Chapter 7
Resective Hard Tissue Surgery
Aim
To review the factors influencing the surgical management of molar teeth with furcation involvement and to outline the resective surgical procedures available to facilitate complete and partial tooth retention as an adjunct to restorative care.
Outcome
Having read this chapter the reader should be aware of the various resective treatment approaches available for molar teeth with furcation involvement and/or combined periodontal-endodontic lesions. The reader should understand that the choice of treatment depends upon several interrelated factors.
Introduction
Loss of alveolar bone support arises as a result of inflammatory periodontal disease. Variations in the morphology of multirooted teeth are important in determining at what stage in the periodontal breakdown process a “furcation” area will become involved. A furcation is defined as the point at which the roots of a tooth divide. Furcation lesions involve bone resorption and attachment loss between the roots of multirooted teeth resulting predominantly from periodontal bone loss.
Evidence exists to suggest that molar teeth with furcation involvement have a reduced prognosis. This can be explained partly by the difficulties in obtaining proper access for instrumentation of teeth with complex furcation anatomy, but largely by a patient’s inability to effect adequate plaque control, resulting in a persistence of pathogenic microbial flora.
The treatment, management and long-term retention of molar teeth with furcation involvement is challenging. Resective and regenerative techniques have been designed to overcome the difficulties encountered in debridement and maintenance of furcation areas. Regenerative surgery has been discussed in Chapter 5, and therefore this chapter will limit discussion to resective surgical management.
Resective surgery aims to:
-
Establish a favourable anatomy at the dentogingival interface that improves patient access and is conducive to high standards of hygiene.
-
Maintain a healthy and functional tooth with acceptable aesthetics.
Furcation plasty is the reshaping of interradicular bone (osteoplasty) and/or tooth substance (odontoplasty) at the level of the furcation entrance to reestablish soft tissue morphology and allow access for cleaning.
Tunnel preparation is the surgical exposure and management of a furcation area by removal of interradicular bone and apically repositioning of the flaps to facilitate interradicular cleaning. This technique may obviate the need for endodontic treatment and prosthetic reconstruction.
Root amputation is the removal of one whole root of a multirooted tooth, leaving the crown intact. It is appropriate largely for maxillary molars.
Hemisection is the division of a tooth with removal of a root with its accompanying crown portion. This is normally appropriate for mandibular molar teeth. In some cases both halves of the tooth may be retained, leaving two separate roots which are treated as separate teeth.
Examination, diagnosis and treatment planning
Hard tissue resective therapy is a technically demanding procedure that relies upon careful case selection and interdisciplinary treatment planning to optimise success. Treatment usually includes endodontic therapy, periodontal surgery and prosthodontic reconstruction. Consideration must be given to factors such as tooth restorability, occlusal factors and the strategic value of the tooth prior to embarking upon treatment.
Improved endodontic management and the increased sophistication of periodontal surgery provide the means to consider retaining molar teeth with furcation problems that would otherwise have been lost.
The unique, complex anatomy of the root favours the development of periodontitis and bone loss in the furcation area. Important anatomical features of the furcation area include:
-
the size of the root furcation
-
root concavities
-
cervical enamel projections
-
bifurcation ridges
-
enamel pearls.
These features hamper access for routine periodontal debridement. Loss of vitality may arise because of the presence of accessory canals in the furcation area. These provide pathways that allow passage of bacteria between the pulp and periodontium, thereby creating a concomitant periodontal-endodontic lesion.
Studies that have assessed the response of teeth with furcation involvement to traditional surgical and non-surgical therapy have all reported decreased success rates compared with teeth without furcal disease.
Furcation involvement can be classified (Hamp’s Classification, 1975) according to the amount of periodontal bone loss that has occurred in the interradicular area (Fig 7-1).

Fig 7-1 Hamp’s Classification of a furcation.
Grade I: Horizontal loss of periodontal support not exceeding one third of the width of the tooth.
Grade II: Horizontal loss of periodontal support exceeding one third of the width of the tooth, but not encompassing the total width of the furcation area.
Grade III: Horizontal “through and through” destruction of the periodontal tissues in the furcation area.
The extent and the severity of periodontal bone loss is assessed by a combination of clinical and radiographic examinations. Radiographic examination should consist of periapical radiographs taken using a paralleling technique to allow comprehensive endodontic assessment and analysis of bone levels. The use of a conventional periodontal probe will allow assessment of probing pocket depth and clinical attachment loss, which are measured in a vertical dimension, but will not allow negotiation and exploration of the three-dimensional aspect of the furcation area. The presence and depth of furcations may be examined with a specific, curved furcation probe (Fig 7-2). The examination of interproximal furcations in maxillary molars and premolars can be difficult owing to problems of access.

Fig 7-2 A furcation probe (Nabers probe, Hu-Friedy).
For the majority of teeth, a conventional non-surgical approach including RSD should be employed in the first instance. If this approach is unsuccessful or inappropriate, consideration can be given to other treatment options (Box 7-1), which include resective procedures.
Box 7-1 Treatment options for molar teeth with furcation involvement
Scaling and RSD
Surgical RSD
Furcation plasty
Tunnelling procedures
Root amputation
Hemisection
Regeneration procedures
Apically repositioned flap
Extraction and prosthetic replacement
Implant placement
Indications for Root Amputation/Resection and Hemisection
-
Advanced periodontal bone loss affecting one root.
-
Grade II and Grade III furcation involvement.
-
Complex anatomy impeding oral hygiene, which would be facilitated by removal of a root.
-
Failing endodontic treatment in one root that is not amenable to retreatment or periradicular surgery. Periradicular surgery may be more difficult to perform on a posterior tooth than an anterior tooth. For this reason, the relatively simpler techniques of root amputation or hemisection may be considered.
-
Severe recession or dehiscence of bone covering a root.
-
Bone loss around a periodontal-endodontic lesion that is compromising bone support for an adjacent sound root, or an adjacent tooth (Fig 7-3).
-
Root fracture.
-
Difficult access to caries within a furcation.
-
External root resorption or root caries affecting one root.

Fig 7-3a Radiolucency and bone loss around distal root of first molar.
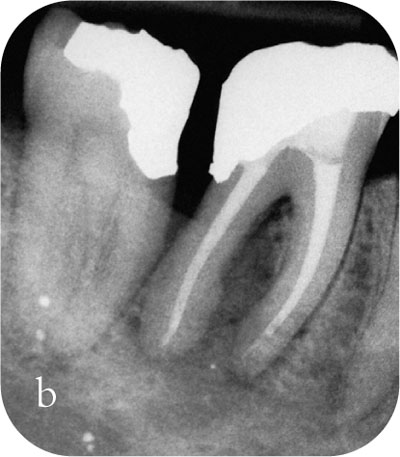
Fig 7-3b Root canal and periodontal treatment did not resolve the intrabony pathology and the bone level mesial to the LR7 was compromised.

Fig 7-3c Six months following hemisection, note the restoration of bone mesial to the lower right second permanent molar.
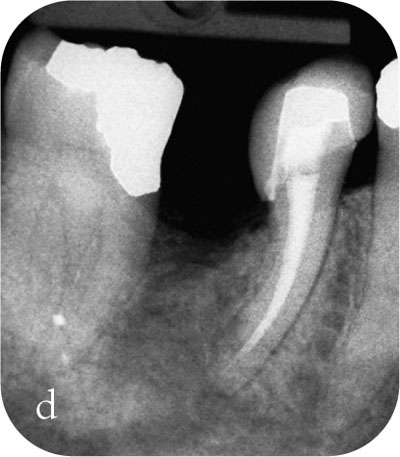
Fig 7-3d Temporary crown, lab-made to facilitate plaque control.
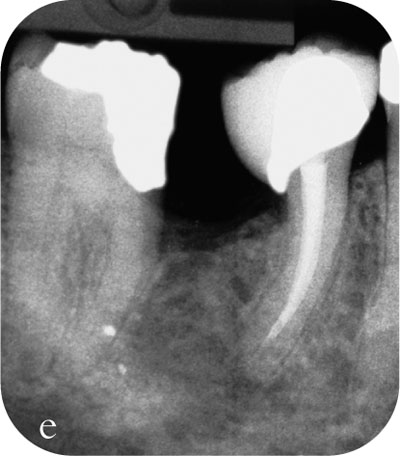
Fig 7-3e Definitive crown, made elsewhere. It is worth noting that the definitive crown has a poor design and emergence profile, compared to the temporary crown. The definitive crown had to be remade to facilitate longer-term maintenance of plaque control.
Contraindications to Resective Surgery
-
Poor oral hygiene.
-
Unwillingness of patient to undergo complex restorative and surgical treatment.
-
Poor long-term prognosis.
-
Poorly executed endodontic treatment in all roots.
-
Any medical condition that contraindicates surgery.
Assessment of Teeth for Resective Surgery
Tooth-specific Assessment
-
Endodontic assessment including the quality of pre-existing endodontic treatment.
-
The anatomy of the roots. Sufficient separation of the roots is required so that resection is possible without damaging adjacent roots. It is important to ensure that there will be enough bone remaining around the roots that are to be retained. Fused or closely approximated roots are not suitable candidates for resection/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


