Esthetic Management of Difficult Cases (Minimally Invasive Approach)
In recent years, implant dentistry has been increasingly influenced by esthetic considerations. In addition to successful osseointegration, harmonious soft and hard tissues must surround the implant restorations so that they look natural and healthy. A major challenge in implant dentistry is that, in many instances, dental implants need to be placed in an esthetic zone in which there is extensive alveolar bone deficiency from tooth loss, dentoalveolar infection, or other pathology (Figure 78-1, A to C). Gingival morphology follows the shape of the underlying bone, and it is difficult to build esthetically acceptable gingiva in areas with deficient supporting bone. Furthermore, using conventional surgical approaches to accomplish the goal in a patient-friendly manner with minimal trauma and clinical predictability is an extremely demanding task.
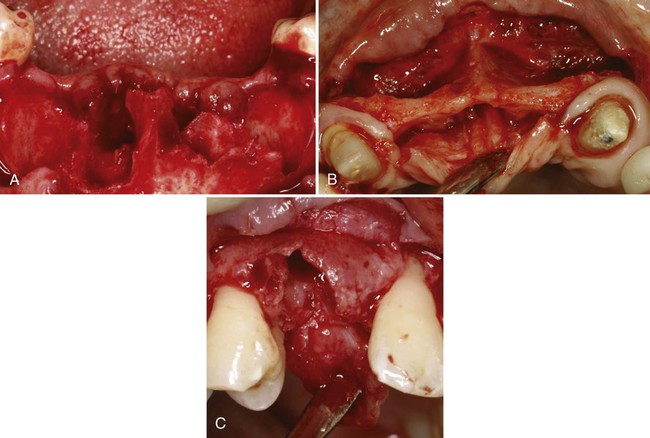
A, Anterior mandibular site showing extensive bone loss following extraction of hopelessly infected mandibular incisors. B, Extremely narrow (labial-palatal) ridge width in the anterior maxilla that was missing centrals and laterals for many years. C, Moderate bone loss associated with the extraction socket of a maxillary cuspid.
Treatment planning in a complex implant case today is often confusing because there are many different surgical and restorative approaches to solve the same problem. Many times these procedures seem to conflict. When considering the surgical placement of implants, clinicians must consider the approach (conventional two-stage approach versus a one-stage approach) and the timing of implant placement (immediate versus delayed or staged placement). For bone augmentation procedures, there is the more conventional approach of augmenting the ridge first and placing the implant(s) after healing, or the simultaneous implant placement with bone augmentation approach in which bone grafting is done at same time as implant placement. All of these approaches can provide a successful outcome if patient selection is appropriate and techniques are performed properly.9,22,24,32 However, depending on the situation, some of these techniques are more advantageous than others in achieving esthetic results with better predictably and less patient discomfort.
Minimally invasive surgery in implant dentistry implies a surgical approach that minimizes the extent and number of surgeries while providing esthetics, predictability, and longevity with minimal surgical morbidity and discomfort to patients. The surgical approach most often required to achieve these goals for anterior implant therapy involves immediate implant placement, one-stage surgical approach, with or without flap, and simultaneous bone grafting. Furthermore, these surgical techniques need to be guided by a consistent surgical strategy that provides predictable esthetic results in implant dentistry. A minimally invasive approach to implant therapy in posterior sextants in which esthetics is not a major concern can be predictably achieved with the use of short wide implants.2,15,16,27
Surgical Strategy for Predictable Esthetics
1. Determine the level of surgical esthetic goal to be achieved.
2. Visualize the final outcome.
3. Preserve existing tissues important for esthetics.
4. Always overbuild bone and soft tissue in augmentation surgeries.
Determine the Level of Surgical Esthetic Goal
The surgical esthetic goal can be ideal, acceptable, or compromised. An ideal surgical esthetic goal (Figure 78-2) implies an ideal, complete surgical reproduction of periimplant tissue around an implant restoration. An acceptable surgical esthetic goal (Figure 78-3) implies that the esthetics of the final implant restoration and the periimplant tissue is not ideal, but both the patient and the clinician accept it. Also, the hygiene and the long-term health of the restoration is not compromised. A compromised surgical esthetic goal (Figure 78-4) implies that the esthetic, hygiene, and long-term health of the implant is far below what is acceptable in today’s clinical standard.

Clinical photograph of an implant-supported crown replacing maxillary right cuspid in a 20-year-old female with a high smile line. Soft tissues are full and contours appear natural.

