8
Cleft and Craniofacial Surgery
INTRODUCTION
Cleft lip with or without cleft palate occurs with a frequency of 1 in 600 live births, making it one of the most common congenital malformations. The functional and aesthetic consequences associated with both syndromic and nonsyndromic facial clefting are well understood and are routinely addressed in an interdisciplinary fashion to optimize the care of the patient. Despite well-established treatment pathways, significant variation still exists in the surgical techniques used to repair the cleft, though many have shown to have excellent results.1 Fortunately, a patient’s age and the anatomic site of their problem contribute to excellent healing with rare complications so long as the surgery is well executed. Early complications range from wound-specific issues and infection to perioperative and anesthetic problems, while late complications can be best categorized as to their effect on appearance, function, and growth.
It has long been held as a general rule that infants are age appropriate for lip repair according to the “rule of 10’s,” or at roughly 3 months of age. Some studies suggest that acceptable perioperative morbidity can be achieved by 1 week of life. In 2007, Fillies et al. retrospectively examined a cohort of 174 cleft lip and palate patients and were able to correlate anesthetic complication risk with body weight at the time of surgery. Interestingly, their work is reflective of results seen in Wilhelmsen’s 1966 review of morbidity of and mortality in cleft surgery.2,3 Given the possibility of syndromic association with clefts and the lack of data supporting early repair, it is generally recommended that sufficient time be allowed for comprehensive workup and weight gain before definitive repair is accomplished. In most centers, this is somewhere between 3 and 6 months of age.
The preoperative evaluation for a cleft patient is fairly standard and is dictated largely by the requirements to undergo a general anesthetic at a given age and by the comorbidities of a specific patient. At the author’s institution, no blood work (CBC or type and screen) is performed for healthy babies undergoing this procedure. The lip repair itself has little systemic impact to the physiology of the child, and blood loss is minimal during surgery. In fact, many institutions routinely perform cleft lip repair as an outpatient procedure and have demonstrated comparable outcome data with those institutions where these children are admitted as inpatients.1,2,4–7
COMPLICATIONS IN CLEFT LIP REPAIR
Early Complications
Early surgical site complications are uncommon. Despite a relative paucity in the literature of reported early lip repair complications, those most frequently reported include infection, lip dehiscence, flap necrosis, and nasal airway obstruction.8–10
Despite being performed as a clean contaminated surgery, cleft lip repair is generally performed in edentulous patients where the typical oral flora has not yet evolved to contain the multiple anaerobic aerodigestive pathogens seen in adult patients. In fact, the flora in this patient population is considerably more limited as demonstrated by Chuo’s retrospective review of swab culture data in 250 patients with clefts.11 In this study, the predominant pathogens were S. aureus and β-hemolytic streptococcus. They chose to administer prophylactic perioperative antibiotics and/or postpone surgery based on culture-positive data and in patients with other comorbidities (e.g., failure to thrive, malnutrition). Unfortunately, they did not list their infection rate in this cohort despite these measures. One has to weigh cost, risk, and available outcome data when deciding on best practices in the absence of a prospective randomized study. At the author’s institution, perioperative antibiotics are used. While others report the additional use of postoperative antibiotics in noninfected patients, we believe that this is difficult to justify routinely in an era of increasing antibiotic resistance and in a surgery that already carries with it a very low risk of infection.9
Lip dehiscence in the acute setting is rarely a problem with the careful and tension-free construction of all tissue layers in the unilateral or bilateral cleft lip patient. Dehiscence has been attributed to both tension and trauma. Reinisch observed traumatic lip dehiscence in 7 of his 123 reviewed cleft patients (all of these were bilateral but one). Five of these patients were older than 9 months of age and age-related mobility and activity was felt to be the cause of this unfortunate outcome.9 Some surgeons opt to use the Logan bow or arm restraints, though there are no substantive data that demonstrate their effectiveness.12,13
Infants are obligate nasal breathers and in the acute postoperative time period, nasal obstruction can occur due to edema or simply the presence of tissue where there was none previously. This can be further exacerbated in the postoperative period by upper respiratory tract infections. Some of these obstruction issues can be ameliorated by the use of nostril conformers or cut-to-fit cannulae made from endotracheal tubes. This not only helps to prevent obstruction, but the conformer or stent can help to support the redraping of the nasal skin/vestibular tissue when a primary rhinoplasty has been performed.14,15,16 These tubes must be routinely cared for with bulb suction and saline drops, lest they clog with dried mucus themselves.
Clinically, significant postoperative hemorrhage is very uncommon in cleft lip repair. Bleeding can be avoided with meticulous dissection, hemostasis, and closure. Care is taken during surgery to perform the operation with the assistance of infiltrated local anesthetic and vasoconstrictors along with the judicious use of electrocautery. Many perform the surgery with loupe or microscope magnification, making any small bleeding points readily identifiable, and layered closure of mucosa, muscle and skin should all but assure a dry field. A small amount of bleeding is to be expected, especially when a mucosal field is involved in the surgery. This can take place for 1–2 days after surgery and might appear somewhat magnified as it mixes with oral and nasal secretions. A small amount of perinasal, perioral, and periorbital bruising is not uncommon either, depending on the surgical techniques utilized for repair.
Flap necrosis has been reported in bilateral cleft lip and palate patients due to excessive thinning of the prolabial skin in efforts to refine the philtral dimple.8 Interestingly, however, as more aggressive nasal surgery has been reported in the recent past to address the nasal tip and the columella at the time of bilateral cleft lip repair, one would expect that the prolabium is even more at risk. For example, Cutting has described a prolabial unwinding technique to reposition the lower lateral cartilages, and Mulliken described marginal incisions paired with extensive tip undermining and suturing despite reporting the use of an extremely narrow prolabial pedicle and flap.17,18,19 No complications have been reported in any detailed manner using these techniques. This should not imply that these maneuvers are without risk. They should simply be undertaken with a thorough understanding of the local anatomy and the techniques described.
Late Complications
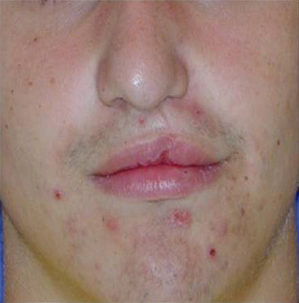
The appearance and function of the repaired cleft lip are greatly impacted by the initial surgery (Fig. 8.1). The simultaneous construction of functional nasal and labial muscles influence the growth and development of the underlying facial skeleton as well as the appearance of the lip.20,21 The eventual form of the lip is the result of both the choice of skin incision and the muscle repair at the initial surgery. Of the various skin incisions that have been used, several, such as the geometric triangular and quadrangular incisions violate the subunits of the upper lip, while modifications of the advancement rotation most accurately replicate normal anatomic structures.22,23,24 While complications classified as “early,” such as infection or dehiscence often lead to sequelae that could be categorized as “late,” many late complications or secondary deformities are the result of avoidable errors in technique or judgment. The end result is suboptimal lip aesthetics that can be difficult to correct.
Fig. 8.1. Nine-year-old boy with left unilateral cleft lip and palate. Note how the nasal asymmetry and vertical deficiency of the lip on the cleft side are part of the same problem. In this case, a muscle reconstruction was not performed at the level of the nose, the medial element was under-rotated, and the lip was left short. A revision here would require recreation of the initial defect and complete reconstruction.

The surgical correction of cleft lip and palate consists of a series of procedures where timing is dependent on both chronological and developmental milestones. The lip repair, consequently, is critical to all procedures that follow it. It is also important to keep in mind that the staged reconstruction of these patients is a stepwise process and that careful consideration must be given to each procedure and its downstream effects including growth.
While the construction of the labial and nasal muscular rings guides the eventual appearance and symmetry of the lip and nose, the individual’s innate ability to heal and scarring tendencies also play key roles in the aesthetic appearance of the repair.20,21 Certain technical shortcomings in the repair can also lead to less than optimal results. The underlying skeletal platform must be considered when evaluating secondary lip deformities, as the presence or absence of a bony alveolar cleft or maxillary hypoplasia greatly impacts the appearance of the nasolabial structures as the child grows. Despite best efforts with soft tissue correction and camouflaging techniques, facial harmony can only be accomplished when these hard tissue problems have been addressed as well. Therefore, it is recommended that, depending on the age of the child and the degree of skeletal dysplasia, soft tissue revisions are sometimes deferred until maxillary bone grafting and/or Le Fort osteotomy have been accomplished.
When evaluating a secondary lip/nose deformity, an understanding of the initial malformation and the goals of primary surgery are important. Understanding the true underlying cause of the secondary deformity and its global functional and aesthetic shortcomings are also crucial. For example, lesser procedures can be used to address minor height mismatches of the white roll, vermilion notching, or vermilion fullness when the muscle is otherwise noted to be functional and united across the cleft. When applied inappropriately, however, these “minor” procedures might only serve to amplify defects, increase scarring, or leave the patient well short of a complete correction. However, a complete takedown of the lip should be considered if there are significant issues with lip height or symmetry, nasal symmetry, substantial vermilion/white roll mismatches, or a dehiscent orbicularis oris. Lastly, when there is significant damage and scarring to the cleft adjacent tissue, especially in the case of the bilateral cleft lip, one may have to recruit nearby tissue to reconstitute the philtral complex and the orbicularis muscular ring.
Cutaneous Lip Problems
Long Upper Lip
The long upper lip is infrequently seen in patients with unilateral cleft lip given the predominance of advancement rotation repairs performed today. Excessive lip length was primarily a problem of the triangular and quadrangular repairs but can be encountered as a result of overzealous rotation in an advancement rotation technique. The long upper lip, however, continues to plague the bilateral patient. While this is somewhat a function of postoperative lip animation and function, the aesthetic result can be visible as a long upper lip. The long lip can be a difficult problem to correct, frequently requiring the horizontal excision of tissue at the supravermilion level or in the subalar region. The scars left by these revisions, though reasonably well camouflaged by the white roll and the alar crease, respectively, are often less than optimal in appearance.
Tight Upper Lip
The tight upper lip can stem from aggressive soft tissue excision at the time of primary or secondary repair, inadequate mobilization of the soft tissues, or be the result of a protuberant premaxilla. The appearance of tissue deficiency can be further mimicked or accentuated by maxillary hypoplasia, or a full lower lip. Further lip revision that includes soft tissue excision might only serve to worsen the problem unless nearby tissue in the form of an Abbé flap is utilized. This pedicled cross-lip flap, based on the labial artery, will add width and appropriate bulk, while decreasing the width differential between the upper and lower lip. The Abbé flap may also be of value when the prolabial tissue has been severely damaged by scar. This technique often has less than desirable aesthetic results, but provides more tissue to the upper lip.
Short Upper Lip
The short upper lip may be the result of several errors in the primary lip repair. Most commonly, it is the result of an under rotated, improperly/incompletely repaired, or dehisced muscle and this will often require a re-repair of the lip (Fig. 8.2). Occasionally, it is the result of exuberant scarring or the sequelae of early infection or dehiscence. In any case, the original repair scar can be used to access the nasal and labial muscles for a more precise functional repair. If conversion to an advancement rotation from a geometric repair is feasible without too much tissue loss, it should be considered, as this places the cutaneous scars in a more natural position. Additionally, Z-plasties can placed at the vermilion-cutaneous junction or at the wet dry line as needed to accomplish aesthetic goals by lengthening the lip.
Fig. 8.2. Teenage boy with left unilateral cleft lip and palate. Note the vertically short lip on the cleft side, the vermilion notch, and the wet-dry line mismatch. This is best approached with complete takedown and reconstruction.
Philtrum Abnormalities
Obliteration of the philtral dimple and Cupid’s bow asymmetries are occasionally seen following primary lip repair. A flat Cupid’s bow is sometimes the result of a triangular repair as well. The philtral dimple can often be preserved in unilateral clefts with minimal cutaneous undermining of the noncleft side at the time of initial repair. This dimple should be respected, as a natural-appearing dimple is quite difficult to restore surgically. Additionally, widening of the scar in the philtral column position can occur as a result of early wound tension (due to inadequate muscle reconstruction), poor suturing, or wound breakdown at the initial repair. This can often be treated with simple excision and augmented with other surface treatments such as surface laser or dermabrasion. In bilateral clefts, the philtrum is often left too wide in conservative attempts to preserve tissue or with stretching that occurs with growth. This can yield an overly wide philtrum that will benefit from a re-repair (Fig. 8.3).
Fig. 8.3. Six-year-old boy with bilateral cleft lip and palate. Note the wide philtral complex and the hypoplastic vermilion in contrast to the robust lateral lip elements. Prolabial vermilion had been utilized in this case for the reconstruction of the red lip. Revision would require recreation of the initial defect, narrowing of the philtrum, and utilization of lateral vermilion flaps to fill out the central lip.

The philtral column(s) are also often left flat. This is largely due to the fact that we cannot surgically recreate the dermal insertions of the orbicularis muscle. We are therefore left to provide surgical camouflage, with carefully everted skin edges, dermal grafts, or local subcutaneous, dermal, or muscular flaps. As previously stated, when the philtrum area has sustained significant damage from the primary repair or a complication thereof, an Abbé flap may be considered.
Cutaneous Defects
Isolated unaesthetic cutaneous lip scarring can be managed in a manner similar to other facial scars, by excision, dermabrasion, or laser resurfacing. One must keep in mind the normal anatomic orientation of the philtral column and other local lip structures. For example, the horizontal orientation of a running W-plasty might not suit this area as well as a wavy line excision to re-create the philtral column in a scar excision. One must also be mindful that the skin of the nose and the skin of the lip are of different quality, much as the skin of the white and red lip. If the skin of the nose has migrated down onto the skin of the upper lip or conversely, the skin of the vermilion has elevated into the cutaneous lip, this must be addressed in the revision (Fig. 8.4).
Fig. 8.4. Two-year-old girl with right unilateral complete cleft lip and palate. Note the mild nasal asymmetry as well as the vermilion cutaneous mismatch, in the face of an adequately full and vertically long lip.

Nostril Stenosis
Nostril stenosis does occur with some frequency on the repaired side (Fig. 8.5). This complication can obscure breathing and impair the normal toileting of the nasal vault and sinuses. A constricted nostril is one of the more difficult secondary deformities to treat. A common strategy is to avoid the complication by leaving the nostril slightly larger than that of the noncleft side at the time of the primary surgery. By the time the wound contracts, the nostrils will become more symmetric. If they do not, it is much easier to reduce a nostril secondarily than to enlarge one. There is rarely a deficiency of tissue, and it is usually the result of over-resection of normal tissue. Additionally, intranasal incisions can contribute to scar contracture. Some have suggested the use of postoperative stents or nasal conformer to combat stenosis. These devices must be used for a prolonged period of time for this purpose and can become somewhat laborious for parents. While most would advocate surgical release with or without grafting and some form of nostril retainer, some have recommended serial dilation with custom stents or secondary Z-plasty procedures.25,26,27
Fig. 8.5. Four-year-old boy with right unilateral cleft lip and palate. Note the mild to moderate right nostril stenosis.

Nasal Asymmetry
Nasal asymmetry can be a challenge in the cleft lip and palate patient and is unique to the initial severity and morphology of the cleft (Fig. 8.6). Primary rhinoplasty can be safe and does not result in growth disturbance. This has been significant in the evolution of the cleft repair as the lip and nose are too intimately related to be considered separately in the malformation. In the initial lip and nasal construction, surgeons must do their best to achieve symmetry in the face of an absent or hypoplastic maxillary bony platform. The lack of support for the nasal base can make absolute symmetry difficult to accomplish, though some techniques offer better solutions to this problem than do others. Many techniques have been able to minimize the depressed ala and nasal sill in the initial repair, and with limited alar, nasal tip, and septal work, excellent results can be obtained. If one has to achieve symmetry in any component of the nose at the primary surgery, it is the author’s opinion that this should be the nostril sill, primarily from the standpoint of its vertical position, bulk and shape. This area can be difficult to deal with in revisions, especially if it has not been well cared for in the initial procedure. A common mistake is the use of an overly extensive perialar incision and a repair in which the ala and sill are somewhat left behind laterally or deep in the bony defect, relative to the cleft-side lip element mobilization and advancement. Frequently, insufficient attention is given to the mobilization and repositioning of the perinasal muscles to their proper insertion on the maxilla. Often, the muscles in the lateral lip element are treated as one unit and little attention is given to separating and repositioning specific anatomic components. Tip symmetry can be addressed later if need be, though much of this is best addressed at the primary surgery if possible. Once again, nostril conformers can be used to assist in the healing and redraping of the primary rhinoplasty but should not be solely relied upon to achieve nasal symmetry.
Fig. 8.6. Five-year-old girl with left-sided unilateral cleft lip and palate. Note the nasal asymmetry and smaller nostril on the cleft side. There is also a small amount of hyperplastic tissue/scar along the vermilion. These issues are independent and can be addressed separately when age appropriate according to growth.

Facial Growth
It has long been debated whether the lip or the palate repair causes the most harm to the growth potential of the maxilla. While there appear to be compelling data that the lip repair might very well be involved, the debate is far from over.28 Studies implicating gingivoperiosteoplasty and certain forms of presurgical orthopedics have their following as well.29 Additionally, the timing and the technique of primary palate repair likely have an impact.29,30 To further muddy the waters, both subperiosteal and supraperiosteal dissection techniques have been advocated in lip repair. Both techniques have had their passionate supporters and detractors, with neither technique having been shown to out- or underperform the other. Approximately 25% or more of adolescents with cleft lips and palates will suffer from the additional stigmata of maxillary hypoplasia, despite the timing of lip/palate repair or the techniques used.1 This leaves the surgeon with the additional task of restoring the skeletal foundation to a more normal anatomic position at some later date. This is traditionally performed with a Le Fort I osteotomy, either as a single stage procedure or utilizing distraction techniques with various devices. Both techniques have been shown to work well in capable hands and require the assistance of a knowledgeable orthodontist. These techniques are fraught with orthodontic and dental challenges, given the frequent absence of teeth and sometimes deficient bone in the cleft area. Occasionally, the maxillary-alveolar cleft must be grafted or regrafted in conjunction with the orthognathic surgery. Iliac crest grafts are frequently used for added stability in the orthognathic procedures, particularly when the maxilla is deficient both horizontally and vertically.
COMPLICATIONS IN PALATOPLASTY PROCEDURES
To clearly understand complications of palate repair, the cleft surgeon must understand the details of current outcome data regarding cleft palate repair. Velopharyngeal insufficiency (VPI) is a debilitating and unfortunately predictable consequence of a certain percentage of patients who undergo palatoplasty. There are also other complications seen with palatoplasty procedures related to technical aspects of the procedure or particular predispositions with some patients (e.g., airway problems in Pierre Robin sequence). This section discusses some of the more common complications and presents the current data regarding functional outcomes of palatoplasty, particularly as they relate to speech.
Palatoplasty Procedures and Outcome Differences
Le Monnier, a French dentist, reported the first successful cleft palate repair in Paris in 1766.31,32 Since that time, many surgical techniques for cleft palate closure have been described. There is still debate over which technique produces superior results. A lack of clinical data from prospective trials forces clinical decisions to be made from retrospective studies, cohort studies, and surgeons’ experience. Due to the inherent bias and uncontrolled nature associated with this level of evidence, clinicians need to be aware of the shortcomings and incorporate the information appropriately into practice. The primary objective of soft palate closure is the development of normalized speech.1,33 Outcome measures for palate closure should also include maxillary growth, facial profile, dental occlusion, and presence of a fistula.1,34,35
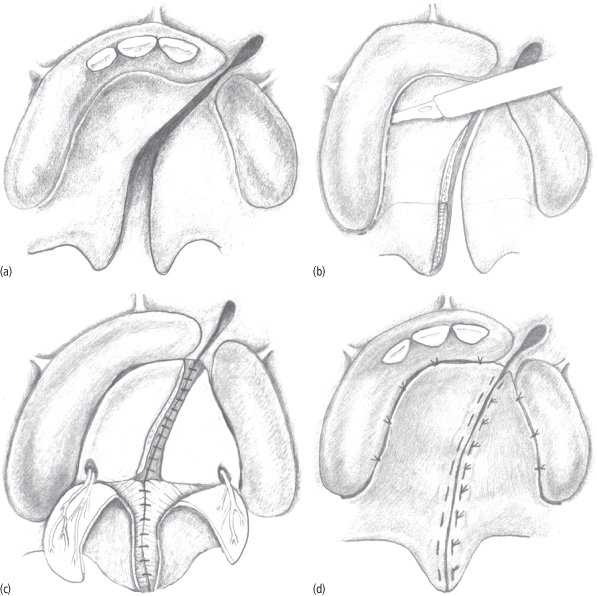
A number of procedures exist for palatoplasty, and their outcome results are complex to evaluate and study with any precision. Bernard von Langenbeck described a palatoplasty technique in 1861, which is the oldest such procedure still in use today. The von Langenbeck palatoplasty involves bipedicled mucoperiosteal flaps with medial repositioning of nasal and oral side mucosa for closure. The technique leaves minimal hard palate exposed but does not lengthen the velum and can impair access for repair of the nasal lining and velar musculature. Subsequently, multiple palate repair techniques incorporated a pushback component designed to lengthen the palate and decrease the incidence of velopharyngeal insufficiency.36 These include variations of the V–Y pushback described separately by Veau, Wardill, and Kilner in 1937.37–39 Mucoperiosteal flaps are raised based on the greater palatine vasculature then retropositioned via a V–Y technique, resulting in lengthening of the velum at the expense of denuded anterior hard palate. Poor growth outcomes and anterior fistula formation has limited the use of this technique. The Bardach two-flap palatoplasty was described in 1967 and further refined with excellent anatomical and functional results.40,41 In the Bardach repair, two mucoperiosteal flaps based on the greater palatine vessels are raised, as the flaps are not pedicled anteriorly (Fig. 8.7). The technique also limits hard palate bone exposure as the flaps are rotated downward at the expense of palatal depth. These cleft palate surgical procedures are now collectively termed the “two-flap palatoplasties.”
Fig. 8.7. (a) Unilateral cleft of the primary and secondary palates is shown with the typical involvement from the anterior vestibule to the uvula. (b) The Bardach palatoplasty technique requires two large, full-thickness mucoperiosteal flaps to be elevated from each palate shelf. The anterior portion (anterior to the incisive foramen) of the cleft is not reconstructed until the mixed dentition stage. (c) A layered closure is performed in the Bardach palatoplasty by reapproximating the nasal mucosa. The muscle bellies of the levator palatini are elevated off their abnormal insertions on the posterior palate. They are then reapproximated in the midline to create a dynamic functional sling for speech purposes. (d) Once the nasal mucosa and musculature of the soft palate are approximated, the oral mucosa is closed in the midline. The lateral releasing incisions are quite easily closed primarily because of the length gained from the depth of the palate. In rare cases, in very wide clefts a portion of the lateral incisions may remain open and granulate by secondary intention.
(From Fig. 35-12 A–D: Fonseca RJ, ed. 2009. Oral and Maxillofacial Surgery, Vol. III. St. Louis: Saunders Elsevier, p. 729.)
In 1978 Leonard Furlow introduced a novel technique of repairing palatal clefts using double-opposing Z-plasties of the oral and nasal layers with anatomic orientation of the soft palate musculature (Fig. 8.8) Furlow has reported superior speech results using this procedure as compared with his experience with the two-flap palatoplasty.42,43 Many centers adopted the Furlow palatoplasty and have reported better outcomes.44–47 These reports consist mostly of self-reported experiences from a single center or surgeon and limited retrospective comparisons of techniques. They do not provide powerful data sufficient enough to make definitive statements regarding their superiority. Currently, only some level II and mostly level III evidence is currently available to help us make clinical decisions regarding repair techniques. Successful cleft palate repair requires adequate muscular reconstruction of the velum to create a dynamic and functional soft palate. The two-flap and Furlow palatoplasties both reconstruct the velar musculature (i.e., the levator veli palatine or palatopharyngeus) into a dynamic sling but do so in different manners.
Fig. 8.8. (a) Complete cleft of the secondary palate (both hard and soft) is shown from the incisive foramen to the uvula. (b) The Furlow double-opposing Z-plasty technique requires that separate Z-plasty flaps be developed on the oral and then nasal side. Note the cutbacks creating the nasal side flaps, highlighted in blue. (c) The flaps are then transposed to theoretically lengthen the soft palate. A nasal side closure is completed in the standard fashion anterior to the junction of the hard and soft palate. In general, this junction is the highest area of tension and can be difficult to close. This contributes to the higher fistula rate in this type of repair at this location. (d) The oral side flaps are then transposed and closed in a similar fashion, completing the palate closure.
(From Fig. 35-13: Fonseca 2009, Vol. III, p. 730.)
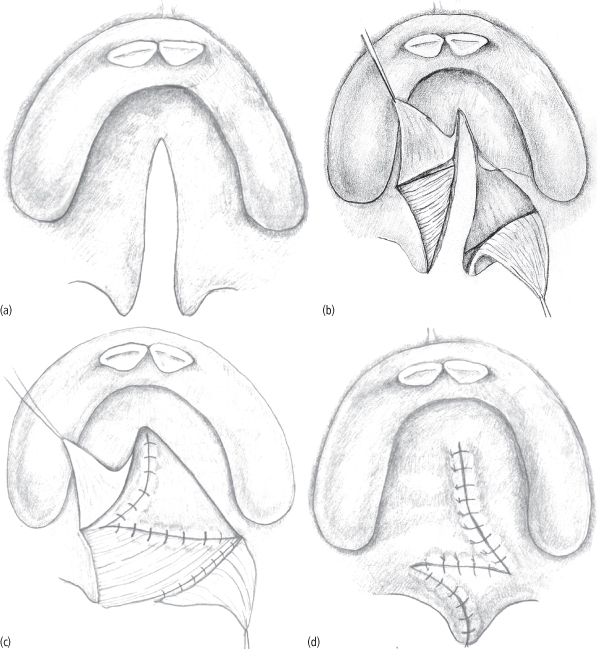
One criticism of the Furlow technique relates to the higher fistula rates found in many studies when compared to two-flap techniques. Fistula rates reported in the literature are infamous for reporting bias, differing definitions and classifications of fistulas, and faulty study design. This makes meaningful comparisons nearly impossible, and a number of authors have recommended strategies to decrease fistula rates—particularly with the Furlow technique. The placement of acellular dermis between the oral and nasal flaps is recommended by some, and this has shown a significant reduction in fistula rates comparable to two-flap closures.48,49,50 Some recent reviews of fistula formation after two-flap palatoplasty revealed low rates of 3%.51,52 Helling reported a fistula rate of 3.2% when acellular dermis was used in conjunction with the Furlow technique.50
The speech outcome data for Furlow palatoplasty technique compared against the two-flap techniques has generally been favorable. Multiple authors have reported their own improved speech results and low rates of VPI with Furlow versus various modifications of two-flap palatoplasties.46,53–56 These studies consist of single surgeon/center experience prior to and after adoption of the Furlow technique. While compelling, these data represent level III evidence and have not had the statistical power to convincingly provide a wave of change in the surgical community. Despite flaws in the study designs, the reduction in reported rates of VPI is impressive. Randall reported a decrease in VPI from 68% to 25% after instituting the Furlow technique.57 Williams reports a VPI rate of 13% with the Furlow and 25% with von Langenbeck palatoplasties.55 A small number of uncontrolled studies have reported no significant difference in speech or VPI outcomes between the Furlow and Veau-Wardill-Kilner or von Langenbeck techniques.58,59 A study conducted at the University of Florida and Sao Paolo, Brazil, sought to compare outcomes of the Furlow and von Langenbeck palatoplasties. The results are unpublished but preliminary findings presented in abstract form have suggested only minor differences in outcome with the exceptions that the Furlow group has a higher fistula rate and the von Langenbeck procedure with increased measurements of hypernasality as only one element of a comprehensive speech evaluation.60 The available published data have been either weak level II or level III evidence, and as such they are difficult to utilize when deciding between repair techniques. As a result, the data at this time are not convincing enough to advocate the Furlow over the two-flap palatoplasties. As evidenced by the available literature, good results can be obtained with either two-flap or double-opposing Z-plasty techniques.
Perioperative Complications of Cleft Palate Repair
Perioperative complications associated with palatoplasty for cleft palate are generally rare. Experienced surgeons routinely obtain superior results with a variety of standardized techniques. Complications associated with the surgical procedure in the perioperative period include bleeding, airway compromise, infection, and vascular compromise of the flaps. Fistulas may be seen early after repair and are discussed in a separate section below.
Bleeding occurs with the palatoplasty procedure due to the rich vascular supply of the local soft tissue and bone. Since most patients undergo palatoplasty between the ages of 9 and 18 months, their blood volumes are fairly small. Diligent control of bleeding is important to limit the blood loss during the procedure. While it is rare to require transfusion after palatoplasty, those children who have palatoplasties at a young age and that involve the hard and soft palate will have significantly higher transfusion requirements. This requires careful attention with volume status assessments, and occasionally an evaluation of the patient’s red blood cell mass intraoperatively and/or postoperatively. Bipolar electrocautery is recommended to avoid conduction of the current down an axial flap and to allow for precise coagulation. Preservation of the greater palatine vasculature is important to avoid vascular compromise of the flaps. Reexploration is quite rare at less than 1%.61
Airway compromise can occur at multiple time points associated with the procedure. While many patients can be visualized during intubation with a simple direct laryngoscopy, others require more specialized techniques. Careful planning should be a part of the preoperative process, including the readiness of specialized airway equipment for the difficult airway. Intraoperative loss of the airway is uncommon but can be related to positioning of the endotracheal tube, tape failure, displacement of the mouth gag/retractor, or placement and removal of an oral–gastric suction tube at the end of the procedure. Postoperative airway compromise may occur with extended periods of retractor activation. The tongu/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


