Technologic Advances in Implant Surgery
Dental Implant Microsurgery—Immediate Placement
The success of dental implants in extraction sites combined with immediate provisionals for newly placed dental implants has brought a convergence in restorative and surgical practice for treatment planning of dental implants. This convergence reaches its summit in the approach to failing teeth in the maxillary esthetic zone. For anatomic reasons, maxillary anterior teeth are at high risk for traumatic injury13,14 (Figure 79-1). Traumatized teeth frequently receive endodontic treatment that may be followed by horizontal or vertical root fracture.1,2,15 Dentistry’s historic answer to tooth loss has been the fixed bridge. Tooth preparation necessary for a fixed bridge often results in significant reduction of tooth structure.22 Inherent esthetic limitations of fixed bridges include loss of gingival papillae and resorption of the buccal alveolar plate. For these reasons, dental implants are a preferred choice for tooth replacement in the maxillary esthetic zone.
Implant Microsurgery
Microsurgery is associated with enhanced soft-tissue procedures and fine suturing. This is part of the scope of implant microsurgery but additional benefits include dental implant drilling precision. The ability to discern minute dimensional differences permits implant osteotomy preparations centered exactly between reference points such as adjacent teeth, adjacent implants, or buccal and lingual ridge anatomy. More profoundly, the microscope allows immediate detection of subtle changes in drill position so appropriate feedback corrections can be applied to the handpiece. Enhanced angular perception is also important. The drill’s angular position can be oriented relative to small landmarks such as the implant platform surface level or the angle of adjacent implant healing caps. This permits optimal parallel positioning and depth of adjacent implants. The implant drill angle can also be accurately oriented to root surface angulation using just 3 to 4 mm of root anatomy exposed between the cementoenamel junction and the osseous crest. These reference points are simply not visible without a microscope. The detection of subtle angulation reference points and changes in drill position permit feedback correction, which is important for osteotomy preparation in extraction sockets. The microscope-enhanced accuracy of osteotomy microsurgery permits socket implant placement in an ideal position followed by an esthetic implant-supported provisional (Figure 79-2). As a flapless procedure, this is accomplished with minimal patient morbidity.22
Microsurgical Tooth Extraction
Tooth extraction has been traumatic for centuries. Conventional tooth extraction may require mucogingival flaps and bone removal, resulting in compromised esthetics. Employing a microscope with minimally invasive principles reduces trauma and results in predictable esthetic outcomes.6 Instrument selection influences the trauma of tooth removal. Periotome luxation or leveraged mechanical extraction employing tapped root anchorage systems can carefully separate a tooth from its surrounding ligament and lift it vertically from the socket. This limits injury to papillae and preserves natural gingival anatomy (Figure 79-3). Subtle nuances in luxation direction can be microscopically detected for root removal in a proper anatomic path of extraction. Increased visibility under the microscope permits most extractions without mucogingival flaps. Greater visibility also permits atraumatic sectioning of ankylosed roots to leave alveolar bone and soft tissue uninjured. Apical granulomatous lesions can be completely debrided with full visibility. Such minimally invasive microsurgical techniques translate into reduced patient morbidity with enhanced healing.
Implant Drilling in the Extraction Site
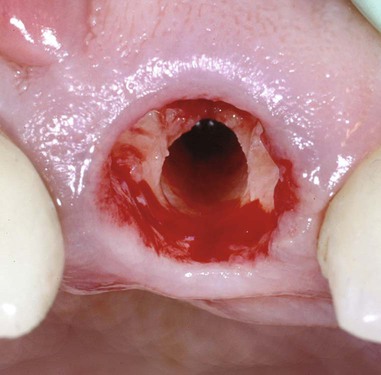
Microsurgical implant drilling in the extraction socket is unique. Under the microscope, a socket appears as large as a room with its apex and walls clearly visible. A different set of skills is required for socket drilling. For placement of maxillary anterior implants, the most favorable bone lies to the palatal (Figure 79-4). Drilling therefore must be done at an angle to the palatal socket wall. Twist drills innately track toward the direction of less dense bone and into the open socket. Drilling sockets under a microscope utilizes visual feedback to constantly redirect the drill to the correct position and angulation. This avoids the common mistake of an implant being placed too far toward the buccal. With the magnification and lighting a microscope provides, implants can be placed in the palatal socket wall with good initial stability and ideal esthetic position. Microscope-enhanced dimensional and angular perceptions allow adjustments to correct drilling speed. Too little or too much drill pressure or excessive drill speed causes frictional heat. This adversely affects implant osteointegration. Detecting micromovement of the advancing drill ensures that proper pressure and rotational speed are applied to varying bone densities encountered in the socket. The angular velocity at the cutting edge of a 4-mm drill is several times faster than the velocity at the cutting edge of a 2-mm drill. For this reason, pressure and rotation of larger diameter drills must be decreased to compensate for their faster cutting speed. Enhanced visual feedback for speed and pressure correction is accomplished through directly viewing the advancing drill under the microscope.
Buccal Gingival Grafting
Recession on the buccal gingival margin around anterior implants placed in extraction sockets has been well documented.11,17 Multiple factors, such as the periodontal biotype, presence or absence of the buccal cortical plate, surgical trauma, implant position, and the emergence profile of both the provisional and final restorations, are associated with such recession.9,12,16,18–20 A subepithelial connective tissue graft is therefore harvested from the palate and transferred into a split-thickness envelope incision on the buccal of the implant. A connective tissue graft is done to maintain or augment gingival height and thickness that may have been lost as the result of injury (Figure 79-5). Even gingiva/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses