Pulp therapy for primary and immature permanent teeth
John Winters, Angus C Cameron and Richard P Widmer

Introduction
Dental caries, trauma and the iatrogenic effects of conservative dental treatment, all provoke a biological response in the pulpo-dentinal complex. This chapter is concerned with the cascade of therapeutic interventions used to promote an adaptive biological response in the pulpo-dentinal complex of the treated tooth, and optimize subsequent growth and development. Therapeutic efforts are directed towards the retention of carious or traumatized teeth, maintaining normal function, with the resolution of, or freedom from, clinical symptoms.
Role of primary teeth
As mentioned in the last chapter, primary teeth play an integral role in the development of the occlusion. Premature loss of a primary tooth through trauma or infection has the potential to destabilize the developing occlusion with space loss, arch collapse and premature, delayed or ectopic eruption of the permanent successor teeth. In general, the effects of early extraction of primary teeth are more profound in the buccal segments than in the anterior dentition.
Effective pulpal therapy in the primary dentition must not only stabilize the affected primary tooth, but also create a favourable environment for normal exfoliation of the primary tooth, without harm to the developing enamel or interference with the normal eruption of its permanent successor. Where these outcomes cannot reasonably be achieved over the clinical life of the primary tooth, it is appropriate to extract the affected tooth and consider alternative strategies for occlusal guidance and maintenance of arch integrity (see Chapter 14).
Immature permanent teeth
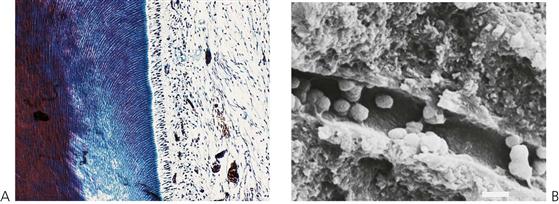
All teeth are immature when they erupt. In addition to the important phase of post-eruptive enamel maturation, the roots of newly erupted permanent teeth will take up to 3 years before their growth is completed. During this period, the roots are short, the root apices are wide open, the dentine is relatively thin and the dentine tubules are relatively wide, increasing the permeability of dentine to bacteria. The open apex is associated with excellent pulpal vascularity and the potential for a favourable healing response.
Therapeutic efforts are directed towards preserving the vitality of the pulpo-dentinal complex to facilitate normal root development and maturation (Figure 7.1). If pulp necrosis occurs prior to root maturation, while the affected tooth can still be preserved using non-vital endodontic strategies, it will be compromised with regard to strength, root length and apical development. It is important to consider whether the tooth itself is actually restorable in the long term. Retention of a compromised immature permanent tooth with a poor long-term prognosis may still be beneficial for arch integrity and normal alveolar development during the period of dentofacial growth (see Chapter 14).
Evidence for current practice
The current evidence base for pulp therapy in the primary dentition is poor with a demonstrated paucity of prospective randomized controlled trials. The single biggest issue surrounding pulp therapy in the primary dentition is the lack of correlation between clinical symptoms and pulpal status. Hence, at present, there is no single recognized technique for pulp treatment in primary teeth, and a range of different protocols and medicaments are suggested for different combinations of symptoms and clinical findings.
The information in this chapter is based on established clinical practice, retrospective descriptive studies, clinical experience and expert opinion. In general, it is appropriate to use the least invasive intervention that is predictably associated with a healthy, adaptive healing response in the affected primary or permanent tooth. Obviously, effective primary prevention and early intervention will obviate the need for many of the procedures and techniques described later in this chapter.
Clinical assessment and general considerations
Diagnosis of pulpal status
Effective pulpal therapy requires the correct assessment and interpretation of clinical signs and symptoms, leading to an accurate diagnosis of the pulpal condition. Ineffective or inappropriate pulp therapy is associated with both acute and chronic clinical signs and symptoms. Unfortunately, there are no objective or definitive tests to determine the health of the pulpo-dentinal complex in the primary or immature permanent tooth. Clinical signs and symptoms are poorly correlated with actual pulp histology.
Acute signs and symptoms include:
• Pain.
• Periapical or intra-radicular abscess.
• Facial cellulitis, including spread of infection into the tissue planes around the airway (Ludwig’s angina, see Chapter 10).
Chronic signs and symptoms include:
Pulp sensibility tests
Standard techniques of pulp sensibility testing are of limited value in children. These techniques rely on patient feedback in response to thermal and electrical stimulation. In the primary dentition, it is likely that children will not have achieved the cognitive development necessary to respond reliably to a potentially painful stimulus and response challenge. In the immature permanent tooth, raised response thresholds to electrical stimuli are observed. These decrease to normal levels with root maturation and apical closure.
Pain (Figure 7.3)
Young patients frequently have difficulty communicating their experience of pain. It is often not until their pain is severe and prolonged that parents might become aware of and seek treatment for their child. Symptoms of severe, prolonged, spontaneous or nocturnal pain suggest irreversible pulpitis or a dental abscess (Figure 7.3B). A history of repeated need for analgesics is also suggestive of pulp necrosis. Dental pain will frequently resolve once a sinus tract establishes drainage, and thus relieves pressure. In these cases, the underlying pathology is still present and must be resolved, despite the lack of obvious discomfort. Chronic infection in the primary dentition can cause disturbances to enamel formation in the permanent dentition (Turner tooth, see Chapter 11) and malocclusion (Fig 7.2B) even in the absence of clinical symptoms or pain.
