6
Distraction Osteogenesis
INTRODUCTION
Distraction osteogenesis (DO) was first described by Codivilla in 1905 for the treatment of a short femur.1 It was later popularized by Ilizarov, an orthopedic surgeon, who formulated and applied the principles of DO for limb lengthening to a large number of patients. As a result of his pioneering work, Ilizarov is recognized as the “father of distraction osteogenesis.”2 McCarthy was the first to use the technique of distraction for treatment of craniofacial deformities.3 Distraction osteogenesis is now part of the standard surgical armamentarium for skeletal expansion in the craniomaxillofacial region.4
Distraction osteogenesis offers many advantages over traditional techniques, including gradual lengthening of the soft tissue envelope5 and the potential elimination of the need for bone grafting.6 However, as with any technique, limitations and disadvantages exist. Some of the shortcomings include difficulties in establishing the correct distraction vector, need for patient cooperation, and prolonged treatment time. As with most procedures, complications may be avoided by careful patient selection and proper surgical planning and technique.6 Complications can be divided into three phases: preoperative (planning), intraoperative, and postoperative.7,8
In this chapter, complications associated with distraction will be described. This chapter is based on two other chapters of complications of DO.7,8
PREOPERATIVE PLANNING PHASE
The best strategy is to prevent complications by careful preoperative planning, which includes appropriate patient selection, accurate assessment of the anatomy and planning of the vector of distraction, and osteotomy location and placement of the distraction device.7,8
Patient Selection
Distraction osteogenesisis a treatment that demands significant commitment from the patient, family, and surgeon. Whether distraction devices are intraoral or extraoral, pin borne or bone borne, they can be bulky and complicated to use.7,8
Primrose et al. reported a series of pediatric patients who underwent distraction with either an intraoral or extraoral device.9 Patients who had extraoral devices reported sleep disturbances because of the bulkiness of the distractor. They also complained of limited ability to engage in recreational activities. Older patients who had extraoral devices felt “abnormal.” Patients with intraoral devices reported speech, eating, and oral hygiene difficulties but felt the devices had less of an effect on social activities.9 Modfid et al. reported that 4.7% of all DO patients displayed poor compliance regardless of the type of device.6 This is a clinical observation, which multiple authors have reported.6–9
The preoperative interview with the family should include a discussion of the impact that this technique will have on the patient’s social life and the possible disruption of participating in educational and recreational activities. The diet should be reviewed with the patient in advance because it will be limited to soft or blenderized foods throughout the distraction and fixation periods. The patient and family should be familiarized with the appliance and verify that they will be able to activate it as needed. The use of educational tools including models and dolls with distraction devices can be helpful (Fig. 6.1). Additionally, the patient and family should be made aware that a number of postoperative visits are necessary with DO (usually more than with conventional procedures).7,8 As with all surgical procedures, alternative treatments, risks and benefits of DO (including possible reoperation) need to be clearly outlined.
Fig. 6.1. Dolls and skull models with distraction devices used for demonstration.

Distraction Vector Planning
An accurate distraction vector is necessary to obtain the desired final position of the distracted segment. Mofid et al. reported an incorrect distraction vector in 8.8% of patients who had a single vector distractor and in 7.2% who had a multivector distractor.6 The wrong vector of distraction can cause malocclusion and/or facial asymmetry, and may require additional procedures for correction (Fig. 6.2).
Fig. 6.2. (a) Patient with left predominant hemifacial microsomia; (b) incorrect vector of distraction caused cross bite on the right side and (c) did not create the desired open bite on the left side.
(All images printed with permission from PMPH-USA.)

In order to accurately obtain the correct distraction vector across the osteotomy, development of the appropriate preoperative treatment plan is required and correct transfer of this information to the operating room is necessary. Preoperative treatment preparation is based on clinical and radiographic examination [lateral and anteroposterior cephalograms, orthopantograms, and computer tomography (CT) with three-dimensional (3D) reconstruction].7,8 Treatment planning software can assist with developing the movement of the distractor, analyzing interferences, and fabricating the accurate device or choosing the correct distractor from a set of existing devices.7,8,10,11
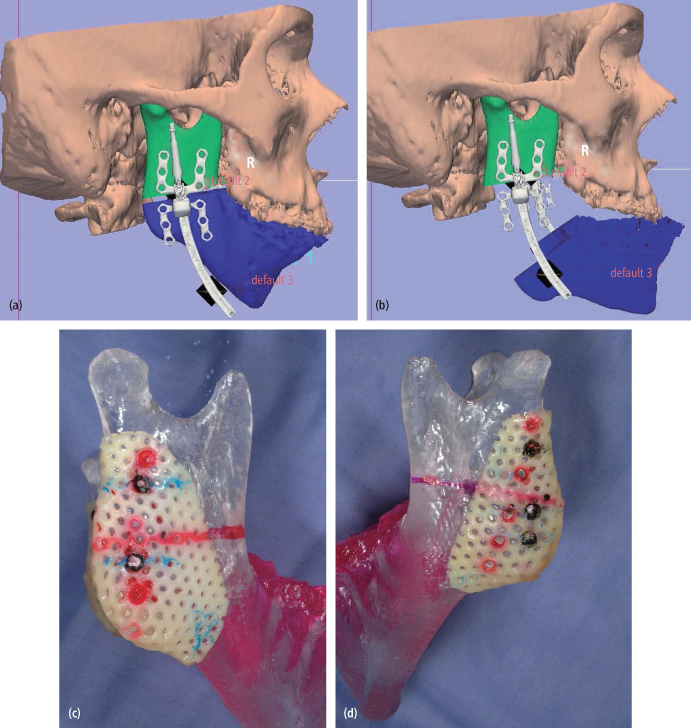
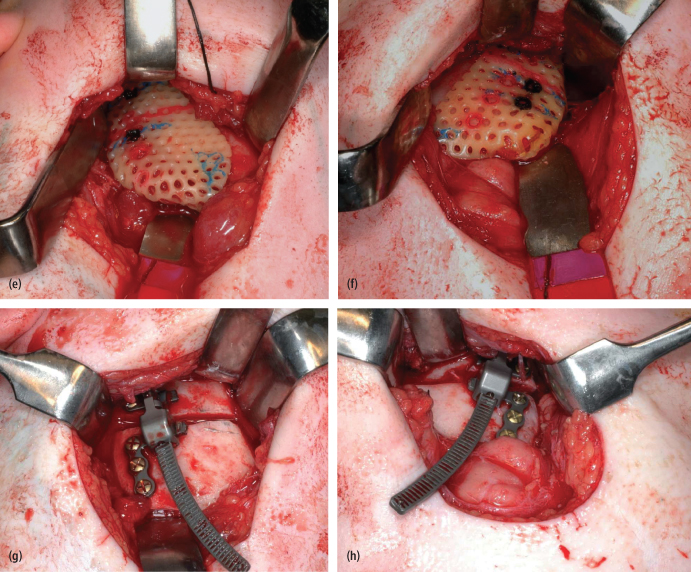
A surgical guide can help transfer the preoperative plan to the operating room.11 After establishing a treatment plan that includes the osteotomy and distractor position, this information can then be entered into a virtual computer environment that allows envisioning the surgical outcome based on the treatment plan. This treatment plan is then transformed to stereolithographic models, and surgical guides are made according to these models (Fig. 6.3). This preparation minimizes the risk of an inaccurate direction of distraction.8 Intraoperative surgical navigation is a developing field and can be a useful tool to use to correctly perform osteotomies and position devices.
Fig. 6.3. Surgical plan using computer software (Ostoplan, 3D Slicer). The location of osteotomy and vector of distraction can be determined. (a), (b) The surgical guide can be made using stereolytic model. (c), (d) The location of osteotomy and position of the distractor can be marked on the surgical guide. (e), (f) Accurate osteotomies and (g), (h) correct placement of distractors can be achieved intraoperatively using surgical guides.
(All images printed with permission from PMPH-USA.)
INTRAOPERATIVE PHASE
Neurologic and Dental Injury
Distraction osteogenesis requires a complete osteotomy and placement of the appliance that can result in damage to adjacent structures such as teeth and nerves.7,8 Mofid et al. reported a review of 3,278 cases. There were 81 (3.6%) cases of damage to the inferior alveolar nerve, 69 (1.9%) had tooth bud injury, and 12 (0.4%) had facial nerve injury.6 Swennen et al. found tooth damage in 2.3% of cases.12 Most of the damage to adjacent structures can be reduced during the osteotomy by careful analysis of preoperative radiographs and accurate execution of the planned osteotomy. In most cases, the paresthesia of the inferior alveolar nerve is transient; typically, younger patients spontaneously recover sensation more quickly and to a higher degree than older patients.7,8/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


