Dental anomalies
Michael J Aldred, Angus C Cameron, Nigel M King and Richard P Widmer

Introduction
The diagnosis and management of dental anomalies constitute important areas of paediatric dentistry. Although most dental anomalies present in childhood, many are misdiagnosed or left untreated, perhaps because of lack of experience or because the case is perceived to be ‘too difficult’. In some instances, genetic consultation is desirable, not merely to diagnose the condition but also to provide appropriate advice on the prognosis and the risk of recurrence in future generations. In many cases, the presence of an inherited dental disorder in one child would not stop a family from having additional children, but it is important to give parents and the affected children themselves appropriate information on which to base their decisions. Genetic services are usually available at most paediatric hospitals.
In this chapter, reference to particular inherited conditions is made to entries in OMIM (Online Mendelian Inheritance in Man). This online database is a catalogue of genetic disorders developed by Dr Victor McKusick of the Johns Hopkins University and the National Center for Biotechnology Information (see References and further reading, below).
Considerations in the management of dental anomalies
• Informing and supporting the child and parent.
• Interdisciplinary formulation of a definitive treatment plan.
• Provision of adequate function.
• Maintenance of occlusal vertical dimension.
• Use of intermediate restorations in childhood and adolescence.
Treatment planning for children with dental anomalies
Treatment planning should be multidisciplinary. Decision-making must involve the child and the parents and should consider the present and future needs and development of the child. Although children will cope with a range of appliances and treatments during childhood, early adolescence represents a period of social adjustment, as well as the transitional changes in the dentition. It is perhaps the most difficult time in which to formulate a long-term plan. Teenagers are most concerned about aesthetics, yet it may be too early to provide definitive restorations; extensive orthodontic treatment may be required or later orthognathic surgery. In institutions, various teams exist to treatment plan and/or manage these cases and a list is suggested below. Note the involvement of the child’s local general dental practitioner.
The team approach
• Surgeon.
It is essential to seek advice from colleagues in the management of children with uncommon dental conditions. Local and international collaboration provides the best opportunities to increase our knowledge and improve the outcomes for these children.
Dental anomalies at different stages of dental development
It is convenient to consider dental anomalies by the development stage at which they arise.
Migration of neural crest cells (ectomesenchyme) into branchial arches
Dental lamina formation stage
Induction and proliferation
Histodifferentiation
Morphodifferentiation
Matrix deposition
Organic matrix deposition and mineralization
Eruption and root development
Formation of dental lamina
Hypodontia
Alternative terminology: Hypodontia, oligodontia, anodontia.
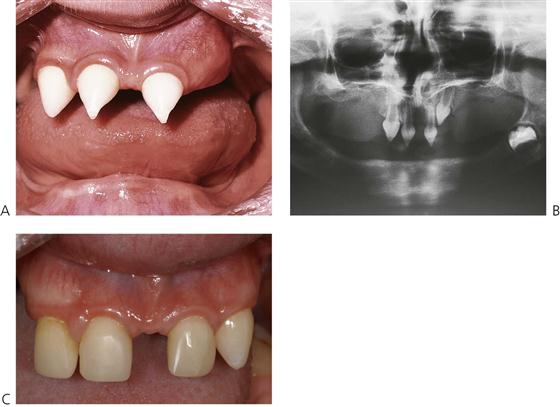
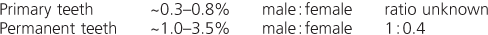
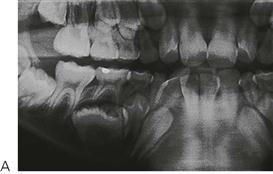
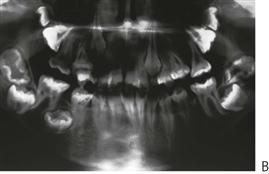
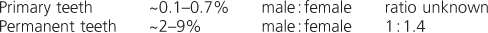
Hypodontia, oligodontia and anodontia are terms that can be interpreted to refer to progressive degrees of missing teeth, though the term hypodontia is preferred because it is inclusive of any number of missing teeth (Figure 11.1A). ‘Oligodontia’ refers to six or more missing teeth, and ‘anodontia’ to the complete absence of teeth. It is implicit in all cases that the teeth are missing because of failure of development. The term ‘congenitally missing teeth’ is a misnomer when applied to the permanent dentition because these teeth do not commence development until after birth (and with regard to the primary dentition one cannot usually determine this clinically at birth); ‘partial anodontia’ is a nonsense term. Some degree of hypodontia is not uncommon, occurring sporadically or with a hereditary component. The teeth most commonly absent are the last teeth in each series (i.e. the lateral incisor, the second premolar and the third molar). Clinically, it is less important to know how many, but rather which types of tooth are absent. It is particularly unusual for a patient to be missing central incisors, canines or first permanent molars. Multiple missing teeth in a child should lead to investigations to determine if there are other affected family members. The presence of a rudimentary or conical tooth may be associated with the absence of the same tooth on the opposite side of the arch. A common example of this is the peg lateral incisor. Furthermore, that lateral incisor itself may be absent in subsequent generations. Missing teeth are also a manifestation of many syndromes of the head and neck.
Frequency
Third molars > maxillary lateral incisors > second premolars > mandibular central incisors.
Major conditions manifesting hypodontia
Hypodontia is a major clinical feature of over 50 syndromes. These include:
Ectodermal dysplasias
Ectodermal dysplasia describes a group of developmental, often inherited, disorders involving the ectodermally derived structures, i.e. the hair, teeth, nails, skin and sweat glands. The most common is the X-linked hypohidrotic form (OMIM 305100, EDA1, Xq12-q13.1; short arm of X chromosome). In this condition the usual presentation is a male child with:
Teeth are small and conical, often with a large anterior diastema (Figure 11.4). Heterozygous females are often identified by dental examination and their manifestations may be limited to a single missing tooth or to a peg lateral incisor (see the Lyon hypothesis, below).
In the group of ectodermal dysplasias, autosomal dominant and recessive modes of inheritance are also seen. In such families, there will not be such a striking difference in the degree of the disorder between males and females compared with X-linked hypohidrotic ectodermal dysplasia (Figures 11.2A, 11.3). Mutations in the MSX1 gene (4p16.1) have been identified in families with missing third molars and second premolars with or without clefting, as well as in families with tooth-nail (Witkop) syndrome. PAX9 (14q12–q13) gene mutations have been found in other families with autosomal dominant missing teeth. More genes implicated in missing teeth and other anomalies continue to be identified.
In some countries, dental care (including prevention, orthodontics and prosthetics) for affected children may be provided under government-funded schemes.
Management
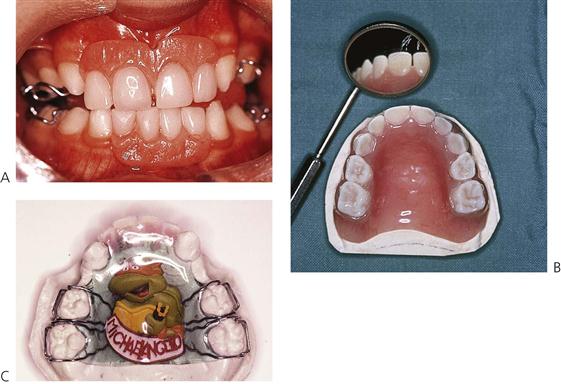
The aim of treatment is to provide adequate function, maintain the vertical dimension and restore aesthetic appearance. Ideally, for social reasons, treatment should begin at around 2–3 years of age. A first step is often the placement of composite restorations to mask the ‘fang-like’ appearance of the caniniform anterior teeth (Figure 11.4A). There is often considerable parental pressure to ‘normalize’ the appearance and later, steps may involve the provision of dentures to reduce the likelihood of teasing, often at about the time that the child starts school. This can begin as soon as the child allows adequate impressions to be taken. Often, however, the first denture is initially worn in the pocket(!), but as the child grows, there is often a desire to have a more ordinary appearance. With encouragement and positive reinforcement, most children will soon try their new appliances.
Treatment planning for children with hypodontia
Treatment planning should be multidisciplinary and should consider the present and future needs and development of the child, while being cognizant of the concerns of the individual and parents.
Treatment options
• Acid-etch retained, composite resin build-ups of conical teeth (Figure 11.6).
• Partial dentures: conventional or overdentures (Figure 11.7).
• Surgical exposure of impacted teeth.
• Orthodontic management of spaces.
• Laboratory-fabricated composite resin veneers, crowns and bridges.
• Osseointegrated implants (usually after the cessation of growth).
The Lyon hypothesis (X chromosome inactivation)
During cellular differentiation, one of the two X chromosomes in each female somatic cell is inactivated. This means that in families with X-linked disorders, approximately 50% of the cells of heterozygous females will express the mutant gene disorder, whereas the remainder will express the normal gene. In the tissues affected by the condition, such females have a mosaic of affected and normal cells. This is of particular importance in X-linked forms of conditions such as haemophilia, hypohidrotic ectodermal dysplasia, vitamin D-resistant rickets and amelogenesis imperfecta. Thus, heterozygous females with X-linked hypohidrotic ectodermal dysplasia may have missing teeth, although they are invariably less severely affected than males. Similarly, in haemophilia A, heterozygous females do not usually have a clinical bleeding abnormality but this can occur if lyonization is severely skewed so that there is a preponderance of cells producing factor VIII under control of the mutant gene.
Dentoalveolar clefting
In patients affected by dentoalveolar clefting, disruption of the dental lamina at that site, there may be abnormal cellular induction or proliferation. This may give rise to either missing teeth, usually the maxillary lateral incisor, and/or supernumerary teeth adjacent to the cleft. However, it is extremely rare for the canine tooth to be affected in the same way.
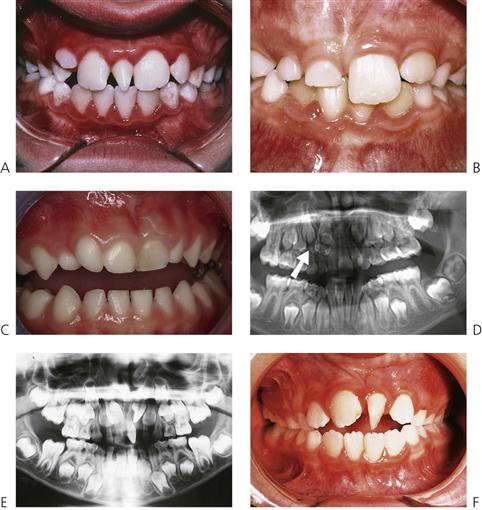
Solitary median maxillary central incisor syndrome (OMIM 147250)
Solitary median maxillary central incisor syndrome (SMMCI) (Figure 11.8) is very rare. It presents with a midline symmetrical maxillary central incisor. The condition may also be associated with other midline disturbances such as cleft palate, choanal stenosis or atresia, imperforate anus or umbilical hernia and is probably part of the spectrum of the holoprosencephaly malformation complex. Of importance in some cases is the association with hypoplasia of the sella turcica, pituitary dysfunction, growth hormone deficiency and subsequent short stature. The syndrome is usually diagnosed on the basis of the dental manifestations. A mutation in the SHH gene (7q36) has been identified in one family but it is probable that there is genetic heterogeneity in the condition.
Ultimately, management of the dental anomaly is by orthodontic and prosthodontic therapy, determined by space considerations. In most cases, the single central incisor is moved to one side of the midline with either creation of space for a prosthodontic replacement, or the adjacent lateral incisors are recontoured.
Osseointegrated implants in children
There has been much controversy about the timing of placement of osseointegrated implants in young children. To date, there has been only limited published material about early placement and any long-term consequences. It is generally understood that implants act similarly to ankylosed teeth and do not move occlusally with the growing bone around adjacent natural teeth. Recent animal research has confirmed that most fixtures do become osseointegrated in growing jaws; however, there was no evidence from this research that the fixtures behaved like normal teeth during development. In the mandible, the fixtures came to lie lingual to the natural teeth; in the maxilla, they came to lie palatal and superior to the adjacent teeth and did not follow the normal downwards and forwards growth of this bone. This latter point is important when considering the placement of implants in the anterior maxilla. Furthermore, placement of fixtures retarded alveolar growth locally and changed the eruptive path of distally positioned tooth buds. Implants should, in most cases, not be considered before the cessation of growth. It should be noted, however, that in children with conditions such as ectodermal dysplasia, alveolar bone does not develop where teeth are not present. Consequently, it may be considered appropriate, particularly where there are multiple missing teeth, to place implants much earlier in these children than in those with a normal alveolus. Recent research suggests that in cases of anodontia, implants are best placed in the mandibular canine region at around 8–10 years of age (which is after the period of maximal mandibular transverse growth) to facilitate lower denture construction.
Disorders of proliferation
Supernumerary teeth (Figure 11.9)
• Supernumerary teeth have been considered to be manifestations of a separate dentition (occurring between the primary and permanent dentitions), and consequently it may be possible to predict when and where supernumeraries may form (Jensen & Kreiborg 1990).
Alternative terminology
Mesiodens (a term restricted to supernumerary teeth in the midline of the maxilla), paramolar, distomolar, hyperdontia, polydontism, supplemental teeth.
Diagnosis
Management
• Conical teeth often erupt and are easily extracted (Figure 11.9A).
• Tuberculate and/or inverted conical teeth require surgical removal ((Figure 11.9D)) as early as possible to allow uninhibited eruption of the permanent teeth.
• Digital imaging techniques using cone-beam tomography (CBCT) provide high definition, 3-dimensional imaging of the head and neck with much reduced radiation exposure than traditional computed tomography (CT) (see Figure 11.19, below).
• During surgical removal, care should be taken to avoid disturbing the developing permanent teeth.
• After 10 years of age, or if the central incisor is malaligned: surgical exposure with or without bonding of orthodontic brackets or chains and subsequent traction may be required (Figure 11.11).
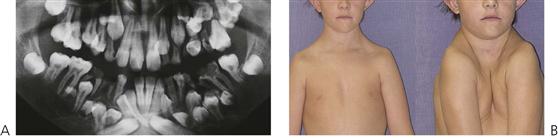
Cleidocranial dysplasia (Figure 11.10) (OMIM 119600)
This condition has an autosomal dominant mode of inheritance, with a high frequency of spontaneous mutations. The condition has been mapped to 6p21 with mutations found in the CBFA1 gene.
Manifestations
Management
• Early diagnosis and documentation.
• Planned removal of non-resorbing primary teeth.
• Surgical removal of supernumerary teeth.
• Surgical exposure of permanent teeth.
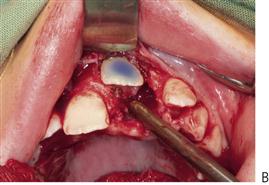
• Orthodontic alignment and consideration of orthognathic surgery when growth complete.
Note that the simple extraction of a primary tooth will frequently guarantee the eruption of the impacted permanent tooth. A two-stage surgical procedure is usually required with an attachment placed on the permanent tooth followed by orthodontic traction. The first procedure involves exposure of the anterior segments with removal of the anterior primary teeth and any supernumeraries that may be present. The permanent teeth are surgically exposed, either with primary apically repositioned flaps or with bonded gold chains attached for orthodontic traction. The anterior teeth are then aligned orthodontically. The second stage involves extraction of the primary molars, surgical removal of remaining supernumerary teeth and exposure of the premolars and molars in the buccal segments. Definitive orthodontic therapy follows; orthognathic surgery may be required in cases with severe skeletal Class III malocclusion. Treatment obviously extends over many years and clinicians should be aware of the potential problems relating to the child’s compliance and the need for multiple surgical procedures.
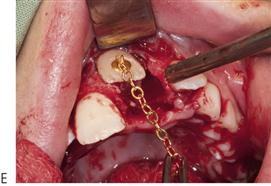
Cherubism (OMIM 118400)
Cherubism is an autosomal dominant condition caused by mutations in the SH3BP2 gene at 4p16.3.
Patients may present in childhood with facial swelling and/or failure of eruption of teeth, typically the mandibular molars. Radiographs will reveal multilocular radiolucencies, typically involving the angles of the mandible (Figure 11.12). A biopsy will reveal multinucleate giant cells in a fibrous tissue stroma. Developing teeth in the affected area tend to be displaced and fail to erupt at the normal time. The maxillae can also be affected, as can the ribs. The facial swelling reflects the involvement of the underlying bone. In some patients the sclera in the lower part of the eyes may be exposed to give the cherubic or heavenward gaze that gives the condition its name. In some cases, there is no discernible facial swelling and the condition is identified as a result of routine radiographic studies such as for orthodontic treatment planning, or because of delayed eruption of teeth.
The condition progresses into adolescence and then tends to resolve, so that by the 3rd or 4th decade radiographic changes may no longer be found. In some families more affected males than females may be identified – this is a result of reduced penetrance in females and needs to be taken into account in genetic counselling. A subset of patients with cherubism is more severely affected with the multilocular radiolucencies affecting the whole of the mandible and maxillae. In mildly affected cases regular review may be all that is necessary, in more severely affected cases surgical reduction may be considered if the patient is distressed by their appearance.
Inflammatory follicular cysts
Some children may present with failure of eruption of a mandibular premolar associated with a radiolucency involving the roots of the primary molar and crown of the unerupted premolar (see Figure 7.2B and Figure 10.27). There is controversy as to whether such cases are due to radicular cyst formation associated with the roots of the primary tooth (which is considered by some to be a rare occurrence) or dentigerous cyst formation around the crown of the premolar. The common characteristics of such cases tend to be:
• Prior endodontic treatment of the primary molar.
• A radiolucency involving the roots of the primary molar and crown of the permanent successor.
• Displacement of the permanent successor away from the alveolar crest.
Histopathological examination tends to show intense acute and chronic inflammation of the curetted tissue which is lined by hyperplastic stratified squamous epithelium. Such cases have been designated ‘inflammatory follicular cysts’, with persistent inflammation from the endodontically treated primary molar leading to an inflammatory enlargement of the follicle of the underlying permanent tooth.
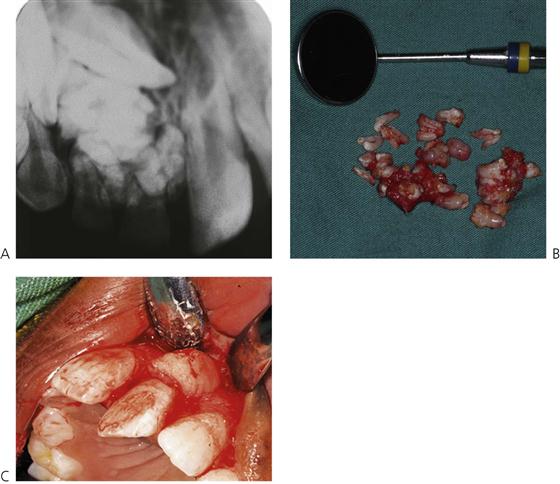
Odontomes (Figure 11.13)
Odontomes occur because of disordered differentiation and often present because of failure of eruption of a permanent tooth. In compound odontomes, multiplex of irregular denticles are found in a circumscribed soft-tissue stroma. Complex odontomes are disordered lesions with a discrete, haphazard mass of calcified tissue containing all dental elements. There is either a normal complement of teeth or the odontome replaces a tooth of the normal series.
Odontogenic tumours (see Chapter 10)
The ameloblastic fibroma, fibrodentinoma and fibro-odontome are uncommon benign odontogenic mixed tumours. All are seen as altered differentiation of the tooth bud: in an ameloblastic fibroma no hard tissue is formed, in an ameloblastic fibrodentinoma only dentine-like tissue is recognizable and in an ameloblastic fibro-odontome enamel is also formed. The lesions tend to be well demarcated.
Management
Odontogenic keratocysts (see Chapter 10)
Odontogenic keratocysts may arise in place of a tooth of the normal series or from the dental lamina in addition to a normal complement of teeth. They constitute 5–15% of odontogenic cysts.
Regional odontodysplasia (Figure 11.14)
Regional odontodysplasia is a sporadic defect in tooth formation with segmental involvement, usually localized to one, or part of one quadrant, but it may cross the midline to affect the contralateral central incisor. All dental tissues are involved in a bizarre dysplasia with hypoplastic teeth which are slow to erupt and which typically radiographically show a ghost-like appearance. The aetiology of the condition is unclear.
• Usually presents initially with abscessed primary teeth before or soon after eruption.
• Some cases are associated with superficial vascular anomalies.
Alternative terminology
Ghost teeth.
Abnormalities of morphology
Macrodontia (Figure 11.16)
Aetiology
• May also be associated with hemifacial hyperplasia.
• Generalized macrodontia is also associated with KBG syndrome (the initials are taken from the surnames of the families first reported with the condition). These children present with short stature, intellectual disability, skeletal abnormalities, syndactyly, a broad face with microcephaly and other facial anomalies (Figure 11.16B).
Alternative terminology
Megadontia, megalodontia and gigantism.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses