Chapter 7
Safety
Aim
The aim of this chapter is to discuss factors related to the safety of local anaesthesia in dentistry.
Outcome
After reading this chapter you should have an understanding of important medical conditions and drug interactions which impact upon the use of local anaesthesia. In addition, you will have an awareness of the safe maximum doses.
Introduction and Terminology
Local anaesthetics have a remarkable safety record in dentistry. This should not lead to complacency in their use. Some groups of the population are more at risk of unwanted effects than others. Among these individuals with increased risk are children, the elderly and medically compromised patients. The cessation of general anaesthetic services in dental practice means that more treatments are being provided for children under local anaesthesia in dentistry. Therefore, safety issues are of increasing importance. As with all adverse reactions, prevention is better than cure.
A major factor in reducing adverse reactions is eliciting a thorough medical and drug history from the patient before injection. The importance of history taking cannot be overemphasised.
The unwanted effects of dental local anaesthesia can occur due to:
-
physical trauma
-
chemical trauma
-
inappropriate site of deposition
-
toxicity
-
allergy
-
an underlying medical condition
-
drug interactions.
Physical Trauma
Trauma can occur at two stages. First, the needle may cause it. Secondly, it may arise as a result of self-injury in an anaesthetised area.
During regional block techniques the needle may damage the nerve trunk. This can cause long-lasting altered sensation, either anaesthesia or paraesthesia. The management of this problem is discussed in Chapter 8. Penetration of a blood vessel may produce bleeding into muscle (for example, the medial pterygoid may be traumatised during an inferior alveolar nerve block). This may produce muscle spasm resulting in trismus.
Self-inflicted trauma may occur if the patient inadvertently, or deliberately, bites an anaesthetised area. This can be a potential problem with children and therefore the patient and parent should be advised about the dangers of biting the area anaesthetised (Fig 7-1).

Fig 7-1 A self-inflicted injury following an inferior alveolar nerve block.
Chemical Trauma
In high concentration local anaesthetics may damage nerves. This can result in long-lasting altered sensation and is discussed in Chapter 8.
Inappropriate Site of Deposition
Occasionally, local anaesthetics are injected in the wrong place such as intravascularly or into the parotid gland.
Intravascular injection
The incidence of intravascular injection varies from site to site in the mouth. The routine use of an aspirating technique is recommended to reduce the chances of inadvertent injection into a blood vessel. During inferior alveolar nerve block injections, incidences of positive aspirates up to 20% of injections have been reported. In other sites, such as the maxillary buccal sulcus, the figure is around 2%. Intravascular injection may cause:
-
pain
-
localised blanching
-
cranial effects
-
systemic effects.
Although the needle may penetrate arteries or veins, it is unusual to enter the lumen of an artery. This is because arteries tend to slip away from the needle unless firmly attached to bone. Entry of a local anaesthetic into an artery will cause localised pain and blanching. Transport of the local anaesthetic in a cranial direction has occasionally caused transient blindness in one eye, limitation in eye movement leading to double vision, and temporary deafness. The most dramatic effect is transfer of material into the brain causing transient hemiplegia. Fortunately, although reported, this is an extremely rare occurrence. Nevertheless, it does dramatically illustrate the importance of aspiration prior to and during injection.
Inadvertent injection into a vein is more common than intra-arterial deposition. Systemic distribution of the anaesthetic agent and any added vasoconstrictor would follow intravenous injection. This may produce toxicity and this is described below.
Injection into parotid gland
The facial nerve traverses the parotid gland. Accidental injection deep to the parotid sheath during an inferior alveolar nerve block will introduce solution into the substance of the gland. This can result in anaesthetic solution affecting the facial nerve. Motor nerves are susceptible to the actions of local anaesthetics. If the facial nerve is affected, the patient will experience hemifacial paresis. The major problem that results is inability of the patient to close the eyelids on the affected side. This is not a dangerous condition so long as the affected eye is protected during the duration of the paralysis. The paralysis will resolve as the effect of the anaesthetic wears off. Clearly, this scenario is best avoided and steps can be taken to minimise the chances of hemifacial paralysis occurring. Ensuring that the needle has contacted bone prior to administration of an inferior-alveolar nerve block should reduce the chances of entering the parotid gland. The rapid deposition of large quantities of local anaesthetic solution in the maxillary buccal sulcus may also cause temporary problems in eyelid closure. In this case the entire facial nerve has not been affected and the paralysis is more localised. Once again, the eye must be protected until motor function is restored.
Toxicity
Toxicity may be due to either the local anaesthetic or to any contained vasoconstrictor. The dose combinations found in dental local anaesthetic solutions are such that it is easier to achieve toxic levels of the anaesthetic compared with the vasoconstrictor. Idiosyncratic reactions may occur in some individuals, however, leading to toxic effects of the vasoconstrictor. If a toxic reaction occurs it is important to determine the causative agent, as the treatment differs (Table 7-1). When the effect is due to the local anaesthetic, the patient is laid flat to combat circulatory collapse. When epinephrine toxicity occurs, the patient is sat upright to reduce cerebral blood pressure. Toxicity to local anaesthesia can be the result of the following:
-
an intravascular injection
-
overdosage
-
the patient’s inability to metabolise.
| Local anaesthetic toxicity | Epinephrine toxicity |
| stop treatment | stop treatment |
| lie patient flat | place patient supine or erect |
| administer oxygen | administer oxygen if not hyperventilating |
| give intravenous fluids | reassure patient |
| give intravenous anticonvulsants | |
| basic life support |
Prevention of toxicity is better than cure. Preventive measures include:
-
aspiration before and during injection
-
calculation of safe maximum dose before treatment begins
-
slow injection.
Intravascular injection
It was mentioned above that intravenous injection could lead to systemic distribution of relatively high doses of both anaesthetic and vasoconstrictor. As all excitable tissues are susceptible to the action of local anaesthetics then unwanted effects may occur. As far as the anaesthetic agent is concerned the most susceptible organs are the brain and the heart.
Local anaesthetic toxicity of the central nervous system begins as excitation as the first effect is on inhibitory fibre activity. This presents as restlessness and tremors. Later stages of toxicity produce central nervous system depression that can lead to unconsciousness and ultimately the fatal condition of respiratory arrest (Fig 7-2).
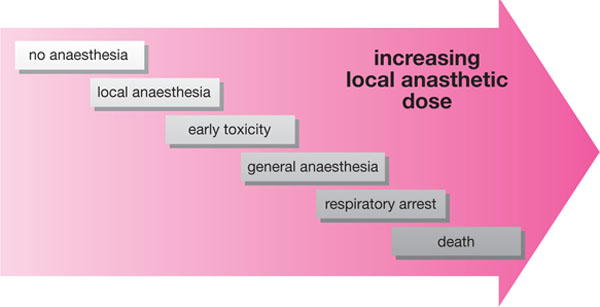
Fig 7-2 What happens when the dose of local anaesthetic increases.
There is sufficient local anaesthetic contained in a cartridge to produce toxic levels of the agent in the central nervous system in children and small adults. This is illustrated in Fig 7-3.
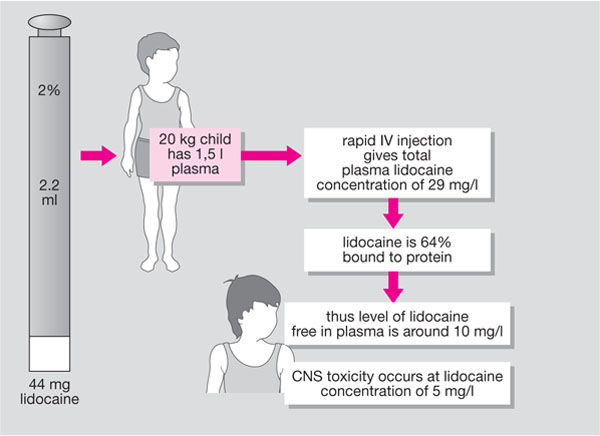
Fig 7-3 An illustration of how easy it is to overdose if a direct intravascular injection is administered in a child.
The commonly used local anaesthetics affect the heart. At low doses cardiac output may be increased owing to a disinhibition of autonomic nerve activity. At toxic doses there is a direct depressant effect resulting in circulatory collapse.
Epinephrine toxicity will induce effects similar to those experienced in fright (Table 7-2). In addition, vasoconstrictors may produce adverse effects on the cardiovascular system. Epinephrine increases cardiac output by increasing both the rate and force of contraction of the heart owing to beta1-adrenergic stimulation. This may lead to an increase in systolic blood pressure. Alpha-adrenergic stimulation causes vasoconstriction of peripheral vessels that is useful in providing haemostasis. Beta2-adrenergic stimulation causes a vasodilatation in blood vessels in other organs such as the liver and skeletal muscle. This latter effect can reduce diastolic blood pressure. In addition to direct effects on the heart and blood vessels, epinephrine produces metabolic changes that can affect cardiovascular function. One metabolic effect that can influence cardiovascular function is the effect of epinephrine on plasma potassium levels. Epinephrine reduces plasma potassium and large shifts in the concentration of this ion can lead to dysrhythmias.
| fear anxiety restlessness heada/> |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


