7
Tooth Resorption
7.1 Introduction
Tooth resorption is the destruction of the hard dental tissues by osteoclasts. Bone is continuously being resorbed (broken down) by the osteoclasts and re-formed (deposited) by osteoblasts. The resorption of the roots of the deciduous teeth is a physiological process. Pathological tooth resorption includes external transient resorption, which arrests spontaneously, and progressive resorption, which starts from within the tooth in the walls of the pulp cavity or on the external surface of the tooth.
The multinucleated (>20 nuclei) osteoclasts likely develop from haemopoietic, pluripotent stem cells circulating within the blood,83 284 which first transform into mononuclear precursors, and which then fuse together,84 possibly under the influence of colony-stimulating factors.305 The osteoclast precursor cells attach to the bone and remain dormant until they are signalled by the osteoblasts to proliferate and fuse to form the osteoclasts.
Factors released by the osteoblasts, such as the receptor activator of nuclear factor κB ligand (RANKL), regulate the functions of the osteoclasts.330 Pre-osteoclasts treated with RANKL transform into osteoclasts. Osteoprotegerin (a member of the tumour necrosis factor (TNF) receptor superfamily) suppresses the resorption activity of the osteoclasts.376
The tooth-resorbing cells, the odontoclasts, may be smaller than the osteoclasts, with a maximum of 10 nuclei.105 160 The existence of specific odontoclasts is not confirmed but if they do exist they have the same origin as the osteoclasts.397 Cementoblasts may transform into cementoclasts.55
The ruffle border of the osteoclasts, which consists of a system of canals, is the active site of resorption. The osteoclasts secrete factors that lower the extracellular pH, resulting in dissolution of the mineral bone phase, and attack the organic matrix with enzymes.22 46 284 313 330
Antiresorptive Factors
A healthy periodontal ligament prevents migration of alveolar bone components towards the root,139 295 but when the ligament is compromised, osteoclasts spread over and resorb the denuded cementum and dentine.69 436
Pre-cementum (a 3–8 µm thick, chiefly organic layer on the cementum)46 appears to be protective,244 as osteoclasts cannot bind to such non-mineralised tissues.162 314 369 422 The predentine is also protective.162 194 The circumpulpal dentine, which is less mineralised than the mantle dentine184 and richer in acid polysaccharides,447 protects the pulp from cervical resorption for a considerable period of time. The dentinal destruction proceeds and encircles the pulp cavity, but the pulp itself remains vital.146 396 447 Collagen-rich predentine is supposedly formed in response to the eventual resorption.146 Macrophages seeded on predentine and demineralised dentine remain attached and do not migrate. The organic, non-collagen component of dentine may contain an inhibitor against macrophages and osteoclasts.435 436 Research is ongoing to discover inhibitors, for instance a collagenase or protease,168 258 and to understand the processes by which cells disperse over the surface.434
Cementum and dentine contain mucopolysaccharides that are active in the ligament of resorbing deciduous teeth, but these substances have not been found when these teeth are ankylosed.8
Denervation of the inferior alveolar nerve was found to result in ankylosis of the second molars. It was proposed that the microscopic epithelial islands of Malassez (see Chapter 3)267 329 may help maintain the width of the periodontal space. Denervation results in loss of the islands of Malassez, which may then allow an increase in the number of osteoclasts in the periodontal space.139 However, this idea of protection provided by the network of epithelial islands has not gained support,422 and nor has the notion of protection by Sharpey’s fibres in the cementum.
