8
Development of periodontal diseases
Figure 8.1 Pristine gingiva. This state of fastidious oral hygiene is rarely achieved clinically. There is very sparse neutrophil migration into the sulcus and no inflammatory response.
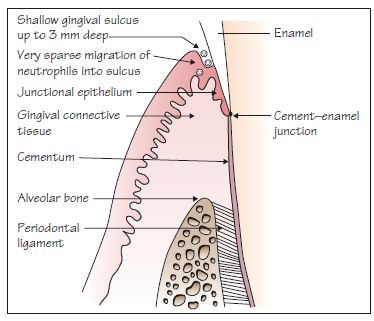
Figure 8.2 An initial lesion.
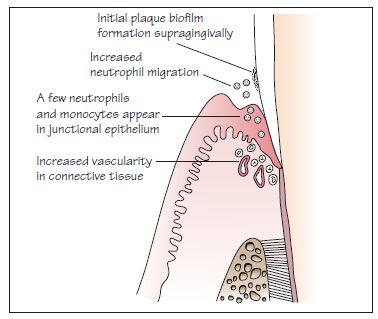
Figure 8.3 Clinically healthy gingiva in a 19-year-old female.

Figure 8.4 An early lesion.
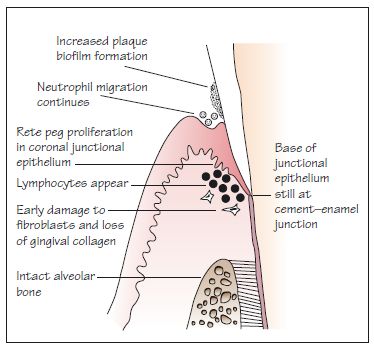
Figure 8.5 An established lesion.
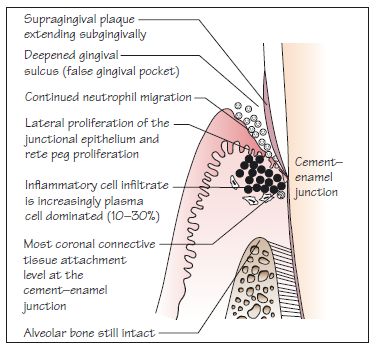
Figure 8.6 Clinical plaque-induced gingivitis. There is visible plaque, blunted interdental papillae, and the marginal gingiva are red, slightly swollen and inflamed.

Figure 8.7 An ‘advanced’ lesion (note ‘advanced’ here is a descriptor of the stage of histological lesion not a descriptor of clinical severity) showing incipient periodontitis: true shallow periodontal pockets (4–5 mm); CAL of 1–2 mm; and incipient alveolar bone loss (horizontal), with the formation of a suprabony pocket.
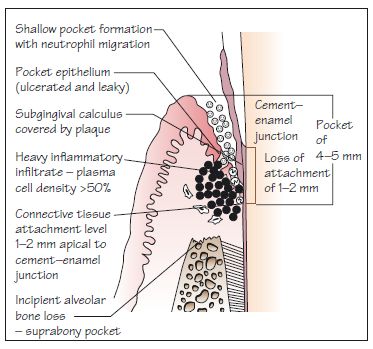
Figure 8.8 An ‘advanced’ lesion (note ‘advanced’ here is a descriptor of the stage of histological lesion not a descriptor of clinical severity) showing moderate periodontitis: typically, true deep periodontal pockets (6 mm or more) and CAL of 3–4 mm are present; alveolar bone loss may be vertical, rather than horizontal, with the formation of an infrabony pocket. Note that 5 mm or more of CAL is considered to be severe.
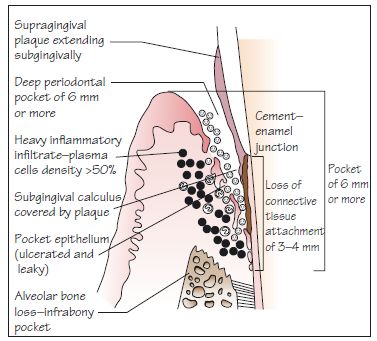
Figure 8.9 Patient with moderate chronic periodontitis showing swollen, inflamed gingivae and recession/clinical attachment loss. The gingival margins are blunted and there is loss of contour.

Following the fifth European Workshop on Periodontology in 2005, the consensus view was that gingivitis and periodontitis are a continuum of the same chronic inflammatory condition that affects the supporting structures of the teeth. It was concluded that: (i) gingivitis may be more important than previou/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