Other clinical signs
Careful clinical examination of teeth can reveal useful diagnostic information.
• Coronal discoloration is suggestive of pulp necrosis.
• Clinical mobility is associated with loss of bone from infection or imminent exfoliation.
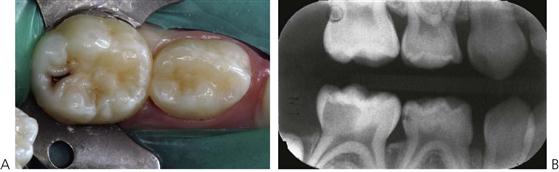
• Marginal ridge fracture in a primary tooth is suggestive of carious pulpal involvement in contact point caries (Figure 7.4A).
• Fracture of the occlusal triangular ridges or carious undermining of the cusps in pit and fissure caries also suggests carious involvement (Figure 7.4B).
Unfortunately, the external appearance of the carious lesion can in some cases, be misleading (Figure 7.5). Persistent symptoms occurring soon after placement of a restoration indicate pulpal pathology. Lack of coronal seal will inevitably lead to pulpal pathology. Radiographic examination is essential to supplement clinical findings and enhance diagnostic accuracy.
Radiographs
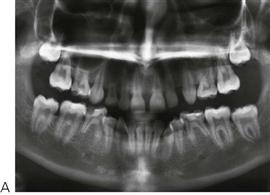
Longitudinal radiographs showing normal dentine deposition within the pulp chamber and the roots suggests pulpal health. Irregular pulp calcification or pulpal obliteration suggests pulpal dystrophy, while failure of physiological pulp regression or arrested root development suggests pulpal necrosis. In a single radiographic examination, individual teeth can be compared with their antimere to identify asymmetry.
Clinical signs or symptoms suggesting carious involvement of the pulp require radiographic investigation. Radiographs will show the extent of the carious lesion, the position and proximity of pulp horns, the presence and position of the permanent successor, the status of the roots and of their surrounding bone. Radiographic examination should be considered essential before undertaking endodontic procedures. The presence of caries in the furcation, internal or external root resorption including physiological root resorption, and periapical or furcation bone lesions, are all contraindications to endodontic treatment in the primary dentition.
Primary teeth with these radiographic signs should be extracted.
Swelling
Alveolar swelling, particularly involving the vestibular reflection, facial swelling, coronal discoloration, and the presence of a sinus, are indicators of pulp necrosis and abscess formation (see Figure 7.3B).
Mobility
Inappropriate tooth mobility, tenderness to palpation or a sensation of occlusal interference also suggests abscess formation.
Antibiotic usage to control acute infection (see Odontogenic infection, Chapter 10) may temporarily resolve some or all of these clinical signs, but will not resolve the underlying pathology. A primary tooth that cannot be saved requires extraction despite potential future orthodontic complications.
Factors in treatment planning
Medical history
A thorough medical assessment is essential prior to the commencement of any dental treatment. Medical issues may limit or change treatment options in a number of ways. As pulp therapy necessarily relies on the adaptive healing response after treatment, so patients with a significantly compromised immune system are considered poor candidates for endodontic therapy.
Contraindications
• Congenital cardiac disease (see Appendix E). Patients who are considered to be at risk of bacterial endocarditis should be free of oral infection and any primary tooth with clinical signs of infection should be extracted. There is no evidence to suggest that a primary tooth with a large restoration is more or less likely to become infected if it has undergone endodontic treatment according to established guidelines.
• Immunosuppressed patients and those with poor healing potential (see Immunodeficiency, Chapter 12).
Generally, children with well-managed diabetes present no particular problem in relation to healing potential. The use of long-term corticosteroids for the management of asthma, or asthma, should not affect the decision to retain primary teeth. However, children who are severely immunosuppressed, such as oncology patients, must be treated more aggressively (e.g. extractions).
Indications
• Bleeding disorders and coagulopathies (see Chapter 12). Current management protocols for patients with a bleeding diathesis (such as haemophilia) may use regular, often home-based, factor replacement. Where patients have access to such medical treatment, the decision to extract or retain a pulpally involved primary tooth should not be determined by the bleeding diathesis, but should be based on the same criteria used for any other patient. Consultation with the child’s haematologist is essential.
• Hypodontia (i.e. ectodermal dysplasia, Figure 7.6A; see also Chapter 11). In cases of congenital absence of teeth, the decision to extract or retain individual teeth will be influenced by the overall orthodontic strategy. In some cases, there is a requirement to extract primary teeth early to encourage occlusal drift and space closure. In these cases, timing of extractions can be critical, necessitating an interim restoration of the affected primary tooth. In other cases, it is necessary to maintain a primary tooth without a successor. In the absence of acute symptoms, a formal orthodontic evaluation should be considered.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses