Chapter 7
Traumatic Injuries to the Teeth and Oral Soft Tissues
Assessment of the traumatised patient
History
A comprehensive history should be taken of the traumatised patient at initial presentation. This should allow the clinician to make the decision whether the injury is suitable to be treated in a primary care setting or should be referred to a hospital/dental hospital.
Refer to a general hospital when there is a history of:
- loss of consciousness;
- vomiting;
- headache;
- amnesia;
- persistent coughing;
- difficulties in focusing the eyes.
Once it has been established that the injury is suitable for management in a primary care setting, the following questions relating to the injury should be asked:
- What is the nature of the injury? (If tooth avulsion, note the extra-alveolar dry time, storage medium and if the tooth was contaminated.)
- How, when (include date and time) and where did the injury occur?
- Are all teeth/broken fragments accounted for?
- Is there any disruption in the occlusion?
Medical history
General health (cardiac, respiratory, fits/faints, episodes of hospitalisation, endocrine, any current treatment by general practioner or hospital specialist) including tetanus status.
Examination
The examination of the patient should begin on entering the surgery. The general state of the patient and the specific injuries should be noted. The ABCDE approach (see Chapter 11) should be used to assess the injured patient.
Extra-oral examination
- Soft tissues: Facial asymmetry, swellings, bruises, lacerations, puncture wounds.
- Hard tissues: Bony step deformity on palpation, deviation/pain on opening/closing, temporomandibular joint.
- Diagram: Draw a rough diagram noting all aforementioned observations.
- The clinician should only attempt suturing when they feel confident in their abilities to achieve an aesthetic and functional result for superficial extra-oral and intra-oral wounds (once thoroughly débrided and cleaned). Gaping facial wounds and deep intra-oral wounds require an immediate referral to the local maxillofacial department. Extra-oral wounds should be secured with Steri-strips® prior to referral if possible.
Intra-oral examination
- Soft tissues: To include thorough examination of all soft tissues including possible ‘through and through’ injuries, and injuries involving the floor of the mouth or tongue. Examine for swellings, lacerations, ecchymosis.
- Bony hard tissues: Check for steps/disruption on movements.
- Dental hard tissues:
- Chart teeth: Account for all missing teeth/fragments.
- Chart: Any fractures involving crown, crown-root or root.
- Note: Mobility, displacement, reaction to percussion, occlusion, reaction to vitality tests.
- Special tests:
- Vitality: Electric pulp test/ethyl chloride test.
- Radiographs: At least two views to identify position/displacement and to diagnose injury (e.g. periapical and upper anterior occlusal or, two periapicals at different angles).
- Soft tissue radiographs: If fragments are unaccounted for and there is related soft tissue injury.
Management of traumatic dental injuries
Management of soft tissue injuries
- Lavage (saline/chlorhexidine)
- Debridement of wound
- Arrest haemorrhage (direct pressure)
- Prescribe chlorhexidine mouthwash
- Where wound contamination or poor oral hygiene, antibiotics should be prescribed.
Management of dental injuries
Management of injuries will be discussed as per diagnosis of injury to either the permanent or primary tooth and will be divided into immediate, intermediate and long-term follow-up. For all dental injuries, the patient should be advised to have a soft diet for a week, and to ensure the area is kept clean using 0.2% chlorhexidine mouthwash. This may help to prevent plaque accumulation and keep soft tissues healthy. In very young children, parents should be encouraged to keep the affected area clean using chlorhexidine mouthwash on gauze, if the child is unable to expectorate.
All dental/soft tissue injuries should be followed up and the essential trauma chart (Table 7.1) completed at each follow-up visit. This will ensure that any problems that may occur are identified early and can be dealt with in a timely manner.
Table 7.1 Example of essential trauma chart.
Injuries to the hard dental tissues and the pulp
Enamel infraction
Enamel infraction relates to an incomplete fracture (crack) of the enamel without loss of tooth structure (see Figures 7.1 and 7.2).
Figure 7.1 Coronal fractures upper right lateral incisor (retained/fractured tooth fragment in place), upper right central incisor showing a star-shaped enamel infracture with embedded grit on the labial aspect and upper left central incisor showing a complicated crown fracture.