7.2 Physiological External Root Resorption: Deciduous Teeth
Physiological resorption is the breakdown of the roots of the deciduous teeth by osteoclasts. Resorption of the deciduous roots, which is necessary for exfoliation, starts soon after root completion on the linguo-apical aspect of the deciduous anterior teeth roots and at the inner side of the molar roots. Pressure exerted by the succedaneous tooth damages the cells lying in the path of eruption, which secrete chemical mediators such as prostaglandin E2, hormones, neurotransmitters, cytokines and monokines (including interleukins), and proteinases.22 75 During resorption, the cementoblasts adjacent to the osteoclasts continue to regularly deposit small amounts of cementum and bundles of collagen fibres;377 this “remodelling” process activates the osteoclasts. If there is agenesis of the succedaneous tooth, the root of the predecessor may or may not be resorbed.288
While a deciduous root is being resorbed, any permanent root in the vicinity is not resorbed. This is because of the differences in the spatial pattern of expression of two extracellular matrix proteins (osteopontin and bone sialoprotein) which influence osteoclast adhesion and activity.251
7.3 Transient External Root Resorption: Both Dentitions
Transient resorption is limited osteoclastic resorption of cementum and the adjacent superficial dentine, with apposition of cementum in the repair phase. Transient resorption arrests spontaneously. This innocuous289 process occurs in almost all dentitions.183 The minute apical shortening and lateral defects caused by transient resorption are often not visible on radiographs. A localised absence of periradicular space allows the alveolar bone cells to come in contact with the root. The normal renewal of the periodontal ligament may underlie the transient destruction,44 but other causes have also been suggested.
7.3.1 Trauma
Mechanical injuries to the teeth cause transient external resorption when a small part of the periodontal ligament is lost as a consequence of a local, sterile inflammatory response.14 22 421 Transient internal resorption at the apical end follows more severe injuries and allows ingress of a vascular network, which aids pulpal healing.14 The process arrests spontaneously14 15 18 in the absence of ongoing stimulation.141 Symptoms may include short-term crown discoloration and temporary loss of pulpal sensibility.14
Healing depends on the outcome of the competition between the bone cells and periodontal cells.22 260 Renewal of the ligament via differentiation of adjacent ligament cells occurs when only a small area (up to a few square millimetres) of a generally healthy periodontal ligament is involved.351 In contrast with transient resorption, bone cells invade the ligament space permanently when larger areas are damaged.141 Healing involves deposition of cellular cementum.171 245 246 297 When the resorptive phase ends, repair is accomplished within a few weeks.38 141 259 In experimental root cavities, macrophage-like cells from the blood stream have been observed after 24 hours. Three days later lacunae were formed by the osteoclasts, which were attributed to activity of cells with a ruffle border, and fibroblast-like cells from the periphery started to colonise the cavities. Six weeks later the cavities showed formation of reparative cementum.209 210 Receptors for the epidermal growth factor in the cell membrane of the active cementoblasts in the neighbourhood of the resorption lacunae are “switched on”.397 The periradicular space regained its normal width.
7.3.2 Orthodontics
Orthodontic tooth movement may cause transient external root resorption.104 288 At the site where the orthodontic force is directed, the periodontal ligament becomes compressed and the pressure is transmitted to the adjacent bone. The pressure exerted by the orthodontic force interferes with the metabolism of the ligament and its cells secrete the mediators already mentioned above, whereupon osteoclasts residing in the bone marrow resorb the bone. As the cementum is more resistant, when bone is resorbed, the tooth moves and the hyalinised tissue (sterile necrosis) is replaced by newly formed vital tissue.
When the orthodontic force is applied, regardless of whether is it heavy or light, the blood supply within the periodontal ligament is compromised when the hydrostatic pressure exceeds the capillary blood pressure.452 The necrotic ligament tissues stimulate cellular activity that degrades these tissues, and the root is no longer protected from the osteoclasts.108 On the pressure side,282 root resorption is seen in relation to the hyalinised zones.237
Healing
After the pressure from the orthodontic force is relieved, the necrotic tissue is cleared. Cementoblasts lay down cementum in the resorptive lesions,108 334 followed by the renewal of the periodontal ligament. The process (in rats) takes about 3 weeks.80 Root resorption arrests either during the late phase of active orthodontic treatment171 or in the retention period.93 In the post-treatment period, sharp root edges become rounded.357 In one-quarter of a sample of adolescents undergoing orthodontic treatment, repair started 1 week after the placement of retention appliances, and in the remaining sample after 8 weeks.334
Prevalence and Degree of Orthodontic Root Resorption
The reported prevalence of tooth resorption caused by orthodontic treatment varies between 3.5% and 100%75 130 due to differences in identification criteria and treatment methods used in the various studies. The maxillary central incisor is most frequently affected, followed by the mandibular incisors.108 213 292 357 “Blunting” (shortening) of the root apex is often the only sign of orthodontic root resorption, in general a few millimetres, and occasionally reported to be much as 5–6.5 mm.3 16 168 240 264 269 281 299 345 357 Maxillary lateral incisors with abnormal root morphology become more blunted than the central incisors.373 Treatment involving extraction of first premolars leads to greater blunting of the central incisor roots than non-extraction therapy.374 Full-grown roots show more resorption than incomplete ones, and this is a reason for early orthodontic treatment,181 but whether adults undergoing orthodontic treatment show more resorption than adolescents is doubtful.264 299
Blunting up to 3 mm leads to loss of tooth attachment as much as that caused by 1 mm loss of cervical bone in periodontitis. When the apical resorption is progressive, the greater root circumference increases the amount of attachment loss disproportionately.214
Factors
- Studies show either a weak or no association between treatment duration and degree of blunting.50 95 181 264 298 345 412 A pause in treatment leads to cessation of resorption,256 282 but Owman-Moll et al. found that the effects of orthodontic appliances exerting a continuous force were no worse than those of a discontinuous force.333
- Appliances: Begg’s orthodontic treatment is accompanied by resorption,240 but use of intermaxillary elastics with other appliances may often cause more resorption than seen with Begg’s or use of magnets.76 Other studies have found similar degree of resorption with the edgewise and Begg’s techniques.255 358 Edgewise appliances might generate stronger forces than the “straight wire” appliance, which involves using pre-formed archwires, which are deformed on insertion into the brackets attached to the teeth. These archwires then slowly attempt to recover their original shape, and in the process the teeth are moved into the desired arch form. Orthodontic tipping movements may be less damaging than bodily movement with fixed appliances.130
- The distance over which the tooth is moved is related to the severity of root resorption.108 282 298 The larger the apical displacement of the incisors, the more severely blunted are the roots.374
- The strength of the force may not be a factor,108 282 but this is an oversimplification.374 A fourfold increased force, from 50 to 200 g, indeed may not cause more frequent or more severe resorption,336 but higher force magnitudes may be detrimental. A light force may initially seem more detrimental than a stronger one,335 just like a light force has been shown to move a tooth initially over a greater distance than a stronger force.225 335 However, the cementoid tends to decrease in thickness on the side of compression, where more resorption occurs than on the tension side, and this has been shown to be more with a heavy force compared with a light force.453
- The degree of resorption has also been found to vary regardless of the above factors.7 239 292 333 The bone quality and effects of medicaments and diseases also co-determine whether resorption occurs.
Hypocalcaemia in cats undergoing orthodontics was associated with an increase in the number of osteoclasts and root resorption.120 Hyper(para)thyroidism promotes alveolar bone remodelling. After parathormone therapy, the intercellular space between the osteoblasts is widened, thereby offering the osteoclasts the opportunity to colonise the bone surface; the cementoblasts do not do the same.261
Medicaments such as thyroxine that increase alkaline phosphatase activity, affect bone metabolism.349 In one study, administration of 0.5 g thyroxine/day arrested initial resorption during orthodontic treatment.266 However, before this can be used clinically, it needs to be clarified which patients may be treated in this way.90 350 Administering prostaglandin E2 stimulated bone resorption and initially speeded up tooth movement, though inconsistently.65 Indometacin counteracts the action of prostaglandins and tooth movement.148 Bisphosphonate, a potent blocker of bone resorption, affected tooth movement (and also tooth eruption) negatively.203 Phenytoin (anti-epileptic) reduces the number of osteoclasts in the bone walls on the pressure side and thereby delays tooth movement.216
Ultrasound may be preventive.117 Low-intensity ultrasound has an anti-inflammatory action and when it was applied for 20 minutes/day to premolars that required to be tipped, the numbers and areas of resorption lacunae decreased and healing with hypercementosis was seen.117
- Direction of tooth movement. Intrusion, torquing (rotating) and bodily tooth movements are, in this order, the most likely to cause orthodontic root resorption.108 Torquing immediately caused resorption. Continuous torquing of premolars resulted in formation of many resorption lacunae.89 206 Resorption is frequently seen after intrusion,50 but a light force caused, in 4 months, only a slight blunting of the roots.95 The duration of intrusion may be more influential than the degree of intrusion,268 specially in maxillary incisors versus the mandibular ones.292 However other studies did not report a significant effect of duration.103 In adults, retraction has been found to be most damaging.47
- Anatomical features, such as the proximity of nasal floor may be a limiting factor for intrusion of the maxillary incisors.103 The risk of severe resorption is increased 20-fold for roots situated close to the cortical bone,213 however, others have suggest that the amount of tooth movement was more important.298 Severe resorption occurs when the apex is moved outside the bone.164
- Predisposing factors are overjet, anterior open bite (tongue thrusting), mouth breathing, thumb sucking and nail biting (which also leads to blunts in the absence of orthodontic treatment), trauma prior to orthodontic treatment, deviations in root morphology and gender.75 76 168 169 255 264 326 366 373 413 In adults, treatment duration and the degree to which the apex was moved were found to be related to resorption, and this was more in men than in women;47 however, this was not the case in a study of brothers and sisters.170 Teeth with blunt and pipette-shaped roots might particularly be at risk.254 Resorption on the prominent sides of the root during rotational movements emphasises the importance of the root morphology.206
- In asthmatic people, the incidence, but not the amount, of root resorption may be increased.293 Vital teeth may be resorbed more than endodontically treated teeth,298 299 357 405 but others have not found a difference.454 A Class III molar relationship increases the risk of severe root resorption.213
7.3.3 Chronic Periodontitis
The more severe is the periodontitis, the greater is the amount of resorption of the root surface in the gingival third of the roots and apically.172 361 The transient resorption may become progressive. Repair with cementum has been observed after improvements in oral hygiene.109
7.3.4 Other Causes
Blunting has been reported in 7–10% of patients with occlusal overload after extraction and loss of periodontal attachment.169 An experimental study found that occlusal overload results in resorption of the cementum without ankylosis.367 The distal root of mandibular permanent second molar may become blunted as part of ageing.
7.4 Progressive Resorption: Both Dentitions
In progressive resorption, the continuation of the process depends on ongoing stimulation of the osteoclasts.141 Several types of internal and external resorption exist.
7.4.1 Internal Resorption
Internal resorption is progressive breakdown caused by osteoclasts, starting at the internal (pulpal) walls and progressing to the periphery of the tooth, sometimes with formation of bone-like dentine.
Types and Macroscopic Appearance
A vital pulp is needed for the initiation and progression of internal resorption.18 The anomaly is commonly detected incidentally on radiographs. Clinical symptoms are absent or may not be noticed by the patient or the dentist. There are three types of internal resorption:
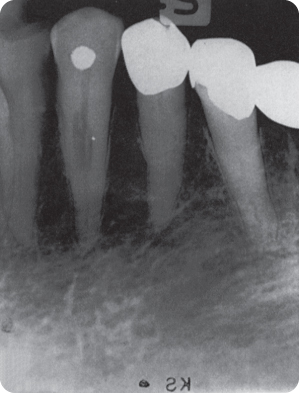
- Internal inflammatory resorption (more recently termed radial pulp enlargement resorption). Radiographs show an oval to round and rather smooth edged radiolucent widening of the pulp cavity (Figure 7.1) or apically. Unless the lesion has advanced to the root surface (Figure 7.2), dentine (and continuous forming53 cementum) separates the lesion from the periradicular space.
