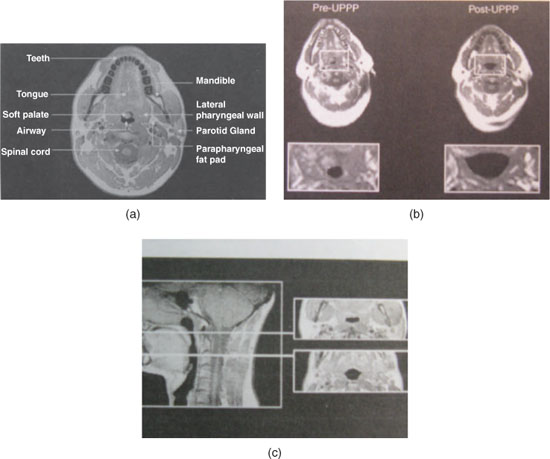
MRI has been used extensively to study the dynamics of the upper airway in a variety of circumstances (Figure 8.1).4, 5 This particular imaging modality is not practical, nor it is indicated in everyday clinical use on a routine basis. It needs to be utilized in specific circumstances mostly related to research endeavors. It would be infrequent for the dentist to order this imaging modality for clinical purposes because of the associated expense to the patient, the difficulty for patients to initiate and maintain sleep in the noisy scanner, and the potential exclusion of some patients with metallic implants or pacemakers.
Figure 8.1 Cross-section MRI views of the airway: (a) general view, (b) the airway pre- and post-uvulopalatopharyngoplasty surgery, and (c) the airway at two levels: retropalatal and retroglossal. (Lee-Chiong T, ed. Sleep: A Comprehensive Handbook. Hoboken, NJ: John Wiley & Sons. 2006. Used with permission).
Nasalpharyngoscopy (fiber optic pharyngoscopy)
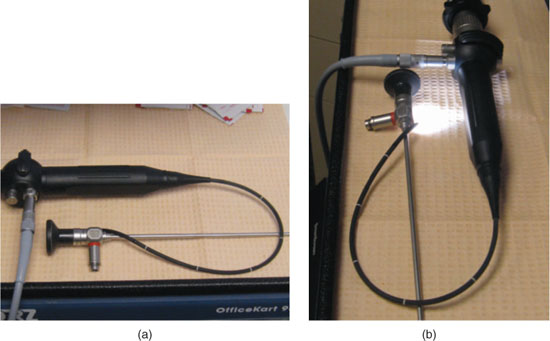
Nasalpharyngoscopy, also known as fiber optic pharyngoscopy, is frequently used by the otolaryngologist to evaluate the airway. A flexible tube with a fiber optic light and camera allow for both dynamic and state–dependent visualization of the airway from the nose down to the larynx (Figure 8.2).
During this evaluation, the effect of inspiration with the nose and mouth closed, termed the Mueller maneuver, is observed.6 This clinical technique replicates the effect of obstructive events in the airway, thereby indicating the impact of apnea events on the airway as well as identifying the specific site of obstruction associated with OSA. One study found that 60% of the sleep apnea patients had complete occlusion of the airway, 40% had multiple sites of obstruction, and there was reduced size along with increased collapsibility of the airway that correlated with an increase in the apnea–hypopnea index.7
Figure 8.2 View of rigid and flexible fiberoptic scope used to visualize the nasal airway and oropharynx down to the level of the epiglottis: (a) the rigid and flexible scopes and (b) the scopes showing the illumination.
Pharyngometry
Pharyngometry, also known as acoustic reflection imaging (ARI), is another technique that has been utilized to evaluate the airway in patients with OSA and/or snoring (Figure 8.3). This modality emits a sound wave through the mouth that is helpful in the identification of the site(s) of narrowing from the oropharyngeal junction to the hypopharynx.
ARI may also determine the impact of mandibular repositioning on the airway and to what extent tongue space may increase. The technique for this modality is not standardized in terms of how it is performed, and it is therefore subject to the procedural handling by each individual user. The advantage of ARI is that it may assist the dentist in determining the potential for the success of OA therapy.8 It was demonstrated that when the airway volume was increased as measured by ARI, there was a 60% chance that an OA would have a favorable prognosis. If the airway volume was unchanged, the possibility that an OA would not be of benefit was 95%. This modality may also be helpful with the postinsertion assessment of the OA relative to whether any further adjustments to the therapeutically induced maxillomandibular relationship may be helpful or necessary.
One study found that ARI could assist in predicti/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