Figure 7.2 The same patient with all loose tooth fragments removed. Complicated crown fractures confirmed on the upper right lateral incisor and upper left central incisor. Note the soft tissue injuries to the upper lip.

Permanent dentition
Immediate management
- Result of investigations:
- Visible fracture line
- Not tender to percussion (TTP)
- Normal mobility
- Positive to vitality testing
- No radiographic abnormalities (recommend periapical view)
- Treatment – no immediate treatment required
Intermediate management
Where marked infraction present, etch and seal with resin to prevent discolouration of the infraction lines.
Follow-up
No follow-up needed (unless associated with other dental injuries).
Primary dentition
As discussed in the preceding text for permanent dentition.
Enamel fracture
A fracture confined to the enamel with loss of tooth structure.
Permanent dentition
Immediate management
- Result of investigations:
- Visible loss of enamel, no visible sign of exposed dentine
- Not TTP
- Normal mobility
- Positive to vitality testing, if negative, monitor until definitive diagnosis
- Radiographically, extent of tooth substance loss is visible
- Treatment (dependent on size of fracture):
- If tooth fragment available, bond to tooth
- Smooth sharp edges
- Restore with composite resin
Intermediate management
- Investigations:
- Radiograph at 6–8 weeks
- Treatment:
- Not indicated
Follow-up
- Investigations:
- Radiograph at 1 year
Primary dentition
Immediate management
- Result of investigations:
- Visible loss of enamel, no visible sign of exposed dentine
- Not TTP
- Normal mobility
- Enamel loss visible radiographically
- Treatment:
- Smooth sharp edges with Soflex® disc
Intermediate management
- Investigations:
- Review at 1 month, 3 months and 6 months
- Treatment:
- No intermediate treatment indicated unless tooth become symptomatic
Follow-up
- To review after every 4–6 months until exfoliation
- Radiograph if clinical signs are abnormal
Enamel/dentine fracture
Enamel and dentine fractures with loss of tooth structure, but not involving the pulp.
Permanent dentition
Immediate management
- Result of investigations:
- Visible loss of enamel and dentine, no visible sign of exposed pulp tissue
- Not TTP
- Normal mobility
- Positive to vitality testing; if negative, monitor until definitive diagnosis
- Radiographically, extent of tooth substance loss visible
- Consider soft tissue radiograph if unable to locate lost tooth tissue
- Treatment:
- Bond tooth fragment, if available.
- If tooth fragment is not available, place a composite bandage (see below) or permanent composite restoration.
- Composite bandage – cover exposed dentine with calcium hydroxide. Follow with etch, bond and placement of a light cured composite resin ensuring the whole fracture site is covered.
Intermediate management
- Treatment:
- Restoration with definitive composite material to restore function and aesthetics
Follow-up
- Clinical and radiographic follow-up at 6–8 weeks and 1 year.
Primary dentition
Immediate management
- Result of investigations:
- As discussed in the preceding text for permanent dentition, but no vitality testing
- Treatment:
- Smooth sharp edges with a Soflex® disc
- Restore subject to cooperation with composite material
Follow-up
- Clinical and radiograph review at 6–8 weeks
- Radiograph if tooth becomes symptomatic, otherwise, monitor for asymptomatic exfoliation
Enamel/dentine/pulp fracture
A fracture involving enamel and dentine with loss of tooth structure and exposure of the pulp.
Permanent dentition
Immediate management
- Result of investigations:
- Visible loss of enamel and dentine with exposed pulp tissue
- Not usually tender to percussion
- Normal mobility
- Pulp usually sensitive to touch (If negative, has there been previous trauma?)
- Radiographically, extent of tooth substance loss is visible
- Treatment:
- In young patients with open apices (or even closed apices), attempt to preserve pulp vitality:
- Pulp capping: Use in vital teeth with exposures less than 1 mm and less than 24 hours old:
- With local anaesthetic and appropriate isolation, apply pulp-capping material (calcium hydroxide compound/ mineral trioxide aggregate (MTA)) to exposed pulp tissue. Ensure good seal over pulp cap with either re-bonding of tooth fragment or composite bandage.
- Partial pulpotomy: Where exposure is minimal and less than 2 weeks old:
- With local anaesthetic and under rubber dam, excise the coronal pulp tissue to a depth of 2 mm below the exposure site. Haemorrhage should be arrested with a clean cotton wool pledget and sterile water only. Apply non-setting calcium hydroxide, followed by setting calcium hydroxide calcium hydroxide over the healthy pulp tissue. Restore the tooth with composite. If haemorrhage continues after removal of the initial 2 mm of pulp tissue, this is indicative of necrotic tissue. A further 2 mm should be removed until healthy pulp tissue is reached. If this does not look achievable due to continuing haemorrhage, proceed to coronal pulpotomy.
- Coronal pulpotomy: In vital teeth where exposure is large and greater than 2 weeks old:
- With local anaesthetic and under rubber dam, coronal pulp tissue should be excised to the level of the cervical constriction. Haemorrhage should be arrested with a clean cotton wool pledget and sterile water only. Apply 2–3 mm of non-setting calcium hydroxide, followed by setting calcium hydroxide. Restore tooth with composite restoration to ensure good seal (Figures 7.3 to 7.6).
- Pulp capping: Use in vital teeth with exposures less than 1 mm and less than 24 hours old:
- In older patients with associated luxation injuries:
- Treatment of choice is extirpation and eventual root canal treatment.
- In young patients with open apices (or even closed apices), attempt to preserve pulp vitality:
Figure 7.3 Both upper central incisors with complicated crown fractures.

Figure 7.4 Pulpotomies carried out on both upper permanent central incisor teeth.
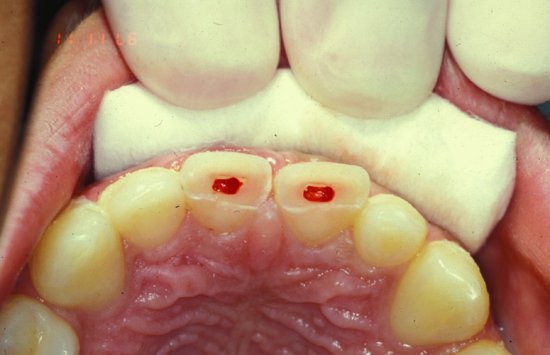
Figure 7.5 Calcium hydroxide paste placed over healthy amputated pulp tissue.

Figure 7.6 Acid-etch composite ‘bandage’ placed to give hermetic seal.

Intermediate management
- Treatment:
- Ensure all definitive restorations have an excellent seal to avoid bacterial contamination of the pulp tissue.
Follow-up
- Review appointments: At 1 month, 3 months, 6 months, 1 year, 18 months and 2 years.
- If there are any signs of pathology, then the following should be done:
- Tooth with open apex: Extirpation of necrotic pulp tissue and dress the root canal with non-setting calcium hydroxide. Achieve apexification with 3 monthly re-dresses using non-setting calcium hydroxide paste. Alternatively, place MTA at the open apex to achieve an artificial barrier. Eventually, definitive root filling once barrier achieved.
- Tooth with closed apex: Extirpate necrotic pulp tissue and dress tooth with non-setting calcium hydroxide. On evidence of stabilisation of the pathology, a definitive root canal treatment can be placed.
- If there are any signs of pathology, then the following should be done:
Primary dentition
Immediate management
- Result of investigations:
- Visible loss of enamel and dentine with exposed pulp tissue
- Not usually tender to percussion
- Normal mobility
- Radiographically, loss of tooth substance is visible
- Treatment:
- Teeth with fractures into the pulp require extraction unless child can cooperate for pulp treatment.
Follow-up
- If pulp treatment performed, monitor at regular intervals to ensure asymptomatic and no signs of pathology.
- If extraction performed, monitor adjacent teeth for signs o/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