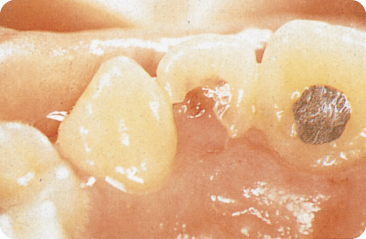
- Internal replacement resorption (metaplastic pulp resorption) (Figure 7.3) is associated with irregular, radiolucent pulpal widening with radiopaque areas where osteodentine is formed. A well-demarcated lesion may distinguish internal from external resorption,144 but which as such is probably not true.
- Internal tunnelling resorption. This process of tooth tissue breakdown after an injury is characterised by the formation of a “burrow” or tunnel behind the predentine layer, along the pulp chamber, occasionally extending into the root. Ultimately the tunnel and the pulp chamber are obliterated.22
Figure 7.1 Internal inflammatory resorption.
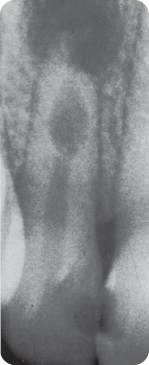
Figure 7.2 Internal inflammatory resorption perforating the root.

Figure 7.3 Internal replacement resorption in a canine.
On radiographs, areas of external labial/buccal and lingual resorption are projected over the pulp cavity and may mistakenly be diagnosed as internal resorption. If on taking radiographs at an angle (from mesial and distal) the lesions are projected outside of the pulp contour, they are external, and if not, they are internal.22 The ligament/alveolar bone is normal, unless the root surface is involved.67
Internal defects are stated not to perforate the external root surfaces, because it is unlikely that both the predentine/odontoblastic layer and the cementum/cementoblasts are involved in the same lesion.271
When internal resorption reaches the dentino-enamel junction, the pulp shines through the enamel: this is called pink spot (of Mummery) (Figure 7.4).310 A pulp polyp, a proliferation of pulp tissue, is seen (Figure 7.5) when the process breaks through the enamel.392
Figure 7.4 The pink spot is the result of either internal resorption in the crown or cervical resorption starting in the root.

Figure 7.5 A pulp polyp formed due to progression of an internal resorption lesion from within the crown towards the tooth surface.
Microscopic Appearance and Associated Findings
The resorptive lesions are filled with proliferating granulation tissue. Irregular lacunae (of Howship) in the pulpal walls contain macrophages in the predentine and osteoclasts in the dentine.435 Resorbing cells showed strong acid phosphatase activity, similar to osteoclasts.437
The predentine is resorbed locally by the action of the macrophages/enzymes but new predentine is not laid down because of the death of the odontoblasts. The osteoclasts or their precursors are thus no longer prevented from reaching the dentine. However, it is only after the granulation-like tissue comes in contact with mineralised dentine that the osteoclasts attack the dentine. The internal resorptive activity usually occurs in relation to an infected vital pulp, but the pulp may also be necrotic coronal to the resorptive defect.418 Root predentine may also undergo physiological “resorption”, as part of ageing, starting apically.408
In replacement resorption, bone-like dentine is formed within the lesion, by odontoblast-like cells. Phases of clastic and blastic activity are interrupted by intermittent resting periods.152
Aetiology and Epidemiology
The prevalence of internal resorption in the permanent teeth is 0.1–1.6%;346 it is lower in the deciduous dentition.392 In general, only one tooth per dentition is involved. The causes of internal resorption can be divided into three groups: inflammatory, systemic and idiopathic.
Inflammation-Related Causes
Replacement resorption accompanies moderate pulpal inflammation and inflammatory resorption is seen in more severe pulpitis.275
Deep Caries (Caries Profunda)
Rarely, pulpitis caused by deep carious lesions results in internal resorption.415 The resorptive lesions always contain inflammatory cells.275 Inadequate caries removal is considered another cause.228
Trauma
Within a few weeks after tooth injury, internal resorption may start as a consequence of pulp inflammation. After luxation (traumatically displaced tooth) about 1.5% of deciduous and permanent teeth undergo internal resorption.22 221 Pulpitis may also develop due to microleakage through a crack in the tooth.