Clinical photograph of implant-supported crowns replacing multiple missing maxillary anterior teeth in a 63-year-old female with a low smile line. Soft tissues are nearly full and contours appear fairly normal but not ideal.

Severe ridge deficiency resulted in long implant-supported fixed restoration and difficult oral hygiene access. Notice the pink porcelain used to mask the increased length of the crowns. Soft tissues are obviously compromised and completely lack any semblance of normal.
Visualize the Final Outcome
Once the level of the esthetic goal is determined, the next step is to visualize the final outcome. Determination of the vertical position of the implant, quantity and quality of the soft and hard tissue augmentation needed, components of the alveolar tissue that need to be preserved in surgery, and what surgical approach is most appropriate for the patient cannot be accomplished without first visualizing the final esthetics of the implant restoration(s) involved. In simple cases, the visualization can be done mentally or with the aid of computer graphic simulation. In more complex cases, a diagnostic wax-up may be necessary.38
Always Overbuild Bone and Soft Tissue in Augmentation Surgeries
Many studies have shown that there is rapid labial and vertical bone loss after extractions,3,26,30 and immediate implant placement does not stop the resorption process.10,12,35 Furthermore, it has been demonstrated that soft and hard tissues grafted in augmentation procedures to enhance esthetics undergo extensive shrinkage within 3 to 6 months.1,36 Therefore the deficient ridge needs to be overbuilt by approximately 30% to 40% at the time of surgery to be esthetically sufficient after the expected primary and secondary tissue shrinkage.
Immediate Implant Placement for Predictability and Esthetics
Immediate implant placement in a one-stage approach, in which a healing abutment or provisional restoration is attached to the implant and remains exposed, provides more predictable preservation of the interproximal periimplant gingival tissue with less patient discomfort and treatment time.21,22 This approach to implant placement is the foundation of a minimally invasive approach to esthetic implant dentistry. However, as with any surgical technique, it takes learning and practice to perform it properly. The criteria and techniques for proper immediate implant placement have previously been established and reported with successful long-term outcomes.18,32
One of the more difficult aspects of immediate implant placement is positioning the implant with sufficient primary stability in an extraction socket, often without elevating a flap. The alveolar architecture in relation to the angle of the implant to be inserted; the presence or absence of a bone concavity apical to the extracted tooth; the amount of existing bone apical and palatal to the extraction socket, which can provide primary stability for the immediate implant; and the quality of the bone and soft tissues of the ridge should all be thoroughly evaluated clinically and radiographically before surgery.18,32 Many clinicians perform successful immediate implant placement without the aid of a three-dimensional scans (e.g., computed tomography [CT] or cone-beam CT [CBCT]). However, if the tooth involved is long and large or if there is an alveolar concavity or other anatomic variations, the use of a CT/CBCT scan is advised.
A major disadvantage of placing implants immediately in the changing alveolar bone of an extraction socket is that it may result in progressive recession of the gingival labial margin over the implant restoration.4,17 Therefore, when placing an immediate implant with one-stage surgical approach in an esthetic zone, a prudent strategy would be to improve the quality and quantity of labial gingival tissue, which seems to be vital for the stability of the labial gingival margin involving immediate implants.19,31 One of the most effective ways to keep the implanted socket from collapsing and improve the labial gingival biotype is to simultaneously fill the labial socket void with particulate bone and augment the labial gingival tissue with soft tissue.3,23,26,30,32
An effective bone and gingival tissue augmentation technique used with flapless immediate implant placement in a one-stage approach is the bone and crescent-shaped free gingival grafting technique.18 In this technique, the space between the inner surface of the labial bony wall and the labial surface of the implant is filled with slow-resorbing mineralized, freeze-dried particulate bone allograft or particulate xenograft to help preserve the horizontal dimension of the ridge (Figure 78-5, A). Then, a crescent-shaped soft-tissue graft is harvested from the ipsilateral palate (Figure 78-5, B) and transplanted into the labial recipient site coronal to the particulate bone graft (Figure 78-5, C). To provide/maintain the blood supply to the donor tissue, it is important that the outer surface of the crescent graft fits with an intimate contact with the bleeding lamina propria of the labial gingiva. Proper suturing ensures good proximity and prevents the graft from being displaced coronally out of the recipient site (Figure 78-5, D).
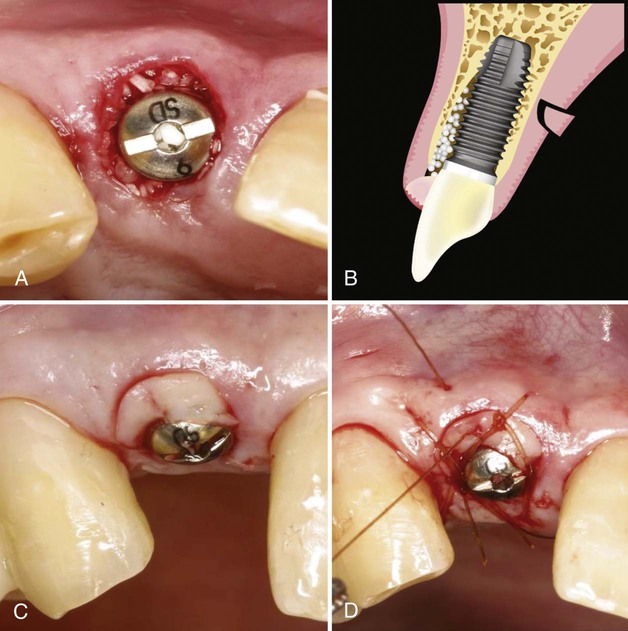
The advantage of this approach to gingival augmentation is simplicity and minimal surgical morbidity. In addition to providing a sealed protection for the bone graft, it prevents resorption of the sensitive labial crestal bone. Preparation of the recipient site involves no surgical manipulation other than deepithelialization as described. Gingival walls are completely intact with a full blood supply. The donor site wound is small (approximately 3 mm depth × 3 mm height at the widest point) with intact epithelium around the wound, which epithelializes within a week and causes minimal discomfort for the patient. Because each donor tissue graft is small, multiple grafts can be harvested from a single palate, so that multiple immediate implants can be augmented at same time. Furthermore, this gingival augmentation technique frequently improves an unfavorable initial gingival margin because the grafted gingival margin is always coronal to the existing gingival margin. This minimizes a need for other time-consuming techniques, such as orthodontic extrusion, or a delayed approach to implant placement when the initial gingival margin is not esthetic or ideal, as recommended by many authors.5,33
Surgical Management of Difficult Cases (Minimally Invasive Approach)
The cause of the failure to satisfy the esthetic needs of a patient frequently starts with an inadequate examination of the soft and hard tissues surrounding the surgical site and the natural dentition. This can result in an incorrect diagnosis, which leads to incorrect treatment plan. The wrong treatment plan combined with selection of inappropriate surgical approaches or techniques can result in a disastrous esthetic outcome and unnecessary patient suffering. The first two case presentations describe the examination and thought processes involved in determining the diagnosis and treatment planning of complex anterior cases with extensive alveolar bone loss. The proper application of the surgical strategies and the minimally invasive techniques, previously described, are illustrated. The final case presentation illustrates the minimally invasive approach to posterior implant therapy with the use of short wide implants, in which esthetics is not the major concern.2,15,16,27
Case Presentation 1
Examination and Diagnosis.
The maxillary incisors exhibit moderate-to-severe periodontitis with 4- to 7-mm periodontal probing depths. They exhibit severe (2+) mobility with fremitus. The periodontal and restorative prognosis of these teeth is poor. She has an excessive overbite with evidence of moderate mandibular incisor wear, indicating possible parafunctional habits. Her incisors are slightly elongated, but the dentogingival symmetry is acceptable (Figure 78-6, A). The shape of the incisors is slightly triangular with sufficient interdental papilla volume and height. Interproximal gingival tissue is not swollen or edematous. Her gingival biotype appears to be on the thin side with slight marginal inflammation, and the position of the labial gingival margins is already high (i.e., maximal apical position). Any further recession will be unaesthetic.


Radiographic evaluation demonstrates moderate-to-severe vertical and horizontal periodontal bone loss. The osseous crest position, in relation to the gingival margins, appears too apical to provide adequate gingival support (see Figure 78-6, B). The restorative and periodontal status of the canines is healthy.
Treatment Options.
Even if this patient can tolerate the temporary removable partial denture, which she said she could not, this option poses a considerable esthetic challenge. The ridge surrounding the extraction sockets will rapidly lose vertical and horizontal dimensional soon after the extractions.3 The loss of vertical height in the interproximal gingival areas creates an esthetic problem that is very difficult to correct. It often requires multiple surgeries that have a high incidence of surgical morbidity and rarely achieves the desired ideal esthetic result. This is especially true in a case like this in which there is extensive periodontal vertical and horizontal bone loss. The anticipated vertical ridge collapse after the extraction is substantial, even with bone grafting of the extraction sockets. More importantly, the need for multiple surgeries to achieve “acceptable” esthetic results for this patient may be too traumatic for her.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


