Oral Ulcerative Diseases
Classification Of Oral Ulcers
Classification based on mode of onset and clinical presentation
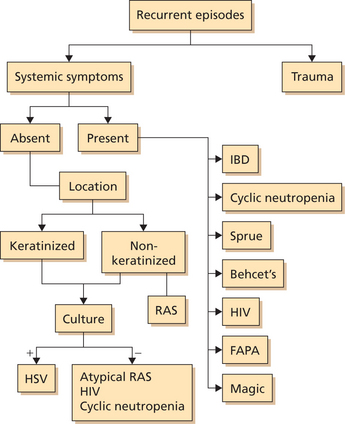
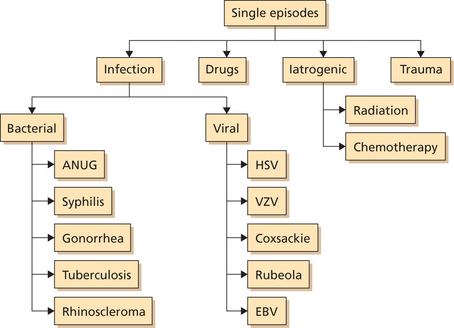
Flowcharts 1 and 2 summarize acute ulcers that are recurring in nature and those that occur as an isolated episode.
Traumatic Ulcers
Types of Trauma
 Mechanical (sharp tooth, overextended denture, orthodontic brackets, toothbrush, ill-fitting dental prosthesis, etc.)
Mechanical (sharp tooth, overextended denture, orthodontic brackets, toothbrush, ill-fitting dental prosthesis, etc.)
 Chemical (aspirin, concentrated clove oil, sodium hypochlorite, hydrogen peroxide, root canal medicaments, chemotherapy, etc.)
Chemical (aspirin, concentrated clove oil, sodium hypochlorite, hydrogen peroxide, root canal medicaments, chemotherapy, etc.)
 Thermal (extremely hot or cold insults such as hot cheese, hot beverages, popsicle) (Figure 1)
Thermal (extremely hot or cold insults such as hot cheese, hot beverages, popsicle) (Figure 1)
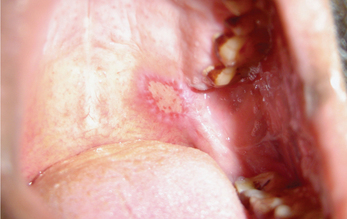
Figure 1 A thermal burn on the hard palate secondary to intake of a hot bread sandwich. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore
 Radiation (used in treatment of head and neck cancer)
Radiation (used in treatment of head and neck cancer)
 Iatrogenic (injuries caused by high speed rotary instruments, cotton rolls, etc.)
Iatrogenic (injuries caused by high speed rotary instruments, cotton rolls, etc.)
Young children are commonly susceptible to electrical and/or thermal burns of the lips and commissure areas. Extensive ulcerations with necrosis may develop. Children in this age group have a tendency to chew their lips immediately after surgical removal of teeth under the influence of local anesthesia.
Clinical features
Ulcerations can occur throughout the oral cavity. Ulcers associated with mechanical trauma are often found on the buccal mucosa, the labial mucosa of the upper and lower lips, and the lateral border of the tongue (Figure 2). The mucobuccal folds, gingiva, and palatal mucosa may also be involved. Most lesions associated with electrical burns occur in children and involve the lips and commissural areas. Ulcers formed due to thermal injuries are generally seen to occur on the posterior regions of the buccal mucosa and the palate.

Figure 2 A traumatic ulcer on the left lateral aspect of the tongue due to sharp teeth. Courtesy: Department of Oral Medicine and Radiology, KLEDC, Bangalore
Caustic chemical agents can damage any area of the oral mucous membrane. However, they are commonly seen on the gingival margins and buccal vestibular regions of the oral cavity. Very frequently these ulcers are covered by a whitish pseudomembrane which when peeled leaves behind a raw ulcerated surface (Figure 3). Some patients in the Indian subcontinent use cloves and topical pain balms meant for extraoral application over the gingiva to relieve tooth pain. Hence, most of the chemical burns are generally seen adjacent to carious teeth.
Diagnosis
The diagnosis of traumatic ulcerations is based on the history of trauma or insult (hot/cold or radiation therapy) prior to onset of ulcer. Mechanical trauma induced ulcers often have linear configuration. The depth of ulcer depends on nature of trauma. Generally the area surrounding the ulcer is inflamed. A traumatic factor will often be evident in the vicinity of the ulcer (e.g. sharp edge of tooth).
Management
 Consumption of a soft and bland diet.
Consumption of a soft and bland diet.
 Removal of traumatic factor (extraction of root stumps, supraerupted teeth and malposed third molars, sharp cuspal edges of teeth may be grounded, irritating dentures may be corrected, restoration of fractured teeth and orthodontic correction of malposed teeth) will cause the resolution of the ulcer in 10–14 days.
Removal of traumatic factor (extraction of root stumps, supraerupted teeth and malposed third molars, sharp cuspal edges of teeth may be grounded, irritating dentures may be corrected, restoration of fractured teeth and orthodontic correction of malposed teeth) will cause the resolution of the ulcer in 10–14 days.
 Patient may be advised to rinse his/her mouth with warm saline.
Patient may be advised to rinse his/her mouth with warm saline.
 Topical application of antiseptic and analgesic/anesthetic medication (choline salicylate 8.7%, benzylkonium 0.01% and lignocaine hydrochloride 2%—patient can be asked to apply the agent over the ulcers 10 minutes prior to food intake, 3–4 times a day).
Topical application of antiseptic and analgesic/anesthetic medication (choline salicylate 8.7%, benzylkonium 0.01% and lignocaine hydrochloride 2%—patient can be asked to apply the agent over the ulcers 10 minutes prior to food intake, 3–4 times a day).
 In case of multiple ulcers—analgesic/antiseptic mouth-wash (chlorhexidine gluconate 0.2% or benzydamine hydrochloride 0.15% mouthrinse—one teaspoon of the agent can be dissolved into 50 ml of water. This prepared solution is swished in the mouth for 1 minute. The patient is advised to rinse the mouth 3 times a day, 30 minutes after food intake).
In case of multiple ulcers—analgesic/antiseptic mouth-wash (chlorhexidine gluconate 0.2% or benzydamine hydrochloride 0.15% mouthrinse—one teaspoon of the agent can be dissolved into 50 ml of water. This prepared solution is swished in the mouth for 1 minute. The patient is advised to rinse the mouth 3 times a day, 30 minutes after food intake).
 Application of topical corticosteroids (triamcinolone acetonide oral paste 0.1%). Patient can be advised to apply the paste 30 minutes prior to food intake, 3 times a day for 2 weeks.
Application of topical corticosteroids (triamcinolone acetonide oral paste 0.1%). Patient can be advised to apply the paste 30 minutes prior to food intake, 3 times a day for 2 weeks.
 For extremely large and deep seated ulcers, penicillin may be administered (Capsule Amoxicillin, 500 mg, 3 times a day for 5 days) to prevent secondary infections.
For extremely large and deep seated ulcers, penicillin may be administered (Capsule Amoxicillin, 500 mg, 3 times a day for 5 days) to prevent secondary infections.
 Patients presenting with ulcers secondary to self-inflicted injuries may be referred to a psychiatrist or psychologist after symptomatically managing the ulcer.
Patients presenting with ulcers secondary to self-inflicted injuries may be referred to a psychiatrist or psychologist after symptomatically managing the ulcer.
Primary Herpetic Gingivostomatitis
Clinical features
 Primary herpetic gingivostomatitis has an acute onset.
Primary herpetic gingivostomatitis has an acute onset.
 Typically affects children (generally below 6 years of age), but this infection also occurs in adults (immunocompromised).
Typically affects children (generally below 6 years of age), but this infection also occurs in adults (immunocompromised).
 Males and females are equally affected.
Males and females are equally affected.
 Prodromal systemic symptoms (fever, malaise, myalgia) precede oral lesions by 2–3 days.
Prodromal systemic symptoms (fever, malaise, myalgia) precede oral lesions by 2–3 days.
 The skin, mucous membranes, eyes and central nervous system are the most commonly affected sites.
The skin, mucous membranes, eyes and central nervous system are the most commonly affected sites.
 Multiple oral ulcers affecting all parts of the mouth.
Multiple oral ulcers affecting all parts of the mouth.
 Generalized erythema of gingiva usually associated with multiple vesicles or ulcers (Figure 4).
Generalized erythema of gingiva usually associated with multiple vesicles or ulcers (Figure 4).

Figure 4 Gingival erythema, multiple small ulcers and vesicles in the attached gingiva in a 36-year-old man suffering from acute herpetic gingivostomatitis. Reproduced with permission from editor, JCDA. Ajar AH and Chauvin PJ. Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management. J Can Dent Assoc 2002;68(4):247–51
 Cervical lymphadenopathy occurs as a rule.
Cervical lymphadenopathy occurs as a rule.
 Food intake becomes difficult and dehydration may ensue.
Food intake becomes difficult and dehydration may ensue.
 Self-limiting condition in normal children. However, it may become disseminated in immunocompromised children or adults.
Self-limiting condition in normal children. However, it may become disseminated in immunocompromised children or adults.
Recurrent Herpes Infection
Recurrent infections of herpes can manifest in two forms:
1. Intraoral herpes (occurs on highly keratinized mucosa of hard palate/gingiva)
2. Herpes labialis (occurs along external vermillion border of lips).
Precipitating Factors
Clinical presentation
 Patients present with cluster of tiny fluid filled vesicles (Figure 5A–C) which rupture to form pinpoint ulcers. These ulcers may coalesce to form larger areas of ulceration.