Iatrogenic
Restorative dental materials may elicit an inflammatory pulpal reaction, as does microleakage along the cavity walls. Insufficient water cooling during cutting procedures in the permanent teeth309 has been implicated. With cooling, cavity preparation with a coarse diamond bur results in rise in the pulpal temperature of about 3 °C, which does not lead to pulpal damage. Despite this, short intervals of rest during preparation are advised.332 A temperature rise during external bleaching of newly erupted teeth could lead to internal resorption.389
Brief heat application to the enamel to several hundred degree Celsius has been shown to cause reversible pulpitis.136 A rise in temperature of 42.5 °C and 47 °C led to irreversible pulpal damage in 15% and 60% of the pulps, respectivley.450 A gradual increase to 49 °C also led to irreversible pulpal damage.10
In an in vitro study, application of heat at 60 °C to amalgam and composite fillings with para-pulpal pins elevated the temperature in the pulp to about 45 °C.33 Most people consume coffee and tea that is at a temperature of 55–68 °C,102 which elevates the temperature in pulps under amalgam fillings by just a few degrees.296 In another study, heat application to the teeth until the subjects reported pain and thereafter maintained for 30 seconds did not affect the pulp.40
In an in vivo study, light curing of a composite increased the mean temperature of the filling and surrounding tissues by 11.7 °C maximally.198 Finishing composite restorations with flexible, coarse discs was found to raise the pulp temperature to a mean of 45 °C (maximum 50 °C); which may endanger the pulp.77 There are no reports of development of internal resorption after these procedures.
Direct Pulp Capping/Vital Amputation
Direct pulp capping/vital amputation with calcium hydroxide (Ca(OH)2) and glutaraldehyde (7%),140 formocresol,185 and zinc oxide-eugenol cement276 is a major cause of internal resorption in deciduous teeth.275 385 415 Ferric sulfate medication was found to be worse than sodium hypochlorite.455 A blood clot between the vital pulp and the Ca(OH)2 dressing384 or an operative procedure such as aggressive amputation technique,22 have also been implicated. Mineral trioxide aggregate (MTA) may be as effective as Ca(OH)2 or superior456 as it has better qualities, and is increasingly used in place of calcium hydroxide.
After pulpotomy with Ca(OH)2, 80% of one sample of deciduous molars showed internal resorption within 0.5–2 years.275 Other studies have reported rates of 20–33% after 1 year.385 Removal of the blood clot from the pulp surface prior to application of the dressing markedly reduced the likelihood of resorption.386
Formocresol, a controversial medicament, has been found to induce internal resorption in some 10% of cases,185 194 but only in 2% of permanent teeth with acute pulpitis.194 Similar clinical and radiographic success has been reported with pulp capping with formocresol and the non-toxic ferric sulfate.457 Half of one sample of pulps with zinc oxide-eugenol cement dressings showed internal resorption on radiographs,276 but histological examination revealed that all teeth were affected.276 277
Orthodontics
Orthodontic treatment in adults and traumatic occlusion occasionally cause internal resorption;71 228 353 this is because movement of teeth with small apical foramina may lead to pulpal inflammation due to the reduction in blood supply.
Systemic Disease
Internal resorption lesions in the lower incisors of a patient with end-stage renal disease resolved after kidney transplantation,200 but in a study of patients with chronic renal failure no internal resorption was found.2 Internal and external resorption was seen in patients with hypophosphatasia.66 Herpes zoster (shingles) seems causative403 and some systemic diseases may lead to internal resorption in multiple teeth.353
Reactivation of latent varicella virus (chicken pox virus) leads to herpes zoster: neuralgia is followed by vesicular eruptions on the part of skin that is innervated by the nerve fibres of the infected ganglion. In about 20% of />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


