Craniomaxillofacial Trauma Surgery
• Subcondylar Mandibular Fracture
• Combined Mandibular Parasymphysis and Angle Fractures
• Zygomaticomaxillary Complex Fracture
• Naso-Orbital-Ethmoid Fracture
• Le Fort II and III Fractures
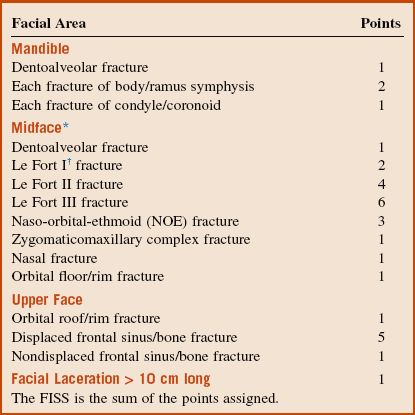
The Facial Injury Severity Scale (FISS) is a tool recently devised for designation of the severity of facial injuries (Box 8-1). The result is a numeric value that is the sum of all facial fractures and fracture patterns. The FISS is a predictor of the severity of facial injury as measured by the operating room charges required for treatment and the length of hospital stay.
The Glasgow Coma Score is a universally used system for evaluation of neurologic status (Box 8-2).
Dentoalveolar Trauma
PMHX/PDHX/Medications/Allergies/SH/FH
The patient denies any significant cardiac, pulmonary, renal, hepatic, or neurologic diseases.
Examination
Intraoral. There is a 1-cm abrasion of the upper lip skin without significant laceration. Intraorally, there is profound ecchymosis of the upper lip mucosa with a laceration extending into the sublabial vestibule (Figure 8-1). Teeth #7 and #8 are mobile as a single unit with displacement of the buccal cortical plate on manipulation. Tooth #9 is grossly mobile and subluxed several millimeters. It also demonstrates an oblique coronal fracture with pinpoint pulp exposure (Ellis class III). In addition, tooth #9 is sensitive to mechanical stimulation with a cotton-tipped applicator and tender to percussion. There is occlusal prematurity with interference of the maxillary anterior teeth on attempted intercuspation.
Imaging
A maxillofacial CT scan demonstrates an alveolar segment fracture involving teeth #7 and #8, with subluxation of tooth #9 and fracture of the alveolar plate (Figure 8-2). There are otherwise no injuries to the maxillofacial skeleton, cervical spine, brain, or cranium. The minimum radiographic study necessary for diagnosis of dentoalveolar fractures is a periapical radiograph, although the diagnosis can often be made with a physical examination alone. Based on availability, other radiographic studies may include:
Treatment
Initial stabilization includes reduction of the teeth and splinting (Figure 8-3). With the current patient, bonded flexible wire splinting was not available, so the teeth were splinted with an arch bar. The occlusion was checked, and the teeth were not in occlusion during maximum intercuspation. The patient’s tetnus status was up to date. He was given a prescription for amoxicillin and chlorhexidine and discharged home. The teeth were splinted for 8 weeks because of the alveolar segment fracture. Root canal therapy was initiated on day 10 with calcium hydroxide therapy.
Complications
In the past, only about 25% to 40% of replanted, avulsed teeth show periodontal ligament (PDL) healing. This has been attributed to poor handling of the tooth. Three different types of posttraumatic external root resorption have been distinguished in the literature: surface resorption (repair-related root resorption), inflammatory resorption (infection-related root resorption) and replacement resorption (ankylosis-related root resorption). Surface resorption has no significant clinical consequences and can be observed. However, the other types of resorption can ultimately result in tooth loss. In the avulsed tooth, if the PDL that is still attached to the tooth does not dry out, the cells can remain viable for an extended period, depending on the storage medium. Once the tooth has been reimplanted and stabilized, the viable PDL cells reattach to the PDL within the socket. When the injury to the cementum of the root is localized, there is minimal destructive inflammation, allowing for new cementum to be laid down after the inflammation resolves. When there is poor handling of the avulsed tooth (e.g., drying or storage in nonphysiologic solutions), damage and necrosis of the PDL occur. Subsequently, there is a large area of inflammation to remove the damaged PDL and cementum. This must be replaced by new tissue. The slower moving cementoblasts compete with the osteoblasts in the replacement process, resulting in some areas of the root surface being replaced by bone. Over time, through osseous remodeling, this can result in osseous or replacement resorption. Internal root resorption can occur through persistent inflammation or metaplastic replacement of normal pulp tissue. This can result in late tooth fractures. Root surface treatments and root canal therapy are directed toward prevention of this complication. Ideal management of dentoalveolar trauma may have to be delayed due to life-threatening injuries that must be managed first (Figure 8-4). This may result in resorptive complications.