Patients present with cluster of tiny fluid filled vesicles (Figure 5A–C) which rupture to form pinpoint ulcers. These ulcers may coalesce to form larger areas of ulceration.

Figure 5 (A) Vesicles on the upper lip in a patient with recurrent herpes labialis. (B) Ulcers formed subsequent to vesicle rupture in a patient with recurrent herpes labialis. Courtesy: Department of Oral Medicine and Radiology, MCODS, Mangalore. (C) Healing lesions of herpes labialis. Courtesy: Department of Oral Medicine and Radiology, KLEDC, Bangalore
 Lesions may be preceded by burning, itching, tingling sensation or pain in the region.
Lesions may be preceded by burning, itching, tingling sensation or pain in the region.
 The lesions last for 5–7 days and subside and subsequently recur. Now the frequency of recurrence may be varied.
The lesions last for 5–7 days and subside and subsequently recur. Now the frequency of recurrence may be varied.
 Occasionally associated with fever and pharyngitis.
Occasionally associated with fever and pharyngitis.
 As a consequence to healing an area of pigmentation is noticed at the site of the lesion (however this pigmented area is readily visualized only in fair skinned individuals).
As a consequence to healing an area of pigmentation is noticed at the site of the lesion (however this pigmented area is readily visualized only in fair skinned individuals).
Varicella Zoster Infection
Chicken Pox
The primary infection by varicella zoster virus usually affects children. It is characterized by the sudden onset of generalized pruritic vesicular rashes affecting the skin. The incubation period of the virus varies from 10 to 21 days. Approximately 50% of the affected children present with prodromal symptoms of fever, malaise, headache, and abdominal pain, which last for about 1–2 days before the appearance of the dermal lesions.
Dermal lesions
 Typical lesions of chicken pox, clinically exhibit four phases. The maculopapular phase (erythematous macules are evident), vesicular phase (minute fluid filled vesicles are seen), ulcerative phase (commonly seen on mucous membranes of oropharynx, vagina and conjunctiva) and the phase of healing (Figure 6).
Typical lesions of chicken pox, clinically exhibit four phases. The maculopapular phase (erythematous macules are evident), vesicular phase (minute fluid filled vesicles are seen), ulcerative phase (commonly seen on mucous membranes of oropharynx, vagina and conjunctiva) and the phase of healing (Figure 6).
 In the maculopapular phase erythematous macules are seen. In some patients, vesicles develop within the maculopapular rash giving rise to ‘dewdrop on a rose petal’ appearance.
In the maculopapular phase erythematous macules are seen. In some patients, vesicles develop within the maculopapular rash giving rise to ‘dewdrop on a rose petal’ appearance.
Herpes Zoster
Clinical features
 The clinical features depend on the dermatome involved.
The clinical features depend on the dermatome involved.
 The nerves that are commonly affected are C-3, T-5, L-1 and L-2.
The nerves that are commonly affected are C-3, T-5, L-1 and L-2.
 When the trigeminal nerve is involved, the ophthalmic division of the nerve is most commonly involved. About 15–20% of the affected individuals show involvement of the maxillary or mandibular division.
When the trigeminal nerve is involved, the ophthalmic division of the nerve is most commonly involved. About 15–20% of the affected individuals show involvement of the maxillary or mandibular division.
 Painful vesicles and/or ulcers seen both inside and outside the oral cavity, which stop abruptly at the midline (i.e. lesions do not cross midline) (Figure 7).
Painful vesicles and/or ulcers seen both inside and outside the oral cavity, which stop abruptly at the midline (i.e. lesions do not cross midline) (Figure 7).

Figure 7 Healed lesions of herpes zoster with scab formation. Characteristically, the lesions do not cross the midline and this patient had involvement of the ophthalmic, maxillary and mandibular divisions of the trigeminal nerve. Courtesy: Dr Sumanth
 Bilateral lesions may indicate severely immunocompromised state. Literature review reveals reports of necrosis of alveolar bone exfoliation of teeth in immunocompromised individuals.
Bilateral lesions may indicate severely immunocompromised state. Literature review reveals reports of necrosis of alveolar bone exfoliation of teeth in immunocompromised individuals.
 Occasionally pain may be present along the course of the affected nerve in the absence of vesicles. Such a manifestation is termed zoster sine herpete or zoster sine eruption.
Occasionally pain may be present along the course of the affected nerve in the absence of vesicles. Such a manifestation is termed zoster sine herpete or zoster sine eruption.
 Ramsay Hunt syndrome is a symptom complex associated with herpes zoster. It is characterized by varicella zoster infection affecting the geniculate ganglion of the facial nerve, unilateral facial paralysis and unilateral vesicular eruptions involving the oral mucosa and external ear.
Ramsay Hunt syndrome is a symptom complex associated with herpes zoster. It is characterized by varicella zoster infection affecting the geniculate ganglion of the facial nerve, unilateral facial paralysis and unilateral vesicular eruptions involving the oral mucosa and external ear.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses