Chapter 7
Pulp Therapy in the Primary Dentition
Aim
The aim of this chapter is to demonstrate the simple pulp therapy techniques that are available to treat carious primary teeth. The rationale for their use will be discussed and each clinical stage demonstrated using a step-by-step approach.
Outcome
After reading this chapter the practitioner should be confident in performing the commonly used pulp therapy techniques for primary teeth.
Introduction
Why is there such an air of mystery surrounding primary molar pulp therapy in the UK? It is one of the most straightforward and quick procedures in the dental armamentarium. It involves simple medicaments and instrumentation and benefits the child two-fold: by avoiding the trauma of extraction and by preserving the space-maintenance role of the primary dentition.
Pulp therapy for cariously exposed primary molars aims to conserve the damaged tooth and restore its function until the permanent successor erupts. Successful treatment of pulp tissue reduces the need for unplanned extractions and the undesirable consequences that may follow.
In order to understand the principles behind the currently advocated pulp therapy techniques, the response of the pulp to a carious insult shall be discussed briefly. A simple step-by-step guide to the techniques will follow this. A complete list of the instruments and medication used is available at the end of this chapter. There have been recent changes to the medicaments available for pulp therapy in primary teeth. Confirmation by the International Agency for Research on Cancer (IARC) of the carcinogenic effects of formaldehyde in humans was published in June 2004. As a result, pulp therapy techniques are undergoing a period of significant change. This chapter is representative of the trend towards the use of aldehyde-free pulp therapy techniques in the UK.
Infected and Inflamed Dental Pulp
There are several reasons for a dental pulp to become inflamed or infected, but by far the commonest is as a sequel to dental caries.
Dental caries in a primary tooth progresses rapidly though the relatively thin enamel and penetrates dentine. The insult from bacterial toxins stimulates the underlying pulp to respond by mounting an inflammatory reaction (reversible pulpitis).
If a carious exposure occurs, microbes invade the pulp tissue, causing a massive increase in pulpal response. This is characterised by irreversible inflammation and tissue necrosis directly adjacent to the site of the exposure. If this remains untreated, bacteria and their products will progress through the pulp tissue, resulting in irreversible inflammation and tissue breakdown involving the whole pulp system. The spread of inflammation is gradual and progressive through the whole pulp and then beyond into the periradicular tissues via furcational, lateral and apical communications. The response of pulpal and periodontal tissues to such injury can lead to one of several outcomes:
-
The periradicular tissues may become affected (periradicular periodontitis), with eventual involvement of associated soft tissue (Fig 7-1).
-
If the exposure site involves a large area, hyperplastic pulpitis (pulp polyp) may occur (Fig 7-2).
-
The tooth may be subject to pathological resorption – for example, internal inflammatory resorption (Fig 7-3).

Fig 7-1 A palatal abscess associated with a grossly carious primary molar.

Fig 7-2 Hyperplastic pulpitis (pulp polyp) seen in the pulp of a primary molar.
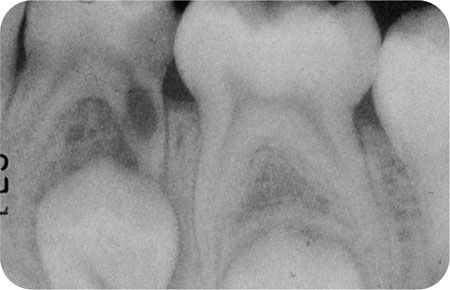
Fig 7-3 Internal inflammatory resorption affecting the distal root of a primary molar.
If vital inflamed tissue is removed, leaving residual healthy pulp, it has the capacity to remain healthy if managed correctly. Therefore, the overall success of pulp therapy in the primary dentition depends upon:
-
Effective control of infection.
-
Removal of irreversibly inflamed tissue.
-
Appropriate wound dressing.
-
Effective coronal seal during and after treatment.
When is Pulp Therapy Required?
-
An accurate pain history is helpful in deciding the probable stage of pulpal involvement, but it is often difficult to obtain such information from a child.
-
Preoperative radiographs are helpful to assess the extent of the carious lesion and its proximity to the pulp. They are also important to determine if periradicular pathology is present. Findings from radiographs can guide treatment decisions.
-
Clinically, pulpal involvement can often be assessed more easily following caries removal. In other words, after caries removal look very carefully for evidence of pulpal exposure. Blood will be present at the exposure site if the pulp tissue is still vital coronally.
-
If a carious exposure is bloodless, then some, if not all of the pulp, is likely to be necrotic.
Assessing Inflammation in a Vital Pulp
It can be difficult to assess the amount and level of inflammation within the pulp. Therefore, in vital pulp therapy it is assumed that the whole coronal pulp is “affected” and so all of the coronal pulp is amputated.
Following amputation of the coronal pulp, our attention must turn to the remaining radicular pulp stumps. The nature of the bleeding from the radicular pulp is used to assess whether inflammation has extended beyond the coronal pulp tissue and into the root canals. If haemostasis cannot be achieved, this tissue is assumed to be irreversibly inflamed and vital pulpotomy techniques are contraindicated. A tooth with persistent bleeding from the pulp stumps should be treated by pulpectomy.
Below are examples of signs and symptoms that could indicate that some form of pulp therapy is needed.
Signs
-
Occlusal caries extending more than 4mm in depth.
-
Approximal caries where 2/3 of the marginal ridge has been destroyed (Fig 7-4).
-
Caries involving or very close to the pulp horns on a radiograph (Fig 7-5).
-
Mobility or tenderness to percussion.
-
Sinus formation.
-
Periradicular bone radiolucency on a radiograph.
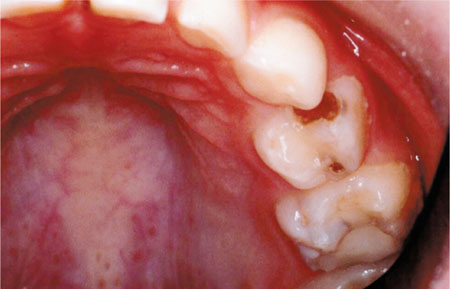
Fig 7-4 A primary molar with more than 2/3 of the marginal ridge broken down. This gives a strong indication that pulp therapy is required.

Fig 7-5 A radiographic view showing the proximity of an approximal carious lesion to the pulp.
Symptoms
-
Pain
-
transient on thermal stimuli (reversible pulpitis)
-
spontaneous and lasting in nature (irreversible pulpitis)
-
from biting on the affected tooth (periapical or intraradicular infection).
-
Indications and Contraindications for Primary Molar Pulp Therapy
Further to the signs and symptoms, additional indications for pulp therapy are:
-
Cooperative child and carers.
-
Avoidance of the psychological trauma of extraction.
-
Medical conditions where extraction should be avoided (e.g. haemophilia).
-
Absence of the permanent successor tooth.
-
To maintain an intact arch in the primary dentition.
-
Space maintenance in the mixed dentition.
There are also several important contraindications to pulp therapy, including:
-
Lack of cooperation from child or carer.
-
Medically compromised children at risk from a dental bacteraemia (e.g. immunocompromised or at risk of developing infective endocarditis).
-
Poor general condition of the mouth (e.g. greater than or equal to three teeth with likely pulpal involvement).
-
Insufficient coronal tooth tissue to ensure an effective coronal seal post-treatment.
-
Caries involving the pulp chamber or root canal.
The Root Anatomy of Primary Molar Teeth
Paediatric dentists have traditionally favoured pulpotomy as opposed to complete extirpation of the pulp (pulpectomy) because of several perceived difficulties relating to the anatomy of the primary dentition. These are reported as:
-
Ribbon shaped canals (difficult to instrument).
-
Thin walls to canals (relative increase risk of perforation).
-
Many lateral and furcal communications (difficult to clean and obturate).
-
Physiological apical root resorption (wide open apical regions).
-
Close proximity of the permanent tooth germ to the apex of primary tooth (relative risk of damaging successor tooth).
To Begin …
It is essential to provide adequate local anaesthesia before pulp treating a vital primary tooth.
Additionally, it is worth remembering that even a tooth that appears to be completely non-vital may still have vital pulp tissue remaining. Therefore, it is essential that adequate pain relief is administered to ensure the continuing comfort and cooperation of the child. Effective moisture control is also important (ideally with dental dam where possible) for caries removal and any subsequent pulp therapy. If placement of dental dam is not achieved, dry guards, cotton wool rolls and a saliva ejector must be used once the pulp chamber is breached.
Pulp Therapy Techniques
The basic pulp therapy techniques available are dependant on the extent of pulpal inflammation and as such can be broadly divided into:
-
Pulp Capping – This involves two approaches; direct and indirect. The direct pulp cap is not routinely used in the primary dentition.
-
Pulpotomy – This can be performed on vital teeth, but the technique can differ in respect of choice of medicament and the number of visits required.
-
Pulpectomy – This can be used for non-vital teeth with or without signs of infection. Complete extirpation of the pulp of a primary tooth and obturation with a resorbable material is gaining in popularity.
The common pulp therapy techniques available, the agents that can be used and the likely number of visits required are given (Figs 7-6 and 7-7). The management of a bleeding carious exposure (vital) is shown in Fig 7-6. The options for managing a carious exposure that does not bleed (non-vital) is shown in Fig 7-7.
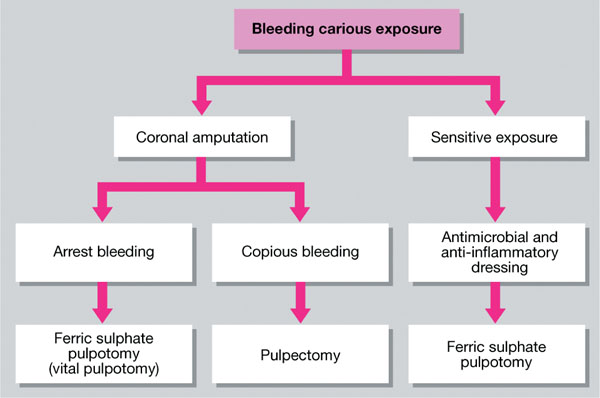
Fig 7-6 A flow diagram showing the options for treating a bleeding carious exposure in a primary tooth
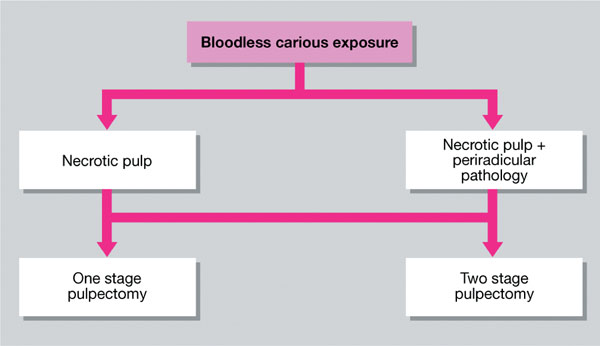
Fig 7-7 A flow diagram showing the options for treating a bloodless carious exposure in a primary tooth.
Pulp Capping
Also termed indirect pulp therapy, this is used in the primary dentition to maintain vital pulp tissue. Pulp capping in the primary dentition may be divided into two different techniques:
-
indirect
-
direct.
Indirect pulp capping in primary molars
Also termed indirect pulp therapy, this involves placing a lining onto deep, softened dentine in order to eliminate microbes and stimulate reparative secondary dentine and maintain pulp vitality. The technique is thought to be successful in pulp treatment of reversible inflammation in primary teeth with deep dentine caries.
Indirect pulp therapy technique
-
The primary tooth must be symptom-free.
-
The walls of cavity must be rendered caries-free, to permit sealing of the cavity margin.
-
Deep, softened dentine may be left at the floor of the cavity, if its removal risks pulp exposure in a symptom-free tooth.
-
There must be no evidence of pulpal exposure:
-
remove all caries from cavity walls
-
excavate cavity floor carefully
-
leave softened dentine, or thin layer of hard dentine, but do not expose the pulp
-
place a setting calcium hydroxide or a glass-ionomer cement lining over the stained or thin dentine
-
place a permanent, well-sealed restoration (compomer, preformed metal crown)
-
provide regular clinical and radiographic review.
-
Direct pulp capping in primary molars
This involves placing an agent directly onto a small traumatic pulpal exposure in order to stimulate the formation of a calcific barrier at the exposure site. This acts to protect the pulp tissue adjacent to the barrier. This approach should never be used for a carious exposure.
A direct pulp cap should only be used for pinpoint exposures caused by instrumentation. In paediatric dentistry, this may sometimes arise (although rarely) if a child unwittingly bites down on a bur during cavity preparation.
If a primary tooth has a carious exposure, the preferred method of treatment is a pulpotomy because infected and irreversibly inflamed coronal pulp should be removed. If there is a small area of contact between a calcium hydroxide direct pulp cap and an inflamed pulp, it will be ineffective, resulting in persistent inflammation, pulp death and often internal resorption. When calcium hydroxide is used as a direct pulp cap over a small exposure of healthy pulp tissue it can stimulate the deposition of a dentine barrier.
Direct pulp capping technique
-
Arrest bleeding with gentle pressure from a sterile pledget of cotton wool moistened with saline (0.9%) placed over the exposure for 1–2 minutes.
-
Bleeding must stop.
-
Gently place a thin sub-lining of setting calcium hydroxide over/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