Discusson
Dentoalveolar injuries have been classified by the International Association of Dental Traumatology, which regularly reviews and updates its guidelines and publishes them online at www.dentaltraumaguide.org. Broadly, the discrete categories of dentoalveolar injury include:
Periodontal Injuries
Periodontal injuries may be classified according to the following system.
Subluxation. Increased mobility of the tooth without dislocation. Treatment is conservative, although a flexible splint may be applied for the patient’s comfort for up to 2 weeks (Box 8-3).
Dental Crown and Root Injuries
Injuries to the dental crown and root are classified as follows:
Injuries to the Alveolar Bone
Injuries to the supporting alveolar bone are classified as follows:
• Comminution of the alveolar socket: Crushing and comminution can be isolated or associated intrusive and lateral luxation.
• Fracture of the alveolar socket wall: Fracture of the alveolar socket isolated to the facial or lingual wall.
• Fracture of the alveolar process: May be isolated or associated with the socket wall.
• Fracture of the mandible or maxilla: Fracture involving the base of the mandible or maxilla combined with the alveolar process.
Andersson, LJ, Friskopp, J, Blomlof, L. Fiber-glass splinting of traumatized teeth. ASDC J Dent Child. 1983; 50(1):21–24.
Andreasen, JO. Effect of extra-alveolar period and storage media upon periodontal and pulpal healing after replantation of mature permanent incisors in monkeys. Int J Oral Surg. 1981; 10(1):43–53.
Andreasen, JO. Traumatic dental injuries: a manual, ed 3. Chichester, West Sussex, UK: Wiley-Blackwell; 2011.
Andreasen, JO, Borum, MK, Jacobsen, HL, et al. Replantation of 400 avulsed permanent incisors. 4. Factors related to periodontal ligament healing. Endod Dent Traumatol. 1995; 11(2):76–89.
Andreasen, JO, Andreasen, FM, Andersson, L, et al. Textbook and color atlas of traumatic injuries to the teeth, ed 4. Oxford, UK: Blackwell Munksgaard; 2007.
Andreasen, JO, et al. The dental trauma guide. www. dentaltraumaguide. org, 2012.
Blomlof, L. Milk and saliva as possible storage media for traumatically exarticulated teeth prior to replantation. Swed Dent J Suppl. 1981; 8:1–26.
Bystrom, AR, Claesson, R, Sundqvist, G. The antibacterial effect of camphorated paramonochlorophenol, camphorated phenol and calcium hydroxide in the treatment of infected root canals. Endod Dent Traumatol. 1985; 1(5):170–175.
Centers for Disease Control and PreventionAtkinson W, Wolfe S, Hamborsky J, eds. Epidemiology and prevention of vaccine-preventable diseases, ed 12, Washington DC: Public Health Foundation, 2012.
Chen, JW. Cervical spine injuries. Oral Maxillofac Surg Clin North Am. 2008; 20(3):381–391.
Cohenca, N, Simon, JH, Roges, R, et al. Clinical indications for digital imaging in dento-alveolar trauma. Part 1. Traumatic injuries. Dent Traumatol. 2007; 23(2):95–104.
Cvek, M, Cleaton-Jones, P, Austin, J, et al. Pulp revascularization in reimplanted immature monkey incisors: predictability and the effect of antibiotic systemic prophylaxis. Endod Dent Traumatol. 1990; 6(4):157–169.
Cvek, M, Cleaton-Jones, P, Austin, J, et al. Effect of topical application of doxycycline on pulp revascularization and periodontal healing in reimplanted monkey incisors. Endod Dent Traumatol. 1990; 6(4):170–176.
Diangelis, AJ, Andreasen, JO, Ebeleseder, KA, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries. Part 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012; 28(1):2–12.
Elias, H, Baur, DA. Management of trauma to supporting dental structures. Dent Clin North Am. 2009; 53(4):675–689.
Filippi, A, Pohl, Y, von Arx, T. Treatment of replacement resorption with Emdogain: preliminary results after 10 months. Dent Traumatol. 2001; 17(3):134–138.
Fuss, Z, Tsesis, I, Lin, S. Root resorption: diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003; 19(4):175–182.
Gassner, R, Bösch, R, Tuli, T, et al. Prevalence of dental trauma in 6,000 patients with facial injuries: implications for prevention. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87(1):27–33.
Gazelius, B, Olgart, L, Edwall, L. Non-invasive recordings of blood flow in human dental pulp. Endod Dent Traumatol. 1986; 2:219–221.
Gonda, F, Nagase, M, Chen, RB, et al. Replantation: an analysis of 29 teeth. Oral Surg Oral Med Oral Pathol. 1990; 70(5):650–655.
Hiltz, J, Trope, M. Vitality of human lip fibroblasts in milk, Hanks balanced salt solution, and Viaspan storage media. Endod Dent Traumatol. 1991; 7(2):69–72.
Iqbal, MK, Bamaas, N. Effect of enamel matrix derivative (EMDOGAIN) upon periodontal healing after replantation of permanent incisors in beagle dogs. Dent Traumatol. 2001; 17(1):36–45.
Jamal, BT, Diecidue, R, Qutob, A, et al. The pattern of combined maxillofacial and cervical spine fractures. J Oral Maxillofac Surg. 2009; 67(3):559–562.
Karayilmaz, H, Kirzio lu, Z. Comparison of the reliability of laser Doppler flowmetry, pulse oximetry and electric pulp tester in assessing the pulp vitality of human teeth. J Oral Rehabil. 2011; 38(5):340–347.
lu, Z. Comparison of the reliability of laser Doppler flowmetry, pulse oximetry and electric pulp tester in assessing the pulp vitality of human teeth. J Oral Rehabil. 2011; 38(5):340–347.
Kehoe, JC. Splinting and replantation after traumatic avulsion. J Am Dent Assoc. 1986; 112(2):224–230.
Kloss, F, Laimer, K, Hohlrieder, M, et al. Traumatic intracranial haemorrhage in conscious patients with facial fractures: a review of 1,959 cases. J Craniomaxillofac Surg. 2008; 36(7):372–377.
Malmgren, B, Andreasen, JO, Flores, MT, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries. Part 3. Injuries in the primary dentition. Dent Traumatol. 2012; 28(3):174–182.
Mithani, SK, St. -Hilaire, H, Brooke, BS, et al. Predictable patterns of intracranial and cervical spine injury in craniomaxillofacial trauma: analysis of 4,786 patients. Plast Reconstr Surg. 2009; 123(4):1293–1301.
Needleman, HL. The art and science of managing traumatic injuries to primary teeth. Dent Traumatol. 2011; 27(4):295–299.
Reynolds, JS, Reynolds, MT, Powers, MP. Diagnosis and management of dentoalveolar injuries. In: Fonseca RJ, Walker RV, Barber HD, eds. Oral and maxillofacial trauma. ed 4. St Louis: Saunders; 2013:248–292.
Sjögren, U, Figdor, D, Spangberg, L, et al. The antimicrobial effect of calcium hydroxide as a short-term intracanal dressing. Int Endod J. 1991; 24(3):119–125.
Soder, PO, Otteskog, P, Andreasen, JO, et al. Effect of drying on viability of periodontal membrane. Scand J Dent Res. 1977; 85(3):164–168.
Tronstad, L, Andreasen, JO, Hasselgren, G, et al. pH changes in dental tissues after root canal filling with calcium hydroxide. J Endod. 1981; 7(1):17–21.
Trope, M. Root resorption of dental and traumatic origin: classification based on etiology. Pract Periodontics Aesthet Dent. 1998; 10(4):515–522.
Trope, M. Avulsion and replantation. Refuat Hapeh Vehashinayim. 2002; 19(2):6–15.
Trope, M, Friedman, S. Periodontal healing of replanted dog teeth stored in Viaspan, milk and Hanks balanced salt solution. Endod Dent Traumatol. 1992; 8(5):183–188.
Valente, JH, Forti, RJ, Freundlich, LF, et al. Wound irrigation in children: saline solution or tap water? Ann Emerg Med. 2003; 41(5):609–616.
Wilder-Smith, PEEB. A new method for the non-invasive measurement of pupal blood flow. Int Endod J. 1988; 21:307–312.
Wolfe, RM. Update on adult immunizations. J Am Board Fam Med. 2012; 25(4):496–510.
Yanpiset, K, Trope, M. Pulp revascularization of replanted immature dog teeth after different treatment methods. Endod Dent Traumatol. 2000; 16(5):211–217.
Subcondylar Mandibular Fracture
Examination
General. The patient is a well-developed and well-nourished man in no apparent distress.
Imaging
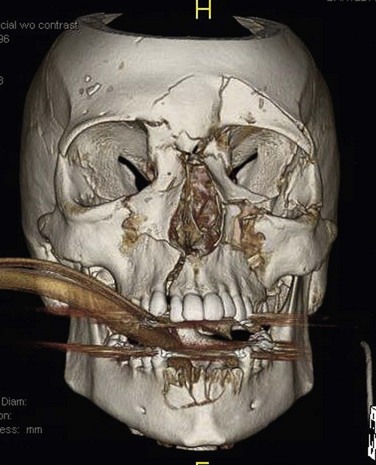
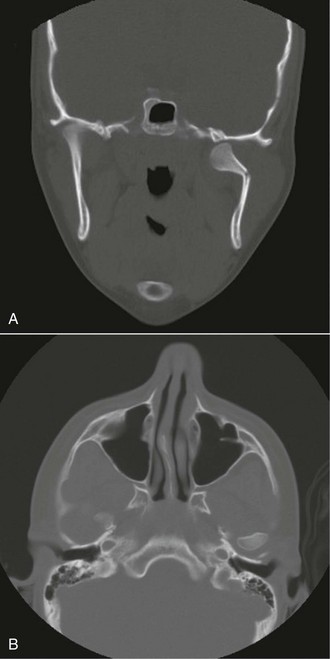
For the current patient, a CT scan was obtained as the initial study. It demonstrated a right subcondylar fracture on coronal and axial views (Figure 8-5). A plain wrist film was also obtained, which revealed a right-sided fracture of the distal radius (Colles fracture).
Treatment
Complications
The complications of treating fractures of the mandibular condyle are well described in the literature and are often used as the basis of comparison for surgical and nonsurgical treatment. One of the most severe late complications can be temporomandibular joint (TMJ) ankylosis (fusion between the mandibular condyle and the glenoid fossa). Patients with TMJ ankylosis often have a history of facial trauma. Prevention of ankylosis was discussed by Zide and Kent in 1983. They advocated appropriate physiotherapy early in the phase of nonsurgical treatment. Other types of late mandibular dysfunction have been cited as complications of closed reduction, including chronic pain, malocclusion, internal derangement, asymmetry, limited mobility, and gross radiographic abnormalities (however, radiographic abnormalities in the absence of pain or functional impairment have no clinical significance). Long-term complications of open reduction and internal fixation (ORIF) are scar perception, facial nerve palsy/paralysis, loss or failure of fixation, Frey’s syndrome, avascular necrosis, TMJ dysfunction, and facial asymmetry. The early complications are few and can include early failure of fixation, malocclusion, pain, and infection.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses