7 PRINCIPLES OF TOOTH PREPARATION
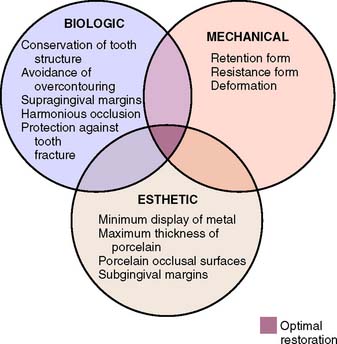
The principles of tooth preparation may be divided into three broad categories:
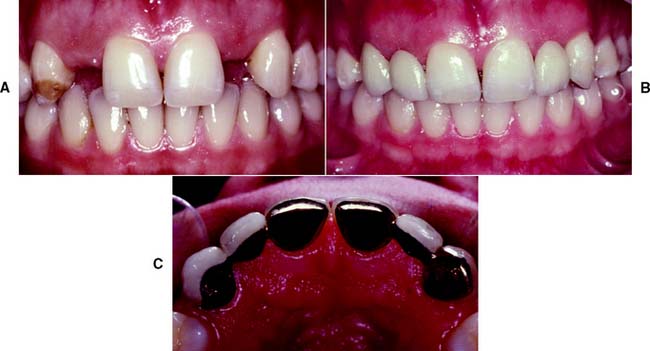
Successful tooth preparation and subsequent restoration depend on simultaneous consideration of all these factors. Improvement in one area often adversely affects another area, and striving for perfection in one may lead to failure in another. For example, in the fabrication of a metal-ceramic crown (see Chapter 24), sufficient thickness of porcelain is necessary for a lifelike appearance. However, if too much tooth structure is removed to accommodate a greater thickness of porcelain for esthetic reasons, the pulpal tissue may be traumatized (biologic consideration) and the tooth unduly weakened (mechanical consideration). In-depth knowledge and an understanding of the various criteria are prerequisite to the development of satisfactory tooth preparation skills. Predictable accomplishment of optimum tooth preparation (Fig. 7-1) often includes finding the best combination of compromises among the applicable biologic, mechanical, and esthetic considerations.
BIOLOGIC CONSIDERATIONS
Prevention of Damage during Tooth Preparation
Adjacent teeth
Iatrogenic damage to an adjacent tooth is a common error in dentistry. Even if a damaged proximal contact area is carefully reshaped and polished, it is more susceptible to dental caries than was the original undamaged tooth surface. This is presumably because the original surface enamel contains higher fluoride concentrations and the interrupted layer is more prone to plaque retention.1 The technique of tooth preparation must avoid and prevent damage to the adjacent tooth surfaces.
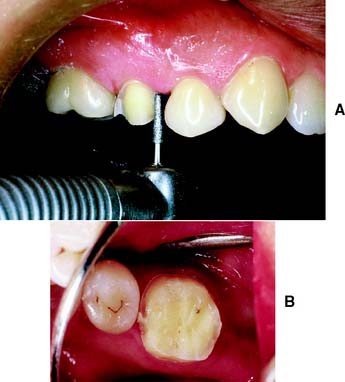
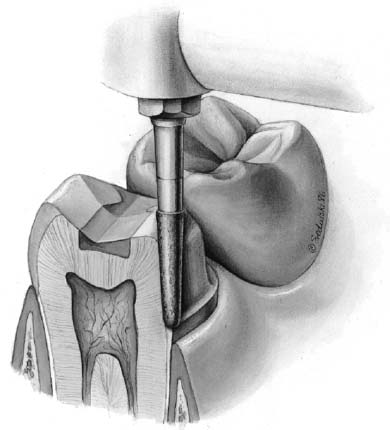
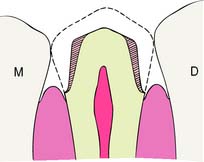
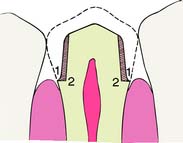
A metal matrix band around the adjacent tooth for protection may be helpful; however, the thin band can nonetheless be perforated and the underlying enamel damaged. The preferred method is to use the proximal enamel of the tooth that is being prepared for protection of the adjacent structures. Teeth are 1.5 to 2 mm wider at the contact area than at the cementoenamel junction. Therefore, a thin, tapered diamond can be passed through the interproximal contact area (Fig. 7-2) to leave a slight lip or fin of enamel without resulting in excessive tooth reduction or necessitating undesirable angulation of the rotary instrument. The latter situation, tipping the diamond unnecessarily away from the adjacent proximal surface, is a common clinical error.
Soft tissues
Damage to the soft tissues of the tongue and cheeks can be prevented by careful retraction with an aspirator tip, mouth mirror (Fig. 7-3), or flanged saliva ejector. Great care is needed to protect the tongue when the lingual surfaces of mandibular molars are being prepared.
Pulp
Great care also is needed to prevent pulpal injuries during fixed prosthodontic procedures, especially complete crown preparation. Pulpal degeneration that occurs many years after tooth preparation has been documented.2 Extreme temperatures, chemical irritation, or microorganisms can cause an irreversible pulpitis,3 particularly when they occur on freshly sectioned dentinal tubules. Prevention of pulpal damage necessitates selection of techniques and materials that reduce the risk of damage while tooth structure is prepared.4
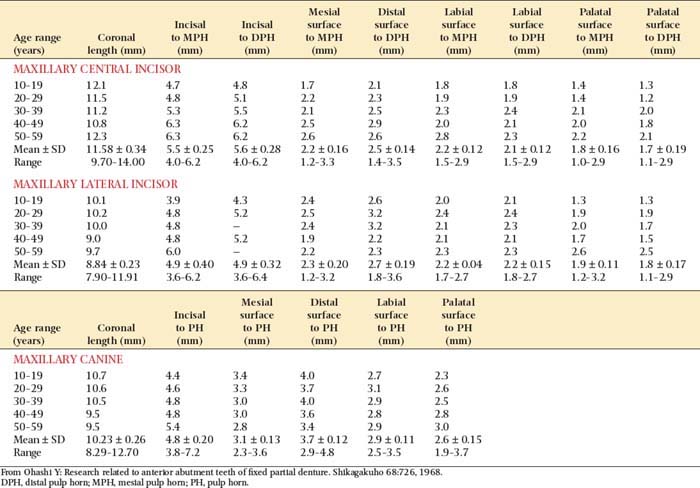
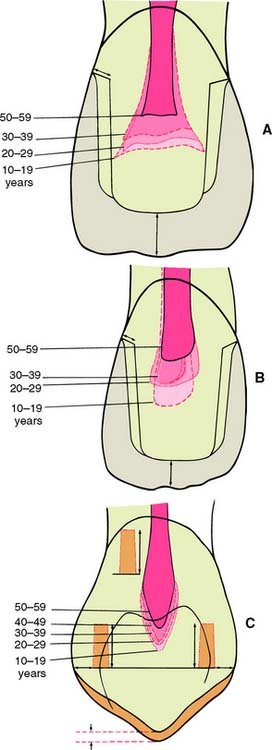
Tooth preparations must account for the structure of the dental pulp chamber. Pulp size, which can be evaluated on a radiograph, decreases with age. Up to about age 50, it decreases more so occlusocervically than faciolingually. Average pulp dimensions have been related to coronal contour5 and are presented in Table 7-1 and Figure 7-4.
Causes of injury
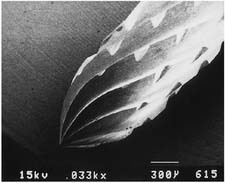
Temperature
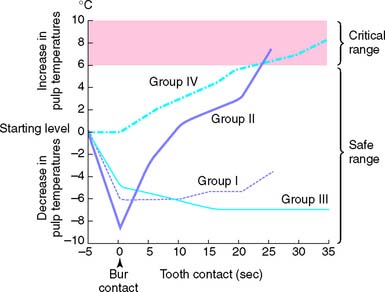
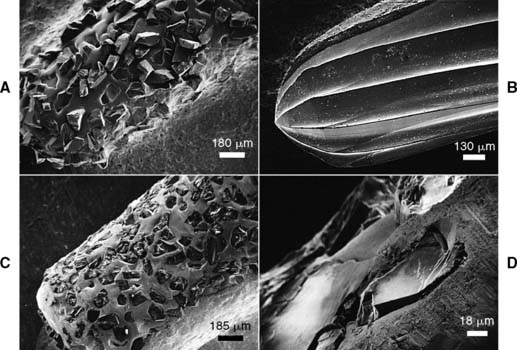
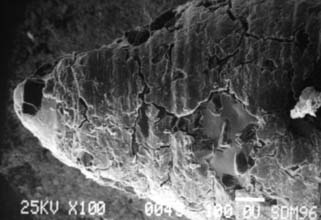
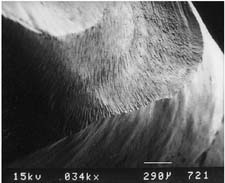
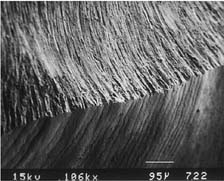
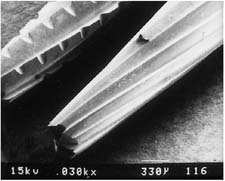
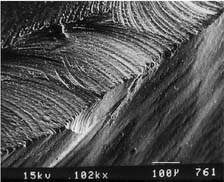
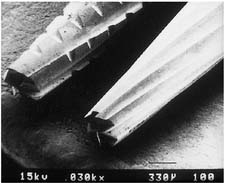
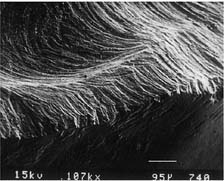
Considerable heat is generated by friction between a rotary instrument and the surface being prepared (Fig. 7-5). Excessive pressure, higher rotational speeds, and the type, shape, and condition of the cutting instrument (Fig. 7-6) may all increase generated heat.6 With a high-speed handpiece, a feather-light touch allows efficient removal of tooth material with minimal heat generation. Nevertheless, even with the lightest touch, the tooth overheats unless a water spray is used. This must be accurately directed at the area of contact between tooth and bur. The spray also removes debris—which is important because clogging reduces cutting efficiency (Fig. 7-7)—and prevents desiccation of the dentin (a cause of severe pulpal irritation).2,7 Debris accumulation has been shown to vary with rotary instrument shape. Shoulder- and chamfer-shaped diamonds may accumulate less debris. Debris is not readily removed after 5 minutes of ultrasonic cleaning.8
If the spray prevents adequate visibility, as may be the case when a lingual margin is being finished, a slow-speed handpiece or hand instrumentation should be used. Relying on air cooling with a high-speed handpiece is hazardous, because it can easily overheat a tooth and damage the pulp.9
Chemical action
The chemical action of certain dental materials (bases, restorative resins, solvents, and luting agents) can cause pulpal damage,10 particularly when they are applied to freshly cut dentin. Cavity varnish or dentin bonding agents form an effective barrier in most instances, but their effect on the retention of a cemented restoration is controversial.11–13
Chemical agents are sometimes used for cleaning and degreasing tooth preparations. However, they have been shown14 to be pulpal irritants. Thus, their use is generally contraindicated, particularly because they do not improve the retention of cemented restorations.15
Bacterial action
Pulpal damage under restorations has been attributed16,17 to bacteria that either were left behind or gained access to the dentin because of microleakage. However, many dental materials, including zinc phosphate cement, have an antibacterial effect.18 Because vital dentin seems to resist infection,19 the routine use of antimicrobial agents may not be advantageous. Many dentists now use an antimicrobial agent, such as chlorhexidine gluconate disinfecting solution (Consepsis*), after tooth preparation and before cementation, although the benefit has not been documented in clinical trials.20
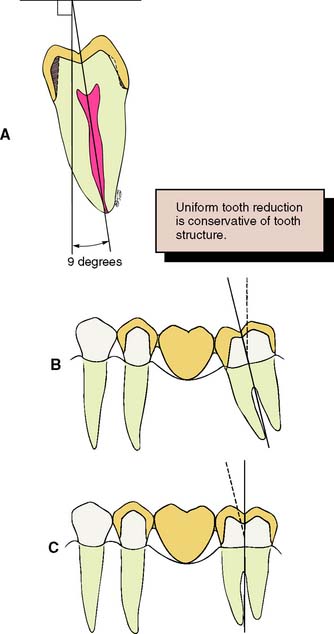
Conservation of Tooth Structure
One of the basic tenets of restorative dentistry is to conserve as much tooth structure as possible while preparation design remains consistent with the mechanical and esthetic principles of tooth preparation. Tissue preservation reduces the harmful pulpal effects of the various procedures and materials used. The thickness of remaining dentin has been shown21 to be inversely proportional to the pulpal response, and tooth preparations extending in close proximity to the pulp should be avoided. Dowden22 argued that any damage to the odontoblastic processes would adversely affect the cell nucleus at the dentin-pulp interface, no matter how far from the nucleus it occurred. For this reason, in the assessment of likely adverse pulpal response, the amount of removed dentin is important; particular care must be exercised when vital teeth are prepared for complete-coverage restorations (Fig. 7-8).
Tooth structure is conserved through adherence to the following guidelines:
Considerations Affecting Future Dental Health
Improper preparation of a tooth may have an adverse effect on long-term dental health. For example, insufficient axial reduction inevitably results in overcontoured restorations that hamper plaque control. This may cause periodontal disease23 or dental caries. Alternatively, inadequate occlusal reduction may result in poor form and subsequent occlusal dysfunction. Poor choice of margin location, such as in the area of occlusal contact, may cause chipping of enamel or cusp fracture.
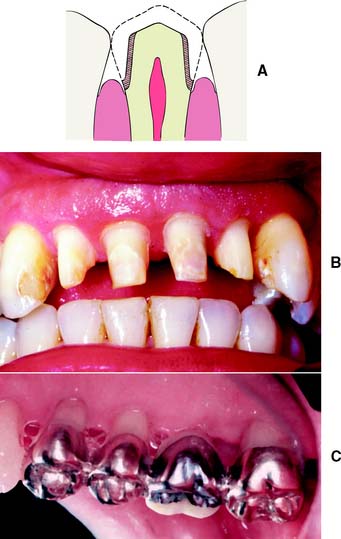
Axial reduction
Gingival inflammation is commonly associated with crowns and fixed dental prosthetic abutments that have excessive axial contours, probably because it is more difficult for the patient to maintain plaque control around the gingival margin24 (Fig. 7-15). A tooth preparation must provide sufficient space for the development of good axial contours. This enables the junction between the restoration and the tooth to be smooth and free of any ledges or abrupt changes in direction.
Under most circumstances, a crown should duplicate the contours and profile of the original tooth (unless the restoration is needed to correct a malformed or malpositioned tooth). If an error is made, a slightly undercontoured flat restoration is better because it is easier to keep free of plaque; however, increasing proximal contour on anterior crowns to maintain the interproximal papilla25 (see Chapter 5) may be beneficial. Sufficient tooth structure must be removed to allow the development of correctly formed axial contours (Fig. 7-16), particularly in the interproximal and furcation areas of posterior teeth, where periodontal disease often progresses with serious consequences.
Margin placement
Whenever possible, the margin of the preparation should be supragingival. Subgingival margins of cemented restorations have been identified26–31 as a major etiologic factor in periodontal disease, particularly where they encroach on the epithelial attachment (see Chapter 5). Supragingival margins are easier to prepare accurately without trauma to the soft tissues. They can usually also be situated on hard enamel, whereas subgingival margins are often on dentin or cementum.
Other advantages of supragingival margins include the following:
A subgingival margin (Fig. 7-17), however, is justified if any of the following pertain:
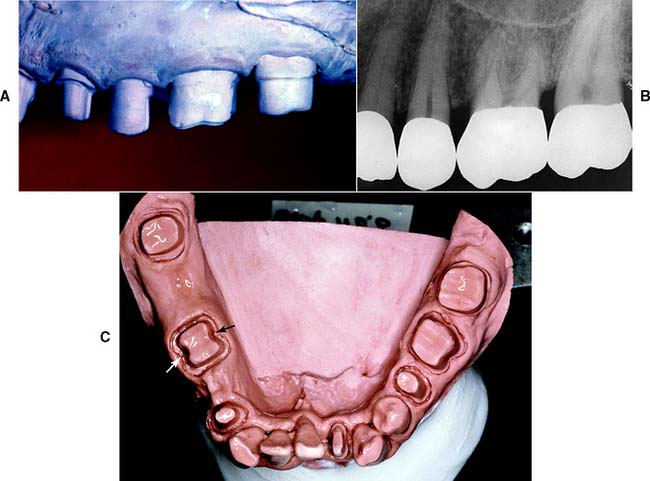
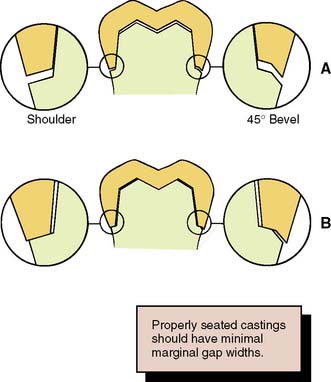
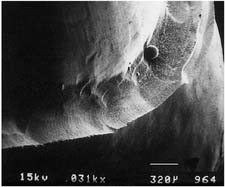
Margin adaptation
The junction between a cemented restoration and the tooth is always a potential site for recurrent caries because of dissolution of the luting agent and inherent roughness. The more accurately the restoration is adapted to the tooth, the lesser is the chance of recurrent caries or periodontal disease.32 Although a precise calculation for acceptable margin adaptation is not available, a skilled technician can routinely make castings that fit to within 10 μm33 and a porcelain margin that fits to within 50 μm,34 provided the tooth is properly prepared. A well-designed preparation has a smooth and even margin. Rough, irregular, or “stepped” junctions greatly increase overall margin length and substantially reduce the adaptation accuracy of the restoration (Fig. 7-18). The clinical significance of preparing smooth margins cannot be overemphasized. Time spent obtaining a smooth margin makes the subsequent steps of tissue displacement, impression making, die formation, waxing, and finishing much easier and ultimately results in a longer-lasting restoration.
Margin geometry
The cross-sectional configuration of the margin has been the subject of much analysis and debate.35–42 Different shapes have been described and advocated.43,44 For evaluation, the following guidelines for margin design should be considered:
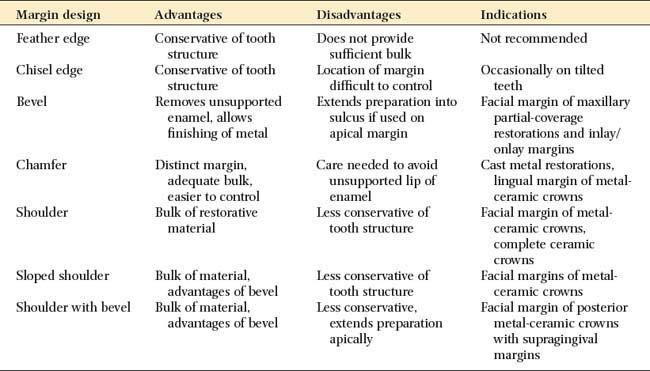
Proposed margin designs are presented in Table 7-2.
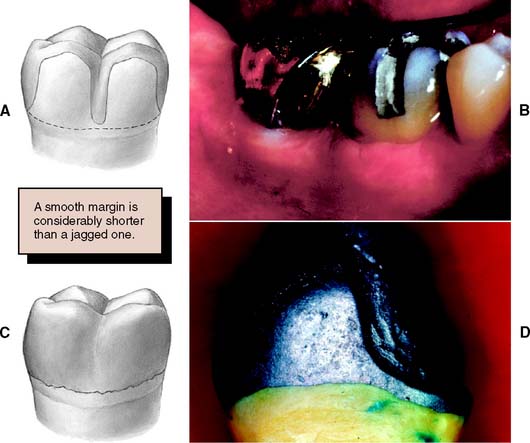
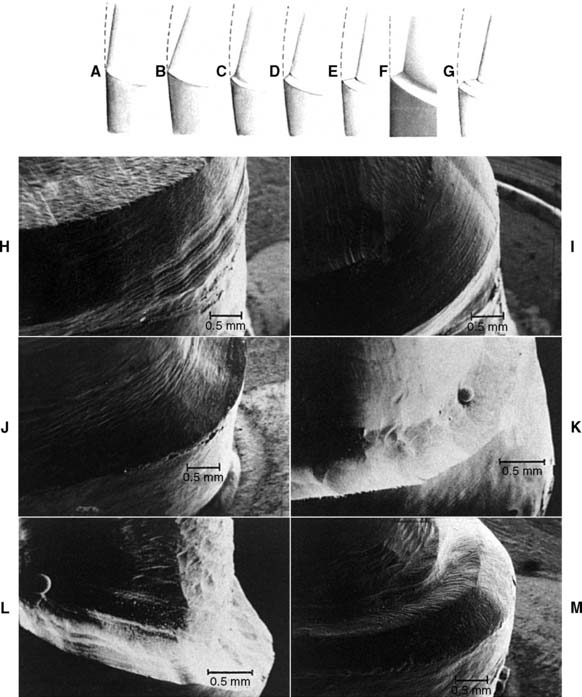
Although they are conservative of tooth structure, feather edge or shoulderless crown preparations (Fig. 7-19A) should be avoided because they do not provide adequate bulk at the margins. Overcontoured restorations often result from feather edge margins because the technician can handle the wax pattern without distortion only by increasing its bulk beyond the original contours. A variation of the feather edge, the chisel edge margin (Fig. 7-19B), is formed when there is a larger angle between the axial surfaces and the unprepared tooth structure. Unfortunately, this margin is frequently associated with preparations with excessive angles of convergence (taper) and preparations in which the orientation of the axial reduction is not correctly aligned with the long axis of the tooth.
Under most circumstances, feather edges and chisel edges are unacceptable. Historically, their main advantage was that they facilitated impression making with rigid modeling compound in copper bands (a technique rarely used today). They were useful for that purpose, because there was no ledge on which a band could catch. A chamfer margin (Fig. 7-19C) is particularly suitable for cast metal crowns and the metal-only portion of metal-ceramic crowns (Fig. 7-20). It is distinct and easily identified, and it provides room for adequate bulk of material and development of anatomically correct axial contours. Chamfers can be placed expediently and with precision, although care is needed to avoid leaving a ledge of unsupported enamel.
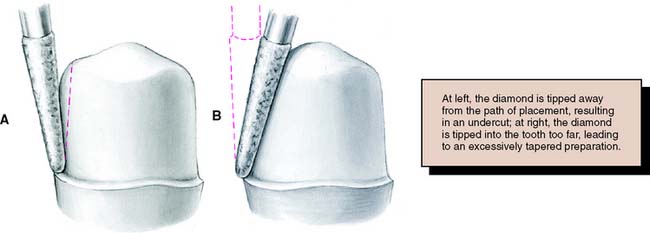
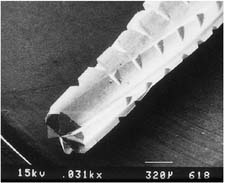
Probably the most suitable instrument for making a chamfer margin is the tapered diamond with a rounded tip; the resulting margin is the exact image of the instrument (Fig. 7-21). Marginal accuracy depends on having a high-quality diamond and a true-running handpiece. The gingival margin is prepared with the diamond held precisely in the intended path of placement of the restoration (Fig. 7-22).
Tilting it away from the tooth will create an undercut, whereas angling it toward the tooth will lead to overreduction and loss of retention. The chamfer should never be prepared wider than half the tip of the diamond; otherwise, an unsupported lip of enamel may result (Fig. 7-23). Some authorities have recommended the use of a diamond with a noncutting guide tip to aid accurate chamfer placement.45 However, such guides have been shown to damage tooth structure beyond the intended preparation margin.46
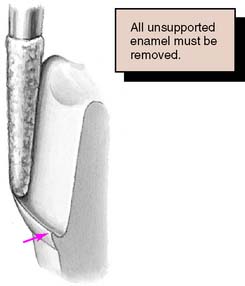
Under some circumstances a beveled margin (see Fig. 7-19D) is more suitable for cast restorations, particularly if a ledge or shoulder already exists, possibly as a result of dental caries, cervical erosion, or a previous restoration. The objective in beveling is threefold: (1) to allow the cast metal margin to be bent or burnished against the prepared tooth structure; (2) to minimize the marginal discrepancy35 caused by a complete crown that fails to seat completely (however, Pascoe40 showed that when an oversized crown is considered, the discrepancy is increased rather than decreased [Fig. 7-24]); and (3) to protect the unprepared tooth structure from chipping (e.g., by removing unsupported enamel). NOTE: when access for burnishing is limited, there is little advantage in beveling. This applies particularly to a gingival margin, where beveling would lead to subgingival extension of the preparation or placement of the margin on dentin rather than on enamel. Facial margins of maxillary partial-coverage restorations should be beveled to eliminate all unsupported enamel, to protect the remaining tooth structure from fracture, and to allow for burnishing of the casting.
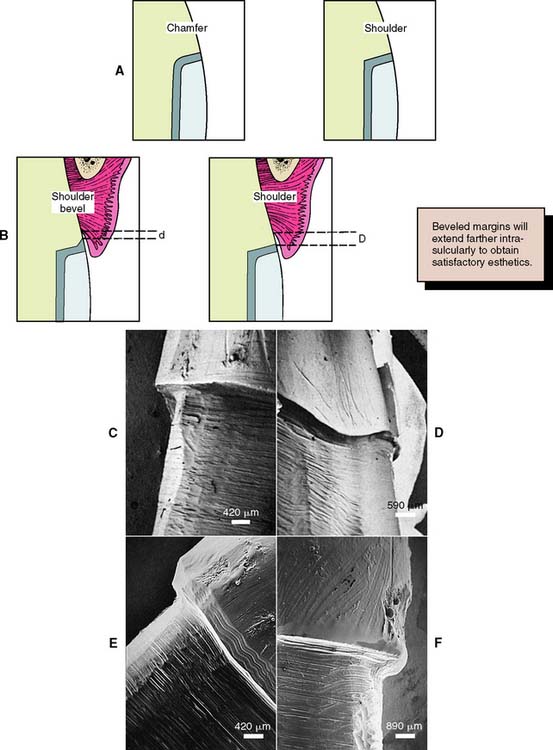
Because a shoulder margin (Fig. 7-19E) allows room for porcelain, it is recommended for the facial part of metal-ceramic crowns, especially when the porcelain margin technique is used. It should form a 90-degree angle with the unprepared tooth surface. An acute angle is likely to chip (Fig. 7-25A). In practice, dentists tend to underprepare the facial shoulder,47 which leads to restorations with inferior esthetics or poor axial contour.
Some authorities48 have recommended a heavy chamfer rather than a shoulder margin, and some find a chamfer easier to prepare with precision. Earlier workers38,39 found less distortion of the metal framework during porcelain application with a shoulder margin, although with modern alloys, these results could not be replicated.49–52
A 120-degree sloped shoulder margin (Fig. 7-19F) is sometimes used as an alternative to the 90-degree shoulder for the facial margin of metal-ceramic crowns. The sloped shoulder reduces the possibility of leaving unsupported enamel but leaves sufficient bulk to allow thinning of the metal framework to a knife-edge for acceptable esthetics.
A beveled shoulder margin (Fig. 7-19G) is recommended by some authorities for the facial surface of a metal-ceramic restoration in which a metal collar (as opposed to a porcelain labial margin) is used. The beveling removes unsupported enamel and may allow some finishing of the metal. However, a shoulder or sloped shoulder is preferred for biologic and esthetic reasons. This allows improved esthetics because the metal margin can be thinned to a knife edge and hidden in the sulcus without the need for positioning the margin closer to the epithelial attachment (Fig. 7-25B). Table 7-3 illustrates chamfer and shoulder preparations obtained with selected instruments.
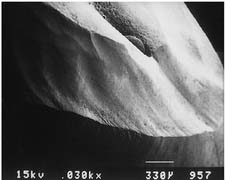
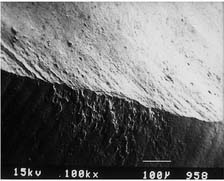
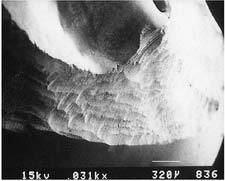
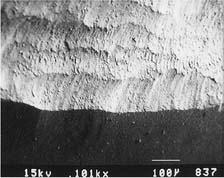
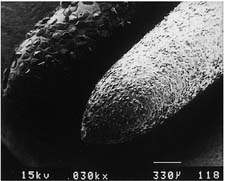
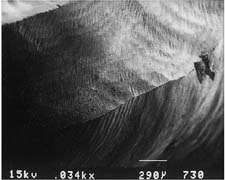
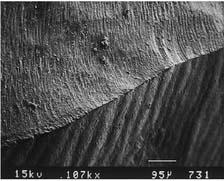
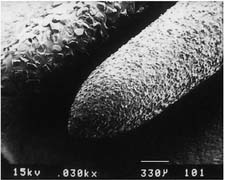
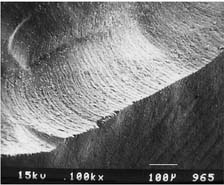
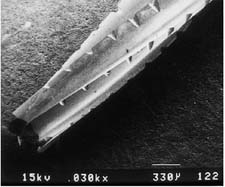
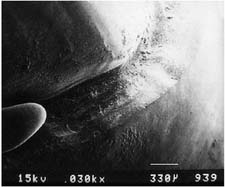
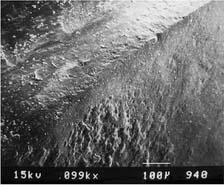
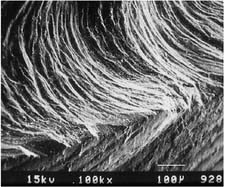
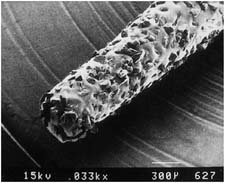
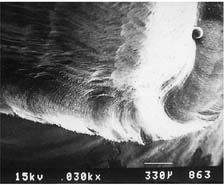
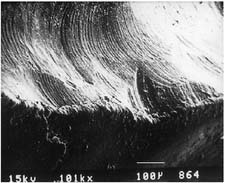
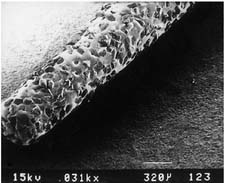
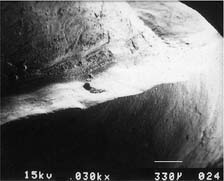
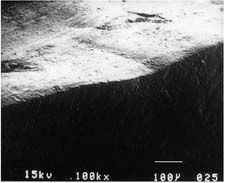
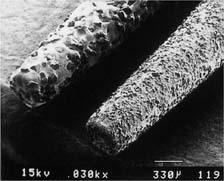
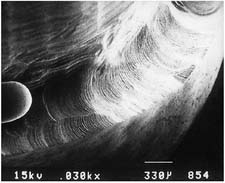
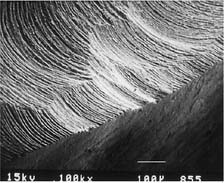
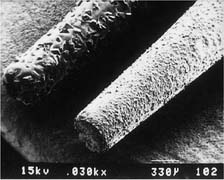
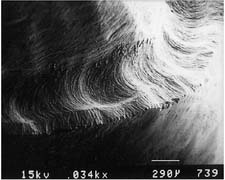
| Bur appearance | Low magnification of the prepared margin | High magnification of the prepared margin |
|---|---|---|
| CHAMFERS | ||
| Chamfer carbide (high speed) | ||
 |
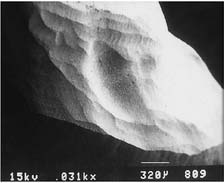 |
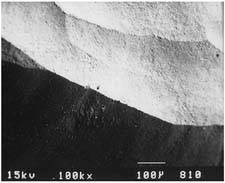 |
| Chamfer carbide (high speed) | ||
| Finishing carbide (high speed) | ||
 |
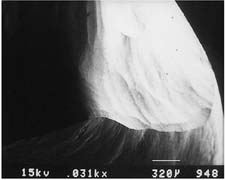 |
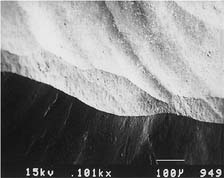 |
| Chamfer carbide (high speed) | ||
| Finishing carbide (low speed) | ||
 |
 |
 |
| Chamfer diamond coarse (high speed) | ||
 |
 |
 |
| Chamfer diamond coarse (high speed) | ||
| Fine diamond (high speed) | ||
 |
 |
 |
| Chamfer diamond coarse (high speed) | ||
| Chamfer diamond fine (low speed) | ||
 |
 |
 |
| SHOULDERS | ||
| Cross-cut fissure (high speed) | ||
 |
 |
 |
| Cross-cut fissure (high speed) and hoe | ||
 |
 |
 |
| Cross-cut fissure carbide (high speed) | ||
| Finishing carbide (high speed) | ||
 |
 |
 |
| Cross-cut fissure carbide (high speed) | ||
| Finishing carbide (low speed) | ||
 |
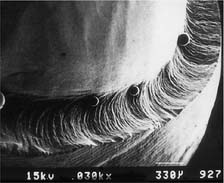 |
 |
| Flat-end coarse diamond (high speed) | ||
 |
 |
 |
| Flat-end coarse diamond (high speed) and hoe | ||
 |
 |
 |
| Flat-end coarse diamond (high speed) | ||
| Fine grit diamond (high speed) | ||
 |
 |
 |
| Flat-end coarse diamond (high speed) | ||
| Fine grit diamond (low speed) | ||
 |
 |
 |
Courtesy of Dr. H. Lin.
A comprehensive 2001 literature review of current scientific knowledge on complete coverage tooth preparations suggests that margin design selection should be based on the type of crown, applicable esthetic requirements, ease of formation, and operator experience. Research has not validated the expectation of enhanced fit being associated with selection of certain types of finish line geometry.53
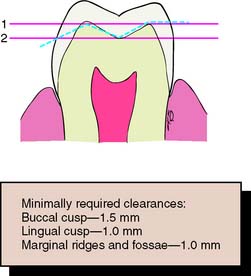
Occlusal considerations
A satisfactory tooth preparation allows sufficient space for developing a functional occlusal scheme in the finished restoration. Sometimes the patient’s occlusion is disrupted by supraerupted or tilted teeth (Fig. 7-26). When these teeth are prepared for restoration, the eventual occlusal plane must be carefully analyzed and the teeth reduced accordingly. Considerable reduction is often needed to compensate for the supraeruption of abutment teeth. In turn, this may shorten tooth preparation axial wall height, with associated mechanical consequences such as reduced retention and resistance (see p. 226).
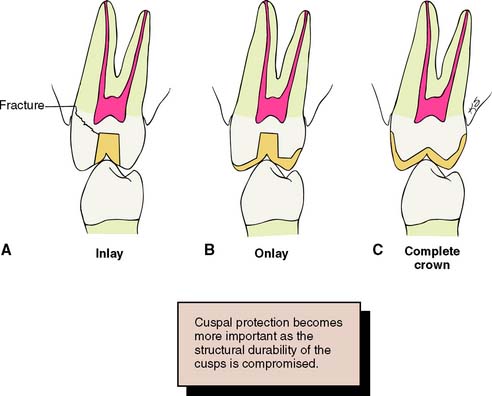
Preventing tooth fracture
The likelihood that a restored tooth will fracture can be lessened if the tooth preparation is designed to minimize potentially destructive stresses (Fig. 7-27). For example, an intracoronal cast restoration (inlay) has a greater potential for fracture because when occlusal forces are applied to the restoration, it tends to wedge opposing walls of the tooth apart. This wedging must be resisted by the remaining tooth structure; if the remaining tooth structure is thin (as with a wide preparation isthmus), the tooth may fracture during function. Providing a cuspal coverage restoration (onlay) rather than an inlay lessens the chance of such fracture.54 However, although not as conservative of tooth structure, a complete crown is often a better solution, because it offers the greatest protection against tooth fracture, tending to “hold” the cusps of the tooth together.
MECHANICAL CONSIDERATIONS
Mechanical considerations can be divided into three categories:
Retention Form
Certain forces (e.g., when the jaws are moved apart after biting on very sticky food) act on a cemented restoration in the same direction as the path of placement. The quality of a preparation that prevents the restoration from becoming dislodged by such forces parallel to the path of placement is known as retention. Only dental caries and porcelain failure outrank lack of retention as a cause of failure of crowns and fixed dental prostheses.55,56
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses