Vesiculobullous Disorders
•. Herpes Simplex Virus (HSV) infections
•. Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis (Lyell’s Syndrome)
Predominantly Vesicular Lesions
Herpes Viruses
When an individual comes in contact with the virus, primary infection is seen. Subsequently these viruses establish latency in the host. The site of latency for each form of herpes virus is different (Table 2).
Table 2
| Name of virus | Site of latency |
| HSV 1 & 2, VZV | Sensory nerve ganglia |
| CMV | Lymphocytes, salivary gland tissue (rarely) |
| EBV | B lymphocytes and salivary gland tissue |
| HHV-6, HHV-7 | CD4 lymphocytes |
| HHV-8 | Still unknown but believed to be associated with B lymphocytes circulating in hematopoietic system |
Herpes Simplex Virus (HSV) Infections
Clinical features
Primary HSV infection
Only 1% of the population in USA exhibit all signs and symptoms of primary infection. It usually affects young children and adolescents, and occasionally young adults. The primary HSV infection seldom occurs in the first 6 months of life as the infant is protected by the maternal antibodies that are still circulating in the newborn.
Herpetic Whitlow and Herpes Gladiatorum
Investigations
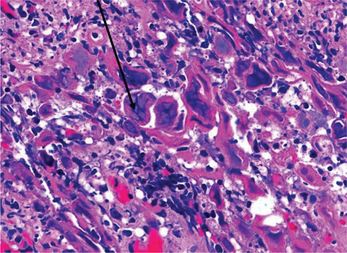
On biopsy the microscopic features include an ulcerated epithelium with large keratinocytes showing glassy giant marginated nuclei (Tzanck cells) (Figures 1 and 2).
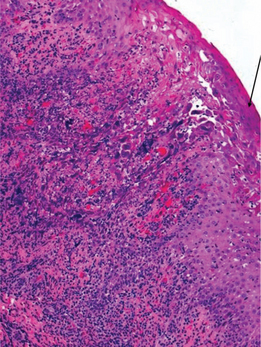
Figure 1 Photomicrograph of herpetic ulcer. H&E stain (10x). Arrow points to acantholytic cells and Tzanck cells. Courtesy: Dr Nagamani Narayana, Nebraska, USA
Recurrent Herpes Infections
Herpetic Labialis
This is the most common secondary herpetic lesion, usually following exposure to UV light or extreme cold. Groups of vesicles appear at the vermillion border, and rupture may result in crusty lesions. The lesions are tingly and painful, normally healing within 2 weeks. The lesions are highly contagious at the weeping stage.
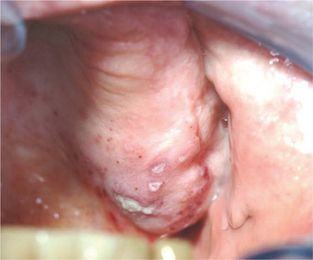
Intraoral herpetic lesions are evident as clusters of vesicles (Figure 3). These vesicles rupture, leaving ulcerations on bound mucosa, usually within 3 days of recent dental treatment. These are also present with prodromal symptoms such as paresthesia, swelling, burning and tingling.

Figure 3 Clusters of vesicles in a 26-year-old female, characteristic of herpes labialis. Courtesy: Dr Nagamani Narayana, Nebraska, USA
Treatment
The aims of managing HSV infections are to inhibit autoinoculation and transmission. The management is targeted at symptomatic relief. Topical and systemic antivirals like acyclovir can be used (Table 3).
Table 3
Treatment regimen for different kinds of HSV infection
| Immunocompetent | Immunosuppressed | |
| Primary herpetic gingivostomatitis—children | Symptomatic—no aspirin or NSAIDs | Acyclovir capsules 200 mg or valacyclovir caplets 500 mg |
| Primary herpetic gingivostomatitis—adult | Symptomatic, aspirin and NSAIDs, magic mouthwash | Acyclovir capsules 200 mg, 5 times daily for 10 days or valacyclovir caplets 500 mg, 2 caplets twice daily for 5 days |
| Recurrent herpetic labialis | Abreva, Denavir 5%, valacyclovir 1,500 mg, single dose or valacyclovir 750 mg, twice daily for 1 day started within 1 hour of onset of prodromal signs | Valacyclovir caplets 500 mg, 4 caplets taken at prodromal symptoms and 4 caplets 12 hours later |
| Recurrent intraoral herpes | Acyclovir 200 mg 5 times a day for 10 days |
Varicella Zoster Infections
Clinical features
Secondary infection (herpes zoster)
Secondary varicella zoster infection occurs in adults with altered immune status or under stress and is unilateral. The main distinguishing feature of VZV is unilateral and involves one of the branches of the trigeminal nerve. Clinically tingling and vesiculation similar to herpes simplex are seen. Clinical appearance of these lesions is very similar to herpes simplex except for the unilateral location (Figures 4 and 5). Patients may complain of mild to severe pain that may exacerbate on the slightest of touch. The dermal lesions usually resolve in about a week forming a scab.
Complications Associated with Herpes Zoster
Herpes zoster is generally unilateral. However in immunocompromised individuals or an associated malignancy, herpes zoster can exhibit a generalized involvement. Other relatively uncommon complications involve encephalitis, peripheral nerve palsies and myelitis.
Hand, Foot and Mouth Disease
Etiology
Enteroviruses are known to cause HFM disease. The enteroviruses that have been implicated are Coxsackie virus serotype A 16, Coxsackie virus serotype A 4 to 7, 9, 10 and Coxsackie virus serotype B 1 to 3 and 5. Asia Pacific region including regions like Singapore, Japan, Indonesia, Malaysia and Taiwan in the 1970s reported severe forms of HFM disease resulting in a widespread epidemic. The cause for this epidemic was Enterovirus-71 A, B, C (EV 71). The EV-71 apart from causing HFM disease can also cause flaccid paralysis, myocarditis, pulmonary hemorrhage, encephalitis and meningitis.
Deshpande et al (2003) isolated a strain of EV-71 from the stool of a child suffering from acute flaccid paralysis following administration of oral polio vaccine. They termed this isolated strain as EV 71 D genotype.
Dermatitis Herpetiformis
Clinical features
Dermatitis herpetiformis usually affects individuals in the 2nd and 3rd decade of life. Dermal lesions are characterized by blisters over an erythematous or urticarial base. The lesions are pruritic.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses